I have recently achieved (previously unattainable) control in some of my chronic pain subjects using recent innovations – but to acheive this required use of multiple modalities at once.
Recently, some of my patients are saying they don’t need working on anymore – something that takes my breath away. How was that achieved? – It took multiple agents at once and those that want to try one thing at a time will never achieve this… It takes a combination that I call “critical mass”. In nuclear terms this is the smallest amount of nuclear material to sustain a nuclear reaction – for a fire this would be the critical amount of heat needed to start a fire. For a pain sufferer it is a combination of 3-5 things that together make a substantial difference. What things helped get patients to that level include:
0) Treat Deficiencies – Check Free androgen Index for any Testosterone deficiency and treat. Also check and treat any B12 and Vit D deficiency but more on that later. Male hormone deficiency is almost universally present as any sleep apnea and chronic opioid use both can lower it. In a Cross-Sex hormone administration study, 55% of women got rid of their pain by becoming men though doses there are much higher than just replacement.
Pain. 2007 Nov;132 Suppl 1:S60-7.
Cross-sex hormone administration changes pain in transsexual women and men.
Aloisi AM et al
http://www.ncbi.nlm.nih.gov/pubmed/17379410
In women that means taking testim 0.2 – 0.3 mls/day (measure with 1cc syringe without needle first time then put same amount subsequent) or taking andriol 40 mg eod (results no way near as good). In older men, testoterone replacement was subject to a FDA warning 2014 as replacement increases heart disease risks 30% so maybe not such a great idea in older men or high heart risk patients.
1) Treat any Mood Disorder – This does not mean they don’t have pain – it means they suffer more. 1/4 fibromyalgia subjects will have a positive mood disorder questionnaire implicating Bipolar.
Wilke, William S., Carmen E. Gota, and David J. Muzina.
Fibromyalgia and bipolar disorder: a potential problem?.
Bipolar disorders 12.5 (2010): 514-520.
http://www.ncbi.nlm.nih.gov/pubmed/20712752
A recent metanalysis pegged it at 20%:
Kudlow, P. A., et al.
Prevalence of fibromyalgia and co-morbid bipolar disorder: A systematic review and meta-analysis.
Journal of affective disorders 188 (2015): 134-142.
http://www.researchgate.net/profile/Paul_Kudlow/publication/281712395_Prevalence_of_fibromyalgia_and_co-morbid_bipolar_disorder_A_systematic_review_and_meta-analysis/links/56022f1f08aeb30ba7355af7.pdf
Seeing as I see the worst, they are represented. I tell them that this “softens” the brain(damages) and makes such pains felt at full volume.
In this subgroup, many can remember never being happy rather than having periods of hypomania. People with chronic pain, lack of sleep, and poverty may not get a happy phase or go on sprees. They will however, perhaps remember a turbulent youth where they may have left home early, gone through a dark phase with drugs, and failed school. They may also notice that antidepressants alone either fail or put then into an agitated state. Typically they are much more likely to has spells of a mixed state – more agitated, can’t sleep, can’t think, and angry. These can be horrible and can worse than their pain. Asking them to explain how in their youth they went from being happy to very sad in one day or visa versa (rapid cycling in adolescence) might help get their attention. Some have never had a good sleep. Family history, suicide ideation or attempts, and prior hospital admissions clinches the diagnosis. ADHD features are common. Being put on mood stabilizers with antidepressants, helps then get happier for the first time in a long time.
Problem is, there children are probably also affected and probably have ADHD or a turbulent youth. Parents (I see more mothers) may not get better until you treat them too. I start with quetiapine 25 mg which helps them sleep and cuts any agitation but finding a right combo will be a challenge and the do best on 3rd generation antidepressant agents (Pristiq, Cipralex) though Duloxetine(Cymbalta) would be better. This is plus either atypical antipychotics and/or lamotrigine. Unfortunately, with multiple chemical sensitivity represented, trying Lamotrigine could result in a dangerous rash but when tolerated helps pain and depression. It does not control the mixed states and require atypical antipsychotics to prevent that – Have seen some of mine go thru problems this spring but they have settled now.
Now it looks like bipolar inherited from mom in some cases could be a mitochondrial disease that responds some to weight loss and metformin:
Fibromyalgia (FM) – Mitochondrial Dysfunction Helped by Metformin and Weight Loss
http://painmuse.org/?p=4468
Metformin is Mitochondrial Enhancer and Helps Bipolar Depression
http://painmuse.org/?p=4480
Another mitochondrial stimulant is Coenzyme Q10 and it is found to help some cases of Fibromyalgia – I bet the more inherited mitochondrial form:
Antioxid Redox Signal. 2013 Oct 20;19(12):1356-61.
Can coenzyme q10 improve clinical and molecular parameters in fibromyalgia?
Cordero MD(1), Alcocer-Gómez E, de Miguel M, Culic O, Carrión AM, Alvarez-Suarez JM, Bullón P, Battino M, Fernández-Rodríguez A, Sánchez-Alcazar JA.
http://online.liebertpub.com/doi/abs/10.1089/ars.2013.5260
- 100 mg three times daily cut pain by 1/2 in 40 days
Recent metanalysis found Olanzepine helpful in chronic pain :
Adding an Antipsychotic Helps Treat Pain (only olazepine)
http://www.medscape.com/viewarticle/859160
also:
http://www.ncbi.nlm.nih.gov/pubmed/16379502
http://www.ncbi.nlm.nih.gov/pubmed/14622714
http://www.ncbi.nlm.nih.gov/pubmed/11997204
2) Gluten question – Consider gluten sensitivity if you have and irritable bowel and try avoiding gluten for extended period. There is a new gluten sensitivity disease (non-celiac gluten sensitivityUNDIAGNOSABLE by usual testing ( blood test and villous atrophy on biopsy) that is well associated with chronic Fibromyalgia pains.
New Help for Some Fibromyalgia (FM) – Gluten Sensitivity Management
http://painmuse.org/?p=4330
In fact 1/3 Fibromyaglia subjects with more diarrhea IBS will be pain free after 6 months of a gluten free diet – and remember gluten sufferers often react to dairy and egg so must look out for those too.
If found to have celiac, may have deficiencies of:
B12 – measure but 1000+u/day prudent.
B6 – take 100 mg/day (no more though as 400+ mg/day can cause neuropathy)
Vitamin E – take 100 unit/day – no more as 400/day might increase stroke rate
Iron – could be associated with restless legs and may require intermittent IV infusions to keep levels up if iron supplementation not work though effectiveness is controversial.
3) Vitamin D – Start on 4000 u/day as recently found to help:
Vitamin D – Could High Doses Help Pains?
http://painmuse.org/?p=4168
High dose vitamin D found to significantly reduce irritable bowel symptoms as well:
Neurogastroenterol Motil. 2016 Oct;28(10):1533-44. doi: 10.1111/nmo.12851.
Effect of vitamin D on gastrointestinal symptoms and health-related quality of life in irritable bowel syndrome patients: a randomized double-blind clinical trial.
Abbasnezhad A et al
https://www.ncbi.nlm.nih.gov/pubmed/27154424
They used 50,000 units D3 every 2 weeks. I use 50,000 units weekly of D2 (Osto- D2)
Try Herbal Palmitoylethanolamide (PEA) – recent metanalysis shows it significantly helps pain – especially neuropathic pain:
Pain Physician. 2016 Feb;19(2):11-24.
Palmitoylethanolamide, a Special Food for Medical Purposes, in the Treatment of Chronic Pain: A Pooled Data Meta-analysis.
Paladini A et al
https://www.ncbi.nlm.nih.gov/pubmed/26815246
Though many studies used 800 mg /day or less, a recent study site is using 600 mg twice daily. You can get PEA off ebay, but in Canada it’s best sent C/O your doctor’s office as it may not make it past customs otherwise.
5) Take Testosterone – a patent study found a significant decrease in pain:
) Finding an opioid that the patient can tolerate – not always easy. Had one patient that refused meds for years because couldn’t stomach anything (and you cannot start fentanyl patch without them being on an opioid first) that did marvelously on BuTrans patch. For elderly is useful at the 5 mcg starter, though might want to leave half the backing on to start, and tape down with Hypafix. Had one elderly case tolerate 5 mcg well but then get very sick when taken to the 10 mcg.
I wrote about it here:
7 day Buprenorphine Patch Lanched in Canada http://painmuse.org/?p=343
5) Try spironolactone 100 – 200 mg but give it 6 weeks. Recently found to dramatically improve 1/2 of Fibromyalgia cases. I have found initial tolerance an issue and suggest start with 25 mg and work up. Remember can elevate potassium.
http://painmuse.org/?p=4054
6) Switching subjects to arthritis med Flurbiprofen – suggested by Dr Jean Gillies, a rheumatologist in Vancouver, as being more effective in certain rheumatologic conditions. For ankylosing spondylitis, a condition that remains subclinical in some resistant pain cases, it was effective in 90% at 100 mg twice daily: (can go to 300 mg/day). If that means taking a PPI with it, it still might be worth it:
Good, Armin, and Hector Mena.
Treatment of ankylosing spondylitis with flurbiprofen and indomethacin.
Current Medical Research and Opinion 5, no. 1 (1977): 117-121.
http://www.ncbi.nlm.nih.gov/pubmed/71969
Recently an article was published on the right handed version of Flurbiprofen. They stated it had “anti-inflammatory, endocannabinoid-modulating and antioxidative properties”
EMBO Mol Med. 2014 Sep [Epub ahead of print]
R-flurbiprofen attenuates experimental autoimmune encephalomyelitis in mice.
Schmitz K et al
http://www.ncbi.nlm.nih.gov/pubmed/25269445
7) B12 shots – my daughter, Janice Montbriand, and I did a case study report on 26 cases taking B12 shots and found it uniformily helpful in neuropathic pains – protocol was to take it 1000 mcg daily for 14 days then every 1-3 days therafter depending on how fast pains return. This was presented at the Canadian Pain Society 2013 as a poster. I wrote about the two randomized double blind trials that showed benefit here:
Chronic Back Pain Help – Forgotten B12 Injections and What Else Good For… http://painmuse.org/?p=1543
There is also literature about using B12 in shoulder bursitis but results were recorded after 6 weeks so suspect anti-inflammatory properties take longer that 2 weeks.
8) Human Chorionic Gonadotrophin (HCG) shots – Saw presentations by a Dr. Tennant where he found subjects on reduced opioid needs by 20-100%. I wrote about it here:
Human Chorionic Gonadotrophin (HCG) Touted as Only Curative Agent For Pain That Has Centralized http://painmuse.org/?p=2958. My experience is that it can drop pain by 2/10 which is alot for many… The B12 and HCG can be injected subcut in same 3 ml syringe ( 2 ml total). Some of HCG’s effect is through increasing androgen levels and I’ve had some older cases just respond to being put on testosterone (testim 0.2 ml/day for women)
Dr. Tennant has a series of websites discussing HCG and hormones:
Websites:
www.foresttennant.com
www.hormonesandpaincare.com
www.intractablepaindisease.com
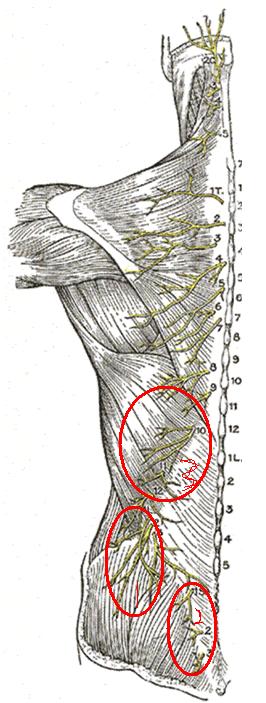
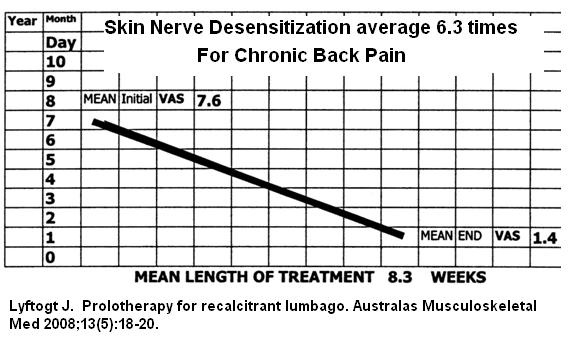
9) 5% dextrose injected above sensitized skin nerves – originally called “neural prolotherapy” because concentrated sugar was initially used – now perineural injection therapy. Part of any regional pain is the sensitization of the skin over the area involved. Merely injecting a bleb of D5W every 1 cm along the course of tender cutaneous nerves has remarkable benefits.
Lyftogt J.
Prolotherapy for recalcitrant lumbago.
Australas Musculoskeletal Med 2008;13(5):18-20.
https://www.researchgate.net/profile/John-Lyftogt/publication/284665969_Prolotherapy_for_recalcitrant_lumbago/links/5e9cd1aa92851c2f52b27ad7/Prolotherapy-for-recalcitrant-lumbago.pdf
Injected subjects an average 6.2 times (2-16) over average 8.3 weeks (1-1& weeks)
Injected Superior cluneal, medial cluneal and thoracic cutaneous nerves.
Results were breathtaking – start at 7.6/10 and end up with 1.4/10. I had sceptics ( I was to start)who were amazed by next visit. I add 3% glycerin to the D5W ( as suggested by a Dr. Rosen) and it makes it last longer. Does take some concentration to feel the nerves but the skin sensitivity helps guide you. Had patients shortly say they were so much better they didn’t need any more treatment in some cases.
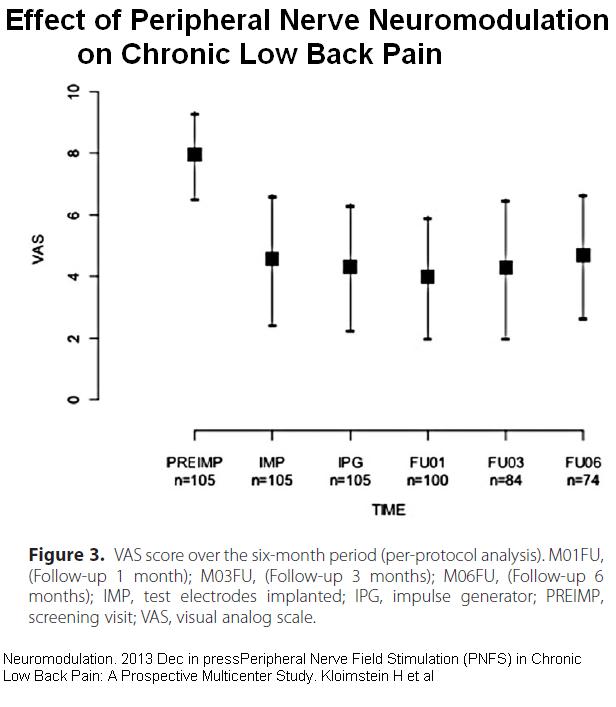
Don’t think the skin can be that important?- well think again – in chronic back pain, a whole new procedure has been developed for implanting peripheral nerves with nerve stimulator leads:
Neuromodulation. 2013 Dec 9. doi: 10.1111/ner.12139. [Epub ahead of print]
Peripheral Nerve Field Stimulation (PNFS) in Chronic Low Back Pain: A Prospective Multicenter Study.
Kloimstein H, Likar R, Kern M, Neuhold J, Cada M, Loinig N, Ilias W, Freundl B, Binder H, Wolf A, Dorn C, Mozes-Balla EM, Stein R, Lappe I, Sator-Katzenschlager S.
Results:
10) Brutal transverse stretch massage:
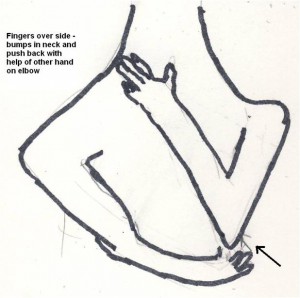
for shoulder tips as follows: –
- put finger tips just in front of side bumps(transverse processes) at base of neck.
- Press down and sweep fingers backwards catching levator scapula muscle as do.
- Once resistance is encountered, force it gradually back through tight levator scap and trapezius tip muscles.
- Best done lying down.
- Burns like crazy and takes 5-10 minutes to release.
- Once more relaxed, massage back and forth over it until nontender.
- Can do it yourself by putting your fingers just in front of side buts and sweeping back at base of neck.
- You can reinforce with opposite hand on elbow:
 People are uniformly amazed when they can now turn their head almost fully to the side done.
People are uniformly amazed when they can now turn their head almost fully to the side done.
I have now found thumping repeatedly with my activator in direction I’m transverse massaging can get near instant release if done 10 -20 times. – shoulder tip, groin tendons etc
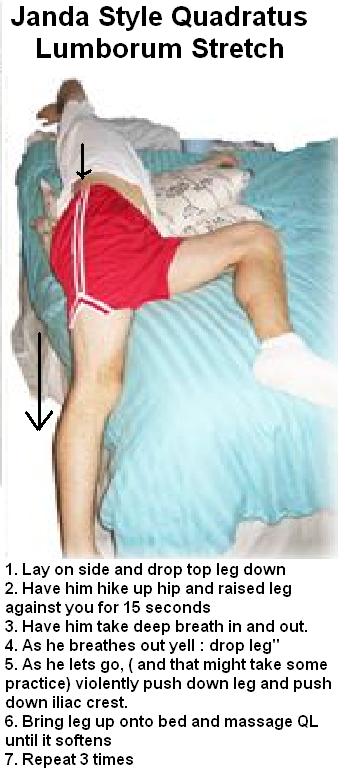
Quadratus lumborum and Abdominal Oblique with cluneal – discussed here: Back Pain Worsening? – Look For Back Pain Multipliers – They Are Treatable. http://painmuse.org/?p=2924
now not only do I use ther finger cover to press on the Quadratus lumborum front and back, I have a vibrator that has a probe like end that I can dig into quadratus lumborum muscle and work over 15 minutes to free up.
I use a Janda style stretch to push leg down (after patient uses it pushing up for 15 second and relaxes) – three times to stretch QL.
For the deep quadratus lumborum, the body needs to be twisted and in this position a superficial band of the abdominal oblique comes into focus and needs to be stretched as well – push down on band that appears until softens and then rub out – will burn like crazy and the patient will not be happy until after… I can feel very tight wirelike tender strings I feel are the cluneal nerves coursing thru and when they are stretched people feel much better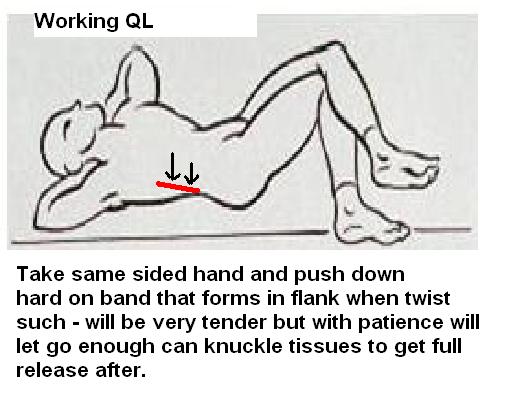
Once the QL is relaxed, painful areas in buttock and side of hip disappear – referral is more than just referred pain – it knots up the muscles in the referral areas as well!
For piriformis I use a 15 minute transverse stretch that I have discussed here:
Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica? http://painmuse.org/?p=1891 and How Should One Investigate Chronic Back Pain and What about the Back Muscles? http://painmuse.org/?p=57
It involves the following:
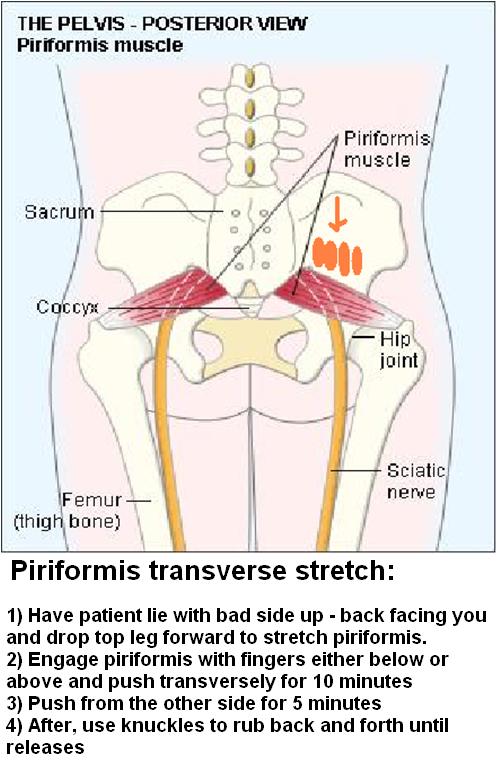
I do it because I can’t get physios or massage to do it – They say it’s too hard but I think it’s just too much work… Results are dramatic and patients who have been painful for years finally get to see what it is like to be better. Needs to be done 2-3 times a week and even then only gets 60-70% better. Botox works here but is expensive. For those that are unduly sore to start, I will inject piriformis with steroid; but that does not decrease need for loosening up.
I have now found transverse stretching with the help of an “Activator” – Thumping apparatus used in chiropractics – remarkably releases bands (over 20+ thumps then massage, then thump transverse stretch again etc…)
11) Ketamine shots. For people with constant pain 7/10 or over I will offer biweekly ketamine injections. This is based on a poster presentation:
INTRAMUSCULAR (IM) KETAMINE FOR TREATING MIGRAINE AND NEUROPATHIC PAIN IN THE CLINIC – they used 0.3 – 0.4 mg/kg in divided doses.
http://www.anodyneheadachepain.com/Research/APS4.pdf
If too much is given at once, a very uncomfortable depresonalization reaction can occur but I have never seen it with the 10 mg every 15 min X 2 protocol that I use. No bladder issues either. A reliable partner can eventually give it once they have proven stable at office. Ketamine has remarkable anti-depressant effects and people say part of the relief is that they no longer care they are in pain for a few days. Often relieved depression within 30 minutes and totally removes suicidality.
12) Pamidronate infusions 90 mg (less in older with reduced renal clearance) every month can reduce mechanical back pain, sciatica, spinal stenosis and vertebral fracture pains by 40%. Unfortunately the infusion takes 4 hours and people feel worse for up to a week. It has made some untreatable cases now respond to measures mentioned above.
wrote about here:|
Chronic Back Pain May Be a Pamidronate Infusion Treatable Disease – And Why Did It take 10 Years to Replicate That? http://painmuse.org/?p=3002
13) Getting sleep studies on my subjects and using CPAP when needed; treating restless legs.
14) 5% semineurolytic LIDOCAINE – injected into discrete triggers or spastic areas that are unduly tender where I suspect there is micorentrapment of nerves in muscle. Sometimes takes 2-3 times to make it take spaced 5-7 days apart. Most adults manage 2cc without difficulty – older 1-1.5 mls. Have one subject who was previously bedridden – have ketamine shots twice weekly and injection into his most tender points of the day – he is now working over 1/2 time. Adding 3% glycerin to the 5% lidocaine makes it work better. Have one lady with occipital neuralgia with real “zingers” – I botox the nerves and tender skin areas, and subsequently inject any tender occipital with 5% lidocaine. The latter used to take several shots. Now that I’ve added the 3% glycerin – one shot is sufficient.
15) Prolotherapy – injecting spinal ligaments to tighten up the structures and make more stable – I have used 17% dextrose but find it unduly painful (College does not like injecting local around spine outside hospital setting). I am starting to use dilute testosterone without local instead which is something worked out by a Dr. Tom Ravin, who gave a presentation and examples at a recent CAOM metting. He wrote about it here ( though I do not use the growth hormone part):
http://www.journalofprolotherapy.com/pdfs/issue_08/issue_08_07_testosterone_growth_hormone.pdf
Making up aqueous testosterone is time consuming:
micronised testosterone 20 mg ( 5 mg/10ml)
D5w 38 mls
sodium bicarbonate 8.4% 1 ml
2 drops tween 80 to help suspend
autoclave
After autoclaved, add small amount of benzyl alcohol that has been passed through millipore filter.
I make smaller amount of dilute testosterone because if it is too old it won’t inject through small bore needles.
Testosterone still clumps some so actual dose might vary some – which might be a blessing because you can measure exact amount out of testosterone first time and the approximate same amount thereafter.
Does it survive autoclaving? – got acne and gynecomastia from repeated injections so am sure. I used to just use unshaken-up supernatant in women but got slight hirsuitism in one lady so now dilute 1/4 like author recommended for women.
Doing prolotherapy – not sure if as potent but subjects do feel better after facet/interspinous injections to unstable segments. For sacrum where I can use local, I use 17& dextrose in lidocaine though.
Does prolotherapy work? – Helps. – Dr. David Watson, one of our CAOM members, published a study of 190 cases using prolotherapy and found improved pain and quality of life.
Watson, John David, and Barbara L. Shay.
Treatment of chronic low-back pain: a 1-year or greater follow-up.
The Journal of Alternative and Complementary Medicine 16, no. 9 (2010): 951-958.
http://online.liebertpub.com/doi/abs/10.1089/acm.2009.0719
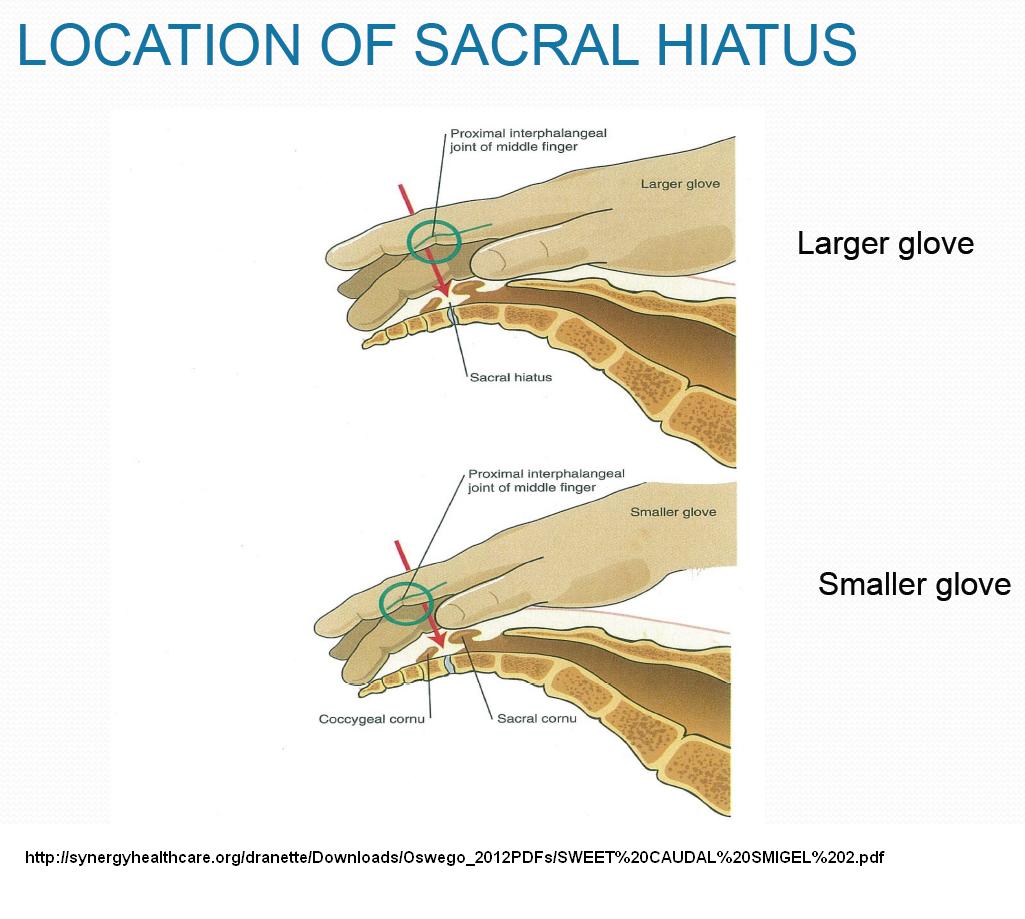
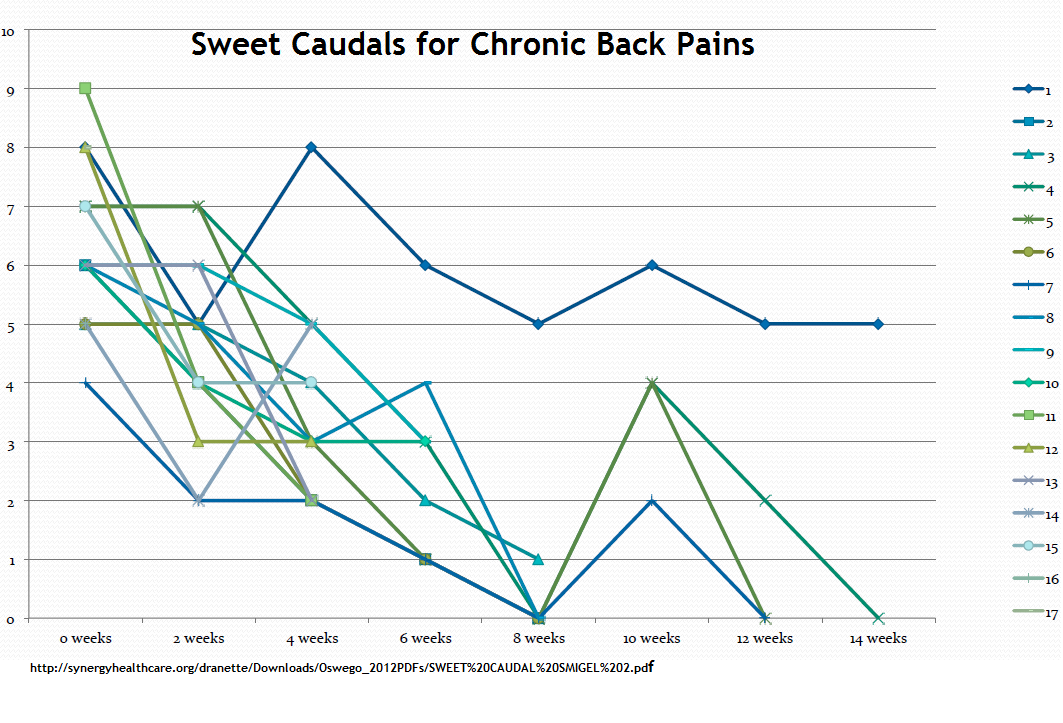
16) Sweet caudals – it is clear D5W has anesthetic effects. Lidocaine etc. is acidic (and burns) so numbs, but can’t be as good long term. Dr. Howard Rosen found just injecting 10 mls D5W caudally repeatedly can give sustained relief in both mechanical back pain and sciatica. It is undergoing controlled trials at this time. One thing that I always wondered about is – If the dura commonly comes down to 1 cm from sacral hiatus – why do you poke needle up caudal canal for caudal epidurals – Dr. Rosen thought the same and found you can inject straight down onto sacral hiatus and still get epidural spread. So he developed a simple painless caudal and allergy free injection of just D5W. There is a discussion here:
http://synergyhealthcare.org/dranette/Downloads/Oswego_2012PDFs/SWEET%20CAUDAL%20SMIGEL%202.pdf
Several points which are nicely made there and I took out incase this site goes down:
1) If you feel tip of coccyx, sacral hiatus is 2nd finger joint from tip:
2) you can get into epidual space by just injecting straight down into sacral hiatus:
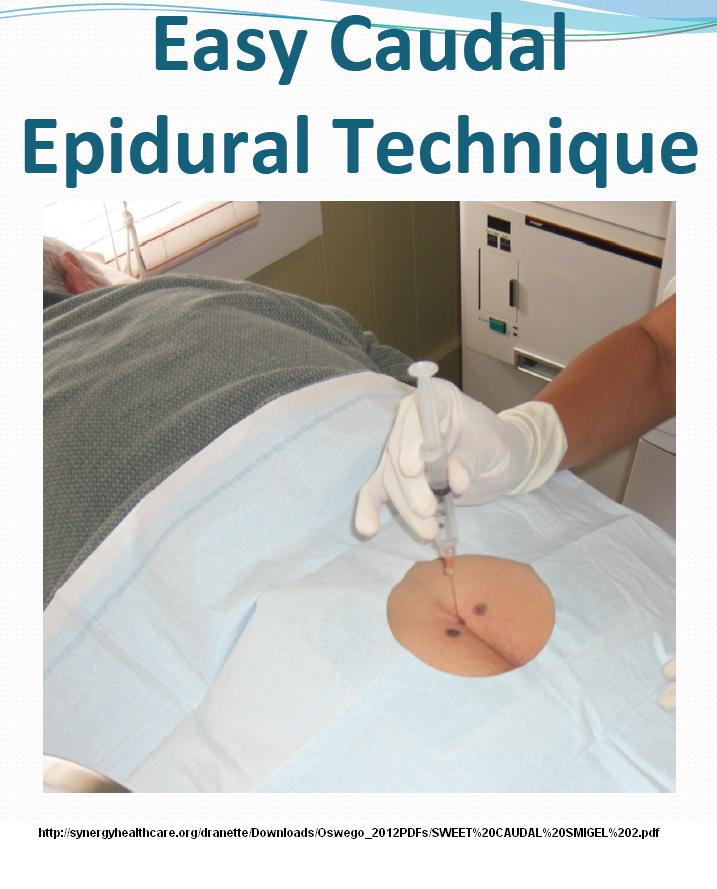 Sadly, I am still a little old fashioned, and think having it tilted a bit towards head might help it go through membrane better:
Sadly, I am still a little old fashioned, and think having it tilted a bit towards head might help it go through membrane better:
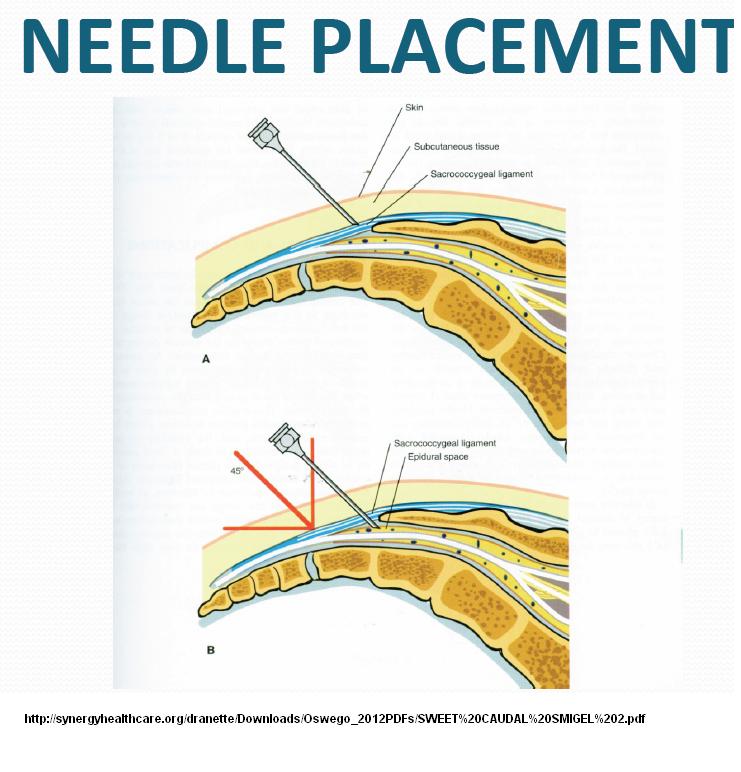
I think the key is you do not have to re-angle which just causes trouble – also the key is you must feel it go through as membrane where you can inject it. I inject local (Diluted with sodium bicarbonate 8.4% so it does not sting – If you go down with injection you can tell if you can go through membrane and if not inject elsewhere until you do then aim for same spot. (If I win a lottery I’ll buy an ultrasound machine – I had one but it was huge and I got rid of it).
Have one lady, with back pain and multiple allergies. Sweet caudals have been tolerated so far. Often there can be 90% improvement in pain shortly after injection. Long term results:
Combined with the D5W, I include B12 based on a study treating diabetic neuropathy with spinal B12:
Clin Ther. 1987;9(2):183-92.
Clinical usefulness of intrathecal injection of methylcobalamin in patients with diabetic neuropathy.
Ide H, Fujiya S, Asanuma Y, Tsuji M, Sakai H, Agishi Y
http://www.ncbi.nlm.nih.gov/pubmed/3568063
- Seven men and four women with symptomatic diabetic neuropathy were treated with methylcobalamin (2,500 micrograms in 10 ml of saline) injected intrathecally
- “Symptoms in the legs, such as paresthesia, burning pains, and heaviness, dramatically improved. The effect appeared within a few hours to one week and lasted from several months to four years.”
- They felt that oral B12 had poor absorption spinally and that seems to be the case with the need for injectable B12 mentioned earlier.
- “These findings suggest that a high concentration of methylcobalamin in spinal fluid is highly effective and safe for treating the symptoms of diabetic neuropathy.”
- This was based on two earlier positive studies but has been totally forgotten before -perhaps because it was japanese and it would be alot of effort to just inject B12 – but as a simple sweet caufdal would be easy, relatively painfree, and safe.
I have been using this in plain back pain patients and one reported (without being asked) that the shots with B12 included worked better (could be placebo though). Though earlier studies were done with 10 ml volume, I understand one of the researchers now uses a 20 ml volume.
17) Blocks – three most common I use are suprascaplar nerve blocks for persistent shoulder pains, and saphenous and obturator nerve blocks for inner leg and knee pains. When used repeatedly will gradually desensitize a pain region. I had one lady with obuturator neuropathy and early CRPS in leg from large superficial blood clots in femoral superfical veins. Repeated ketamine injections and obturator nerve blocks have removed that issue. Repeated every third day nerve blocks has been found to help resistant migraines (and I would combine that with daily ketamine shots) until some relief has been achieved.
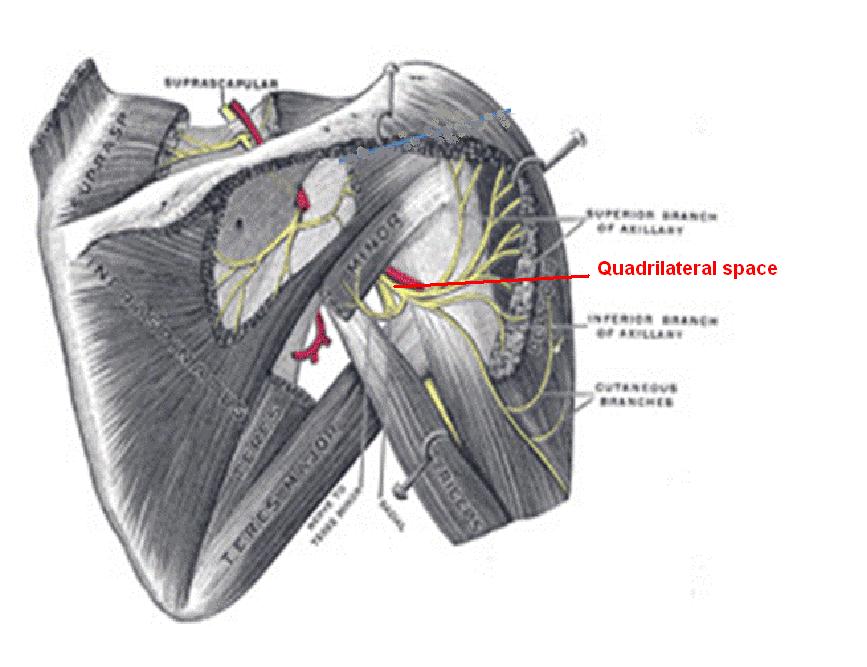
One of the things I have noticed, is that a suprascapular nerve block does not give a good block to the deltoid muscle and pain on subsequent visits seems to be related to deltoid spasm. Now I have found that injection posteriorly between teres major and minor just behind triceps in what is called the quadrilateral space will give me that deltoid relaxation and I can work out some very tight bands there:
 18) Methotrexate therapy or Prednisone for inflammatory pattern FM.
18) Methotrexate therapy or Prednisone for inflammatory pattern FM.
Fibromyalgia – Responses to Methotrexate and Steroids
http://painmuse.org/?p=4373
There is a foundation in the US that treats FM patients with low dose prednisone ( getting down to 5 mg only several times a week so minimal side effects) and claims it works well.
A pulse of dexamethasone could help determine if it is inflammatory (half will be nerve and muscle so don’t expect more). These pulses work as well as Ihttp://rheumatology.oxfordjournals.org/content/47/2/208.full.pdf+html methylprednisone and don’t kill veins:
Here is dose in CIDP:
-Use included Dexamethasome 4 mg – 4 am, 4 lunch, 2 supper = 40 mg/day – for 4 days
Pulsed high-dose dexamethasone versus standard prednisolone treatment for chronic inflammatory demyelinating polyradiculoneuropathy (PREDICT study): a double-blind, randomised, controlled trial
Ivo N van Schaik, Filip Eftimov, Pieter A van Doorn, Esther Brusse, Leonard H van den Berg , W Ludo van der Pol, Catharina G Faber, Joost CH van Oostrom , Oscar JM Vogels, Rob DM Hadden, Bert U Kleine, Anouk GW van Norden, Jan JGM Verschuuren , Marcel GW Dijkgraaf, Marinus Vermeulen
The Lancet Neurology, Volume 9, Issue 3, Pages 245 – 253, March 2010
http://www.thelancet.com/journals/laneur/article/PIIS1474-4422(10)70021-1/fulltext#article_upsell-
19) IV Gammaglobulin or Plasmaphoresis – If Fibromylagic, Diabetic or Celiac, and if some numbness – consider Chronic Demylinating Inflammatory Polyneuropathy – numbness often but not always with noticeable weakness – loss of ankle jerks and a positive EMG clinches the diagnosis. Responds to steroid pulses, gamma globulin infusions, and plasmaphoresis
Caro, X. J., Winter, E. F., & Dumas, A. J. (2008).
A subset of fibromyalgia patients have findings suggestive of chronic inflammatory demyelinating polyneuropathy and appear to respond to IVIg.
Rheumatology, 47(2), 208-211.
http://rheumatology.oxfordjournals.org/content/47/2/208.full.pdf+html
“Fifteen FMS/CIDP subjects were subsequently treated with IVIg (400 mg/kg each day for 5 days). Pain (P=0.01), tenderness (P=0.001) and strength (P=0.04) improved significantly. Fatigue and stiffness trended towards improvement.”
20) Cheap pulse frequency treatment – high frequency (radiofrequency) pulse generating machines have been recently used to render nerves silly so they will not conduct pain. They have to be very careful to watch the temperature and cut the duration short because these machines are too powerful. I just used a low frequency pointer plus starting at level 2 and working up to top 10 and pulse it for 10 minutes. Under local, I start at 20 gauge cathlon IV at site and thread a 2 inch 25 gauge needle through it. Only the tip is exposed. I then inject 5% lidocaine 0.7 ml into site before pulsing it off and on for 10 minutes manually. You can do up to 3 sites that way. The patient will feel it in the hand and will tell you when it is too much. I have used it for resistant occipital neuralgia and into a suprascapular nerve to shoulder where a lady had 10/10 CRPS pains ( dropped it to 7). Still new so don’t know how long it lasts.
21) I have some post surgical messes that nothing works and have given them marijuana. I wrote about its use here:
Canadian Marijuana Presciption Steps
http://painmuse.org/?p=4679
There are more things I use – SI joint prolotherapy or blocks, caudal intrathecal midazolam to augment steroid epidural blocks when they wear off, and so on. And let us not forget Botox except for fact it is expensive..
Putting this all together was alot of work – if you found this helpful- say so!

Nice pictures!
Gee, I thought I was aggressive!!! We must collaborate!
Very interesting, need to reread a few times and break out my medical dictionary to remember what some of those words mean
Pingback: Dispelling Myth That Chronic Pain is Unresponsive to Treatment | Pain Medical Musing
Pingback: Neuropathic Treatment Failure -The Greatest Issue In Treatment of Chronic Pain | Pain Medical Musing
Excellent article, I need to try the stretches out.
Wow – great articles – I scanned your notes but will be visiting the recommended sites. I will post the site on my website. I am on twitter and it breaks my heart to see how many people suffer and seem to have so little support.
Judy you have NO IDEA of the obscenity being foisted on sevrely injured workers by WCB and SGI. Saskatchewan is worse than a 3rd world country when significant injury and insurance interests are involved aka;WCB / SGI
The Next Election will be fought correcting these atrocities.
Judy you have NO IDEA of the obscenity being foisted on sevrely injured workers by WCB and SGI. Saskatchewan is worse than a 3rd world country when significant injury and insurance interests are involved aka;WCB / SGI
The Next Election will be fought correcting these atrocities. EXAMPLE: A certain medication prescribed for workplace injury was deliberately discontinued by WCB who “Falsified”fabricated lies to deny deny deny. When a severely injured workers physician request’s treatment “Everything possible is used to Deny, Deny, Deny; This is deliberately done by WCB to DRIVE the injured to suicide.
The Sheer amount of falsification used by WCB and their contractors is over the top. WCB employee’s make Mass Murderers look sane….