Got a recent enquiry of what to do if you are an enbrel failure. I will go over what I can.
I’m a 55 yr. old female with psoriatic arthritis, fibromyalgia and celiac disease. I am currently taking enbrel 50 mg. 2/wk, sub-q, for the psoriatic arthritis. I’ve suffered from herniated discs (L4-5 and L5-S1) and lower back pain for years. For the past year I’ve had excruciating sciatic nerve pain for which I’ve been give Lyrica, Gabapentin, local steroid shots in the buttocks, chiropractic treatment, TENS, pain creams, etc, etc. So when I learned about the spinal injections of enbrel as a treatment for sciatica, I contacted the Florida office of Dr. T… and paid (thru the nose) for one treatment. Their claim is that one shot should do the trick, at the most 2. Well, my back pain went away for a day, range of motion increased and all my numbness and tingling disappeared. However, the nerve pain down my right leg didn’t feel any relief at all. It’s been a month since that first shot and all my back pain is back, as well as the numbness and tingling, too. My nerve pain is worse than ever and they want me to have a 2nd shot.
Their fee is $460 for initial consultation and $4000 for the shot, but when I said I didn’t have that, they immediatly dropped the price to $120 for the consult and $1250 for the shot, and if I wanted the 2nd one I have window of opportunity of 4 weeks at the reduced price, othewise it jumps to the $4000 original fee.
I did it because of the pain I am having, but I will not go for the 2nd one. The whole operation was very slick and I wasn’t comfortable with the evironment.
Question: I’ve been on IV/Remicade before, would it be a good idea to switch to Remicade again to see if it helps my back and nerve pain? Do you think it’s worth a try? I’ll go thru all the insurance changes and all that if I knew it’s worth trying. What do you think?
I can’t imagine what it must be like to live like that.
Some thoughts that come to mind:
- Might not be fair to expect enbrel shots to help you if you are already on enbrel shots – I suspect the tumor necrosis factor inflammation is not as big as other inflammatory issues. Having said that ONE shot does little – 2 shots a week apart would be the minimum . Why don’t you have your regular enbrel shots just under the skin in your low back? – it could help there.
I would be more enclined myself to have steroid epidural shots:
– though 40 mg each shot might be enough – (then you could have one every 6 weeks rather than 80 mg every 3 months)
Sciatica Back Epidural or Caudal – 40 mg Steroid as Good as 80 mg– have it done by paramedian approach (needle 1 inch off to side and angled in) so needle more likely to be on right side of epidural septum:
Epidural Primarily Work on Side Needle Tip is Closer To– make sure I lay with bad side down for 15- 30 minutes after shot:
Steroid Epidurals – Why Some Work And Some Not So Well
– and if they don’t last long enough then have intrathecal midazolam:
Confirmed – Intrathecal (Spinal) Midazolam Gives 1-3 Months Relief in Chronic and Failed Back Pain
I give midazolam, neutralized with bicarbonate and diluted in saline, through the tailbone – it is very simple – makes you drowsy 1/2 hour
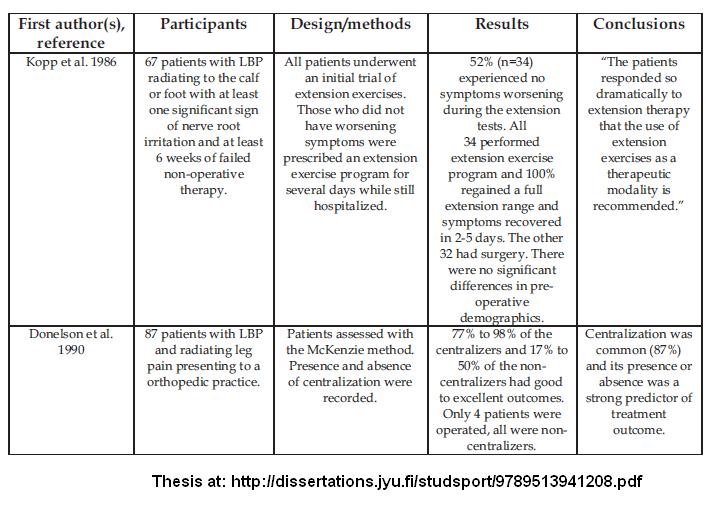
- McKenzie physiotherapy techniques are used and could be beneficial if pain can be “centralized” to back: more discussion on page 31 of thesis here
You can locate a McKenzie thereapist from here:
http://www.mckenziemdt.org/
- For leg pain, a simple injection of local by the knee, if done repeatedly can give relief:
Simple Sciatic Leg Pain Relief – Repeated Simple Knee level Peroneal Blocks - If you have psoriatic arthritis, chances are, you will have an inflamed sacroiliac:
The prevalence of sacroiliitis in psoriatic arthritis: new perspectives from a large, multicenter cohort
M. J. Battistone, B. J. Manaster, Domenic J. Reda and Daniel O. Clegg
Skeletal Radiology Volume 28, Number 4, 196-201 abstract here – 30-78% depending on study. - In celiac, 2/3 have sacroiliitis as well:
Adult celiac disease is frequently associated with sacroiliitis.
Paolo Usai.
Digestive Diseases and Sciences 40(9), 1906-1908 abstract here
So I think the odds are high there is some sacroiliac arthritis – this may be controlled by enbrel, but if is not, then it will cause belt level back pain and flare up your piriformis which I will discuss next. - Sacroiliac inject with local and steroid could cool that down nicely (but not the piriformis)
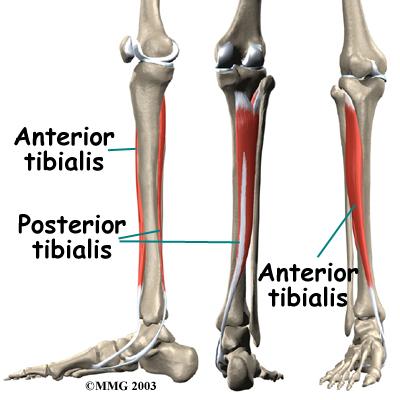
Double Crunch issue in chronic radiculitis process: – back and piriformis
When a nerve is already damaged spinally, it takes very little further damage elsewhere to create a major problem – they call it the “double crunch” – a bit damage spinally and a bit damage further down adds up to a big problem. Examples of double crunch:
- “One extraordinary study found that division of the piriformis muscle in patients with lumbosacral radiculopathies produced pain relief ”
Mizuguchi T.
Division of the pyriformis muscle for the treatment of sciatica. Postlaminectomy syndrome and osteoarthritis of the spine.
Arch Surg 1976;111:719 –722. as mentioned here (1st article); free poor HTML here - found 10/14 postlaminectomy and even spinal stenosis cases got pain relief though numnbess persisted
- I had a lady with severe sciatica admitted to hospital – her piriformis was bad so I worked it out both by below method, then with rectal massage. She actually felt considerably better despite fact she that when she finally had her MRI, she had an extruded disc requiring surgery.
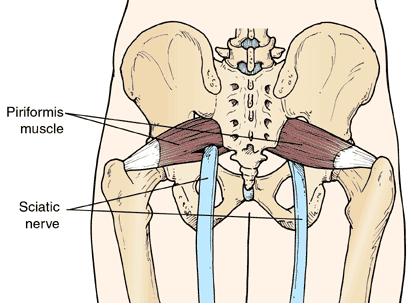
Piriformis
The number one contributor is going to be the piriformis. In fact, in cases where there is no spinal sciatica, 67.8% of the time, the problem is coming from the piriformis:
Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment
AARON G. FILLER, M.D., PH.D., JODEAN HAYNES, B.A., SHELDON E. JORDAN, M.D., JOSHUA PRAGER, M.D., J. PABLO VILLABLANCA, M.D., KEYVAN FARAHANI, PH.D.,
DUNCAN Q. MCBRIDE, M.D., JAY S. TSURUDA, M.D., BRANNON MORISOLI, B.A., ULRICH BATZDORF, M.D., AND J. PATRICK JOHNSON, M.D.
J Neurosurg Spine 2:99–115, 2005 free article here
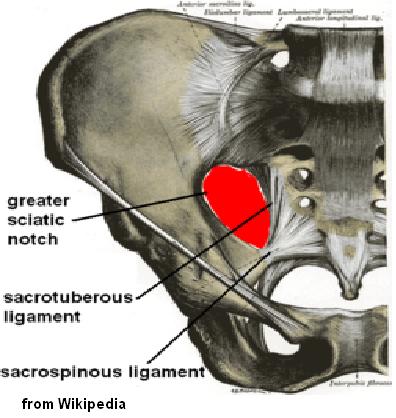
I find gluteal and/or piriformis triggers almost always occur in chronic back pain and are ignored. The piriformis can cause severe and pernicious back and leg pain because the sciatic nerve can go right through the muscle (on on the left side below):
Believe it or not, the diagnosis is best done by your family physician who can do a pelvic exam – the muscle will be very tender in the greater sciatic notch (piriformis goes thru it). I once had the vernerable Back Doctor Hamilton Hall laugh at me when I said I could feel a piriformis, but I doubt he had ever done a pelvic since his training…:
A Mayo clinic study used “Absence of other findings and ipsilateral painful rectal examination as the definitive test”
Hallin RP.
Sciatic pain and the piriformis muscle.
Postgrad Med 1983;74:69 –72. as mentioned in second article here
There are fancy tests for piriformis – they are not reliable – significant tenderness is.
Steroid injection can be done through the buttock but might only last a few weeks by itself . Botox injection can last 3 weeks – ?3 months. Studies got long lasting results combining it with physiotherapy mentioned below. I covered how to inject the piriformis:
Accurate Piriformis Injection
What is the real workhorse for dealing with the piriformis is engaging muscle from top or bottom and pushing transversely for 15 minutes.(I do 10 from top and 5 from bottom)
Piriformis Syndrome: Diagnosis, Treatment, and Outcome—a 10-Year Study
Loren M. Fishman, MD, George W. Dombi, PhD, Christopher Michaelsen, MD, Stephen Ringel, MD,
Jacob Rozbruch, MD, Bernard Rosner, PhD, Cheryl Weber, MD
Arch Phys Med Rehabil Vol 83, March 2002 Pages 295-301 abstract here
I then knuckle it out (takes 120+ rubs)
It needs to be repeated 2-3 times a week. Patients might need intermittent steroid injection if too painful and not making progress…Not many can afford botox (800 for 2 bottles) and insurance companies find it easy to not cover it.
Following Fishbain’s article above, he saw 3000 cases that came to him thinking they had a piriformis – and 1/2 were right.
The Piriformis Syndrome Is Underdiagnosed
LOREN M. FISHMAN, MD,1 and MICHAEL P. SCHAEFER, MD2
MUSCLE & NERVE November 2003, 646 – 649 – free article (2nd one) here
——————————————————
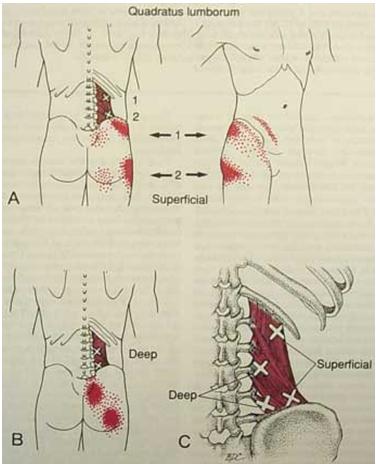
Role of Quadratus Lumborum, Gluteal and leg (often calf and lower end thigh adductors) Triggers
- Both Hip problems and Certain Back issues can aggravate piriformis issues
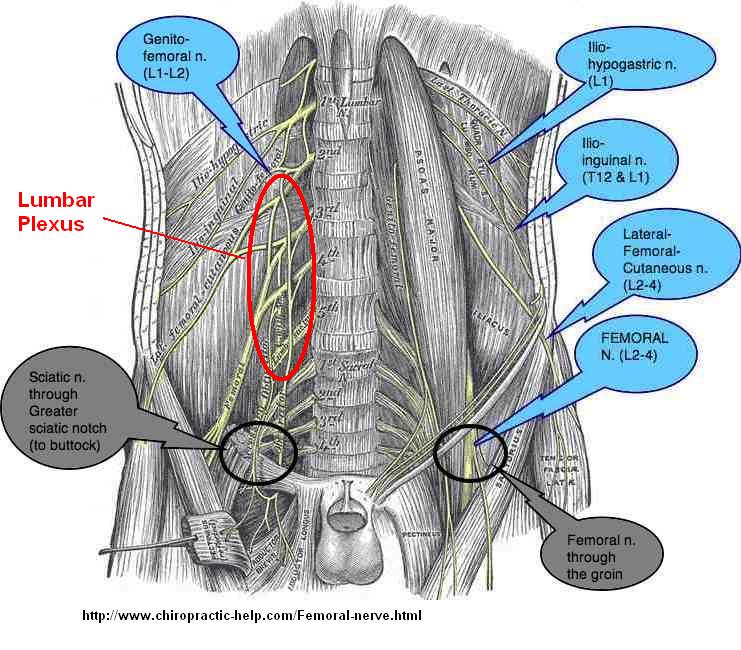
- One major muscle is the Quadratus lumborum – often with its adjoining muscle, the psoas in front
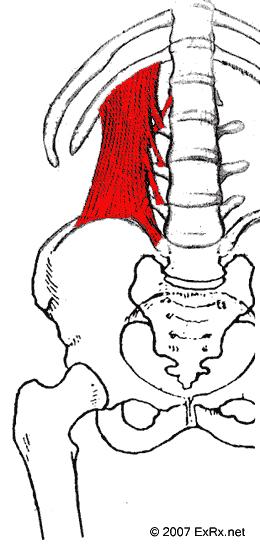
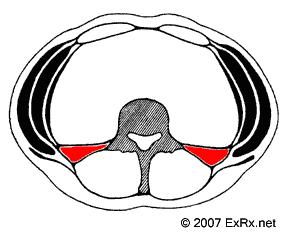
With the patient seated sideways on a chair, and facing away from me, I will grab the muscle and get my fingers in front of it. I will then push in posteriorly until it loosens up some. Then I will shake it until it let goes some. Then I will knuckle it. Then I will repeat the process lying down with bad side up facing away. If that dosn’t work, I will inject or needle it. Lastly, lying down facing away, I will have patient bring top shoulder back and work the muscle while in rotation – it’ surprising how much tightness is still apparent in rotation. It is interesting how much gluteal and trochanteric pain and lower hip pain can subside once the QL has been dealt with. I wondered why it can almost be neuropathic in severity at times and have concluded that the lumbar plexus that comes out between the tight QL and psoas must be affected and give more severe pain: (psoas in front, quadratus lumborum behind)
QL referrals: (originally from Travell& Simon’s book)
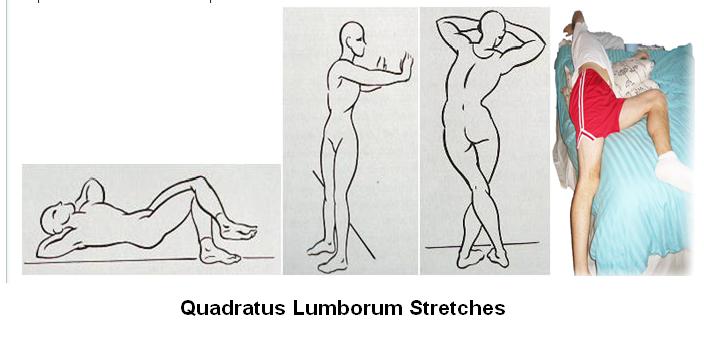
There are a variety of stretch exercises I got from a Korean article: – note keeping tha arm up on the side stretched helps
 \Facet Syndromes –
\Facet Syndromes –
a whole talk in self – the small joints chiropactors crack (actual manipulation may not a good idea for bad discs with radiculopathy)
I use an Activator – a device that can thump various levels without putting strain on discs to see how much comes out that way. There are no conclusive findings for facet syndromes except local tenderness and often 2 levels that show dis-similar rotations and movement on flexion/extension. They can however be suggested by local injection – we have a radiologist who does it here but he will not do complex cases. I inject levels with dilute testosterone without local and it stabilizes the leevls some – just started using it so cannot say for sure how well it works.
Near midline Iliac crest points
Medial cluneal nerve near PSIS – area often very tender near low midline back where hip crest has a bump in back. Injections with semineurolytic lidocaine or other agents might give temporary relief.
Sacral ligaments
discussed here
Chronic Low Back Pain Injection Spot
Trochanteric Bursitis
In:
Poster 234 Possible Clinical Triads in the Patients With Lumbosacral Radiculopathy
PM&R, Volume 3, Issue 10, Supplement 1, September 2011, Page S252
Jinghua He, Tsai Chao, Daniel Kline, Niu Niu no abstract
They found in MRI positive sciatica:
- 99% involved SI joint related pain
- 77% involved greater trochanteric related pain
- 40% involved lateral and anterior thigh numbness
- “We successfully treated patients with most severe acute LBP [Sciatica] by using steroid injection of the SI joint and trochanteric bursa as well as nerve block of lateral femoral cutaneous branch.”
One study:
Comparison of fluoroscopically guided and blind corticosteroid injections for greater trochanteric pain syndrome: multicentre randomised controlled trial
Steven P Cohen, associate professor,1,2 Scott A Strassels, assistant professor ,3 Leslie Foster, assistant professor,4 John Marvel, assistant professor,5 Kayode Williams, assistant professor,5 Matthew Crooks, assistant professor,5 Andrew Gross, pain management fellow,6 Connie Kurihara, pain management center,2 Cuong Nguyen, chief,7 Necia Williams
BMJ 2009;338:b1088 free article here
Required:
- three months’ duration,
- spontaneous pain in the lateral aspect of the hip,
- tenderness overlying the greater trochanter,
- one of the following three minor diagnostic criteria:
– increased pain with extremes of rotation abduction, or adduction
– pain with forced hip abduction
– pseudoradicular pain extending down the lateral aspect of the thigh.
Pain dropped from 4.5/10 to 2.6/10 after 1 month with “60 mg of depo-methylprednisolone and 2.5 ml of 0.5% bupivacaine”
My comment – early in the article, they admit that much of the inflammation could be extra-bursal – then they just inject a small area with small volume – I draw out a map of the whole area and inject it all with 10 mls total to make sure I get it all- can’t claim any better results though they did find blind injection got slightly better results… This is one of the situations that I call one shot Moron studies – I do not believe any chronic condition alive would respond to one injection and if you are doing injections, do 3 at 3-4 week intervals.
Gluteal Issues
Gluteal Burstis
Gluteal bursitis can mimic radiculitis or be part of it:
Pseudo-radiculopathy in subacute trochanteric bursitis of the subgluteus maximus bursa.
Archives of Physical Medicine and Rehabilitation [1976, 57(8):387-90]
Swezey RL abstract here
This is known as rotator cuff disease of the hip
I wrote about it here:
Rotator Cuff of hip causes Greater Trochanter pains
Gluteal and Trochanteric in Back/leg pains not really radiculopathy
One amazing study of women with chronic back pain where 77.7% had leg pain as well – They had injection of “peritrochanteric” steroid – 1 cc steroid mix (they don’t say what) and 3 ml local vs a control group:
Greater trochanter bursitis pain syndrome in females with chronic low back pain and sciatica
Fares SAYEGH, Michael POTOUPNIS, George KAPETANOS
Acta Orthop. Belg., 2004, 70, 423-428
- 300 cases
- females – 24 to 84 years with an average of 49.6 years
- chronic low back pain with 77.7% leg pains as well
- “All those patients had been seen repeatedly by other orthopaedic surgeons and complained of failed long-term conservative therapy”
- active group “given a local peritrochanteric infiltration of 1 ml of glucocorticoid mixed with 3 ml of 2% lidocaine”
- all had normal spinal movements and straight leg raises. None had neurological deficits. 14.3% had bilateral peritrochanteric issues. –obviously not a significant radiculopathy group
- “Recurrence should always be expected, but treatment may be repeated.”
Results
a href=”http://painmuse.org/wp-content/uploads/peritrochanteric-for-back_leg-pains.jpg”>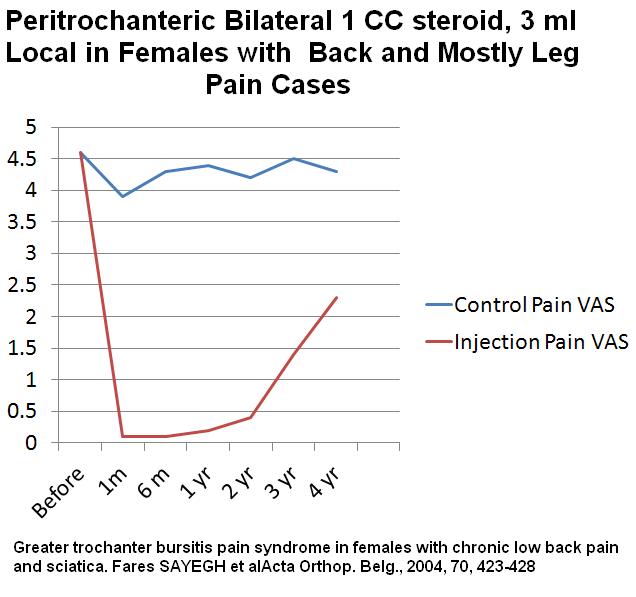
OK – not a typical radiulopathy but could well be a player in radiculopathy cases and cannot knock their findings…
Rotator Cuff of hip causes Greater Trochanter pains
- Pain with standing on affected leg after 10- 30 sec. “virtually always present”
- Mentioned in same referral above, if raising the opposite leg causes the raised leg side pelvis to dip (Trendelenberg) then the chances are high (1/2 – 3/4) that there is more than just bursitis – there is actual tears – it takes an MRI and a good radiologist to make that diagnosis and It is not often made.
- The fact the pain is “refractory to treatments” is a good indication:
Prospective study of refractory greater trochanter pain syndrome. MRI findings of gluteal tendon tears seen at surgery. Clinical and MRI results of tendon repair
Michel Lequesnea,Patrick Djianb, Valérie Vuilleminc, Philippe Mathieu
Joint Bone Spine Volume 75, Issue 4, July 2008, Pages 458–464 abstract here
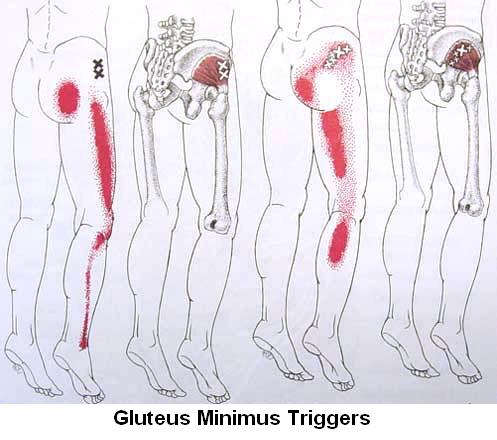
Gluteal Triggers Gluteal triggers can aggravate pain radiation in the leg and muscle knots in leg can make leg pain activation by sciatica easy
Problems – mostly facet in the mid Thoracolumbar spine can activate these gluteal triggers:
One of the fun things to do is to palpate very tender upper buttock muscles, then find out what levels in the lower ribcage area are sore and then thump them with the “Activator” – a device for manipulation. I don’t think it matters to much which way you thump them, if you are perpared to massage out the rotatories by massaging back and forth 120 times up and down paraspinously. Once the area is no longer tender, then go back to the buttocks – to the patient’s amazement the muscles will no longer be very sore and can be easily massaged out. This certainly confirms in my mind that the Thoracolumbar area is a player in buttock pains.
Muscles at that level, often activated by the spine, will also refer to buttocks:
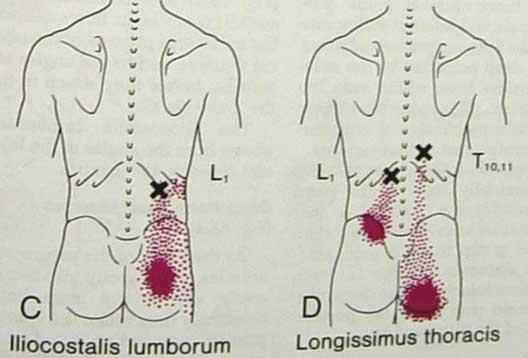 Thumping the back won’t take them out and they need to be worked on or injected.
Thumping the back won’t take them out and they need to be worked on or injected.
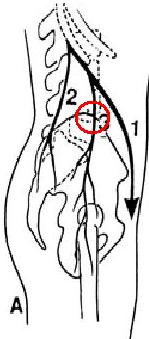
Getting complex enough? – here’s more: Lateral Iliac Crest Cluneal Nerve Pains
When all is worked on and done, then the really severe neuropathic area becomes obvious – and it is no where near the back – it is on the side just at the iliac crest. I think the quadratus lumborum pulls the ribs close to the iliac crest and if the rib should rub there, it creates severe pain that they will jump if you press on. I don’t usually find it until I have taken out Quadratus lumborum and thoracolumbar problems.
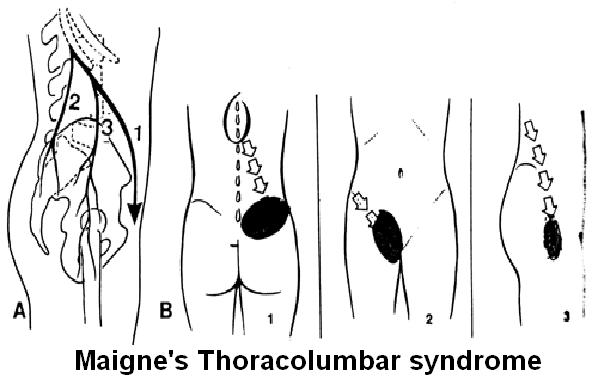
It is the most lateral clunal nerve in Maigne’s description:
Having said that, there are actually 3 nerves that go over that area:
I inject nerves by injection onto the side of the crest and depositing 40 mg kenalog over areas. I have had 2 former military types, who thought they were goners, some better that way. It doesn’t particularly go down leg but it can be so painful you might not be able to tell that.
Hip, yes hip problems
I am often suprised to find a severe “back problem’ has a back problems but also a serious hip problem that adds to the pain. There are some that have a malformed hip that pinches in certain positions – It is a relatively new disease and standard hip xrays don’t show much arthritis. Yet they will have severe pain with some catching at times. Hip internal rotation or hip extension may be painful. The tight buttock muscles will pull it such that it is more sore. Another issue that can be that seious is a labral tear in the hip. Dye enhanced MRI might not show it and hip arthroscopy might be needed to diagnose and certainly needed to treat it. In Regina, Dr. Beggs does it.
I wrote about it here:
Inguinal Groin Pain They Can’t Figure Out – Consider Femoroacetabular Syndrome Hip
Peripheral myofascial nerve triggers
Even in MRI negative sciaticas, multiple leg triggers are activated. Dr. Chen Gunn has devised a technique of electrically stimulating these spots and their associated back areas and this speeds up recovery – He calls it Intramuscular stimulation.
Dry-Needling of Muscle Motor Points for Chronic Low-Back Pain
C.C. Gunn, MA, MB, BChir, W.E. MILBRANDT, MD, A.S. LITTLE, MD,
and K.E. MASON, BSc, MSc
Originally in Bone and Joint but available here
A trained therapist might exist near you and can be checked by looking on his site at istop.org here
Examples or leg triggers include:
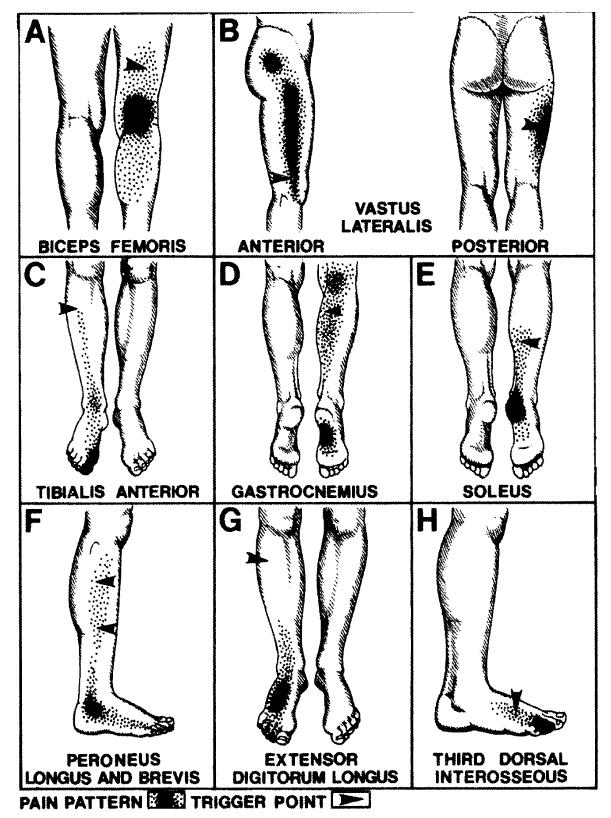
I recently had one lady with chronic scitica that I was able to gradually inject ands strech out her calf triggers. To my amazement I found exquisitely tight soleus muscle underneath – the consistency of thick tough cardboard – I injected, transverse stretch /massaged and knuckled it out – it was very painful to do but once loosened up, her leg got significantly better.
_______________________________
Leg Skin Nerves
Sometimes, the leg pains are primarily in the skin nerves and they can be injected with plain 5% dextrose in water (D5W) repeatedly with benefit (called neuroprolotherapy).
_________________
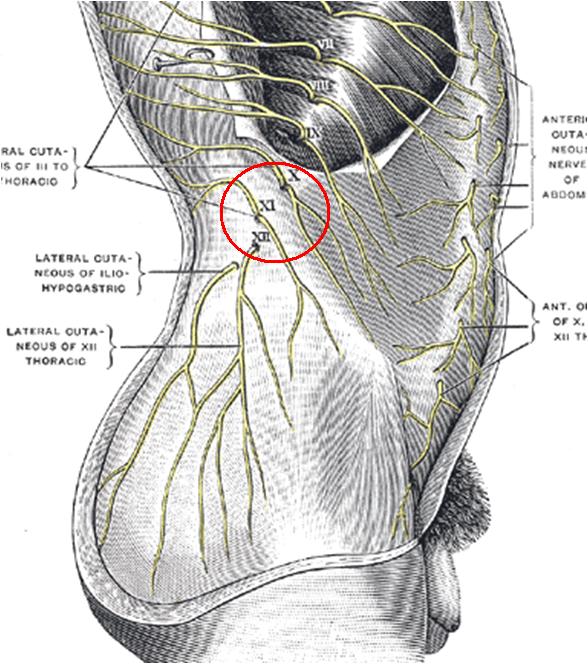
Posterior Shin-splints
With significant lower leg pains, posterior shin splints is almost guarenteed. This is especially the case if you don’t wear shoes around the house. It is deep and feltby pressing deeply in midline between your calf muslces. I just needle it from front – by passing an acupuncture needle between tibia and fibula. I press at the same spot posteriorly and pulse it with a pointer plus – after 2-3 minutes it softens up and feels better – two different levels may have to be done. Arch supports might be needed. It’s amazing how much better leg can feel just having that done…
The shinsplint muscles anterior and posterior:
_______________________
You mentioned you had fibromylagia:
Fibromylagia Neuropathy – FM is now considered a neuropathic pain dosorder. If numbness is a bad part of your leg conditon, then Chronic Inflammatory Demyelinating Polyneuropathy could be involved and pulse steroids and Immunoglobulin infusions might help:
A subset of fibromyalgia patients have findings suggestive of chronic inflammatory demyelinating polyneuropathy and appear to respond to IVIg
X. J. Caro, E. F. Winter and A. J. Dumas
Rheumatology (2008) 47 (2): 208-211. free article here
_________________
Instability
If you have suddden catching pains in the back – that might suggest some instability (or a lateral recess syndrome)- injecting the ligaments does help – saline and concentrated dextrose have both been shown to help. I have been trying dilute testosterone injections which are less sore but when repeated, may be beneficial – it is called prolotherapy – I am not sure if present case would be a candidate. A back brace would help here. There is also a common syndrome where people’s backs tire quickly after sitting or standing – often within 10-15 minutes – this can also be a syndrome of ligamentous laxity and benefit from prolotherapy – this is an article all in itself – sorry to short change it.
____________________________
Desperate and Miscellaneous ideas: were covered near the bottom of a previous article:
Consider repeated B12 injections – they do seem to help neuropathic pain and certainly help back pain see:
Chronic Back Pain Help – Forgotten B12 Injections and What Else Good For…
PS – if you are on any cholesterol lower drugs please get off them for a month to see if it helps – low vitamin D and Coenzyme Q 10 may make it worse while on statins.
Had one lady with back and leg issues aggravated by her posterior baker’s cyst in knee that can be injected.
Spinal cord stimulation has been used for intractible pain
Spinal pain pumps are an option
_________________________________
As you can see, dealing with this issue
Bottom line: – Get a steroid epidural
– Find a good therapist to work on your piriformis – if it is bad see if you can get botox injected
– Consider getting your SI joint injected. and maybe peritrochanteric with steroid
– Find an istop therapist for needling and perhaps a McKenzie therapist for Manual extension/flexion exercises on back
– Make sure your hip is not a problem and you are not unduely sore over you hip crest bone laterally
– see how bad your buttoock are and see if massage helps
etc as per article
Medications
It is true that medications do not seem to work well in sciatica pain:
Sciatica Pain Is Different and Does NOT Respond Much to Pregabalin (Lyrica)
Etanercept (Enbrel) for Radiculitis (Sciatica)
(long discussion of fact most meds don’t work)
For the medication route, I’d suggest either methadone if standard opioids don’t work or spinal morphine pump if desperate…
Ketamine shots can pull you out of the worst of it but are difficult to maintain and even worse here in Canada with Sandoz supplier shut down by FDA (grrrr…)
Good luck
Do others think I am wet? Please give your critiques! I couldn’t possibly cover everything so could use input..


I had an ALIF with BMP2 Infuse in 2010. Have severe pain tht I think in partly an inflammatory reaction to the BMP2. Have inquired about Enbrel for this but no consensus of opinion. Do you have any opinion?
————————–
Spinal fusions (where 2 back levels are fused together) are usually done by chipping bone of iliac crest (hip crest) at the back and poundind it in between two vertebra in back and hope it fuses – 1/3 of time does not fuse.
Industry designed a way of using a spinal cage (titanium LT-CAGE fusion cage device) for single level fusion
combined with “Infuse Bone Graft” = morphogenic protein-2 (BMP-2) on a collagen sponge. – used to stimulate bone growth.
Industry sponsored studies gave glowing reports of increased fusion rates (90%) versus 65% by old techniques – with “no adverse effects”:
http://www.healio.com/orthopedics/biologics/news/print/orthopedics-today/%7Bb5564936-9625-4da9-a1e6-f3f124a3d341%7D/bmp-2-improves-outcomes-of-two-alif-constructs
However, when the dust settled,
“risk of adverse events associated with rhBMP-2 is 10 to 50 times the original estimates reported in the industry-sponsored peer-reviewed publications”
as per
A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned
Eugene J. Carragee, Eric L. Hurwitz, Bradley K. Weiner
The Spine Journal 11, (6) , Pages 471-491, June 2011
http://www.thespinejournalonline.com/article/S1529-9430(11)00299-3/abstract
Early on, by 3 months, posterolateral fusion using recombinant human bone morphogenetic protein had a 16% back and nerve root incidence either due to direct irritation of dura and nerve roots or by bony growth into nerve root. Part of the nerve root irritation could be from the “approximately 500% higher rate of both epidural hematoma and wound complications with rhBMP-2 use and a posterior approach”.
We know for sure it can damage nerve roots because 6-9 % of men develop retrograde ejacuation (semen ejacuate goes into bladder).
Can there be help for the nerve root pain? – Possibly, unless there is bony growth into nerve root – something that is not necessarily easy to see on imaging. If there is bony ingrowth, then enbrel is not likely to work well. Enbrel works best in conjunction with a steroid epidural – Have the steroid epidural (lay with bad side down for 20+ minutes after shot and hope epidural went on affected side of epidural septum); if fails then add the enbrel shots -TWO of them a week apart. Half of the nerve root pain is going to happen from activation of muscle trigger knots – especially in the piriformis and gluteal muscles – dealing with them helps as well. Everything else I said about enbrel failure treatments applies as well.
Good luck.
Pingback: Severe Neuropathic Pain – Only 1/4 Respond to Standard Drug Protocols – What Else Is There? | Pain Medical Musing
Pingback: Reaching “Critical Mass” to Achieving Pain Control – Procedure Pearls | Pain Medical Musing
Pingback: What Can You Do For Sciatica Leg Pain | How to get relief from Sciatica
Pingback: What Can You Do For Chronic Sciatica | Treatment for Sciatic pain
Pingback: Mckenzie Exercises For Sciatica Pdf | Sciatica Natural Treatment
Pingback: Sciatic Nerve Glides Seated Shoulder Press | Sciatica Natural Treatment