Is there anyone who can help me, please???
- I am a 49-year-old woman who was diagnosed with an infected dental implant almost 3 years ago. Unfortunately, the Oral surgeon who removed the infected 3rd molar implant & cadaver bone in which the titanium pin was in did not do intra-operative cultures per the requests of my 3 MD’s & he also put more cadaver bone in an infected area. As it turned out, it was determined in a later Cauldwell-Luc procedure that I have invasive paecillomyeces Lilacinus fungus. I received IV infusions until 3 weeks into it when I became allergic to the Voriconazole prescribed to kill it. Ive had 3 more surgeries with the Drs. trying to clean out as much infection as they could.
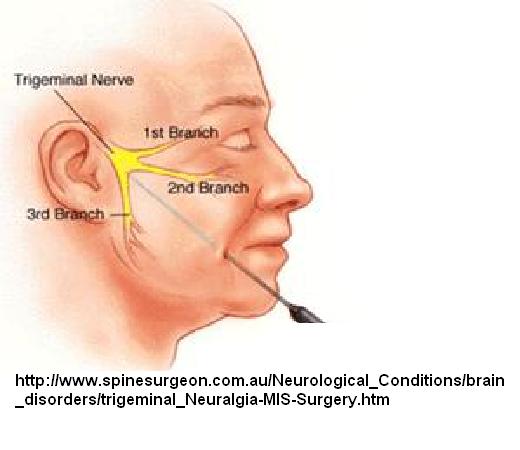
- I have had constant nerve pain in the right side of my face, eye & head since the beginning. I have been diagnosed with permanent damaged trigeminal nerve, ganglion branch & ocular nerve – from both the first surgery, done by a freshly minted surgeon whom I since have found out per other oral surgeons & MD’s alike, did not know what he was doing and was said to have “performed the most brutal implant extraction they’ve ever seen” and “should have known that you never introduce foreign matter back into an obviously infected area by putting yet more cadaver bone in after the extraction of the old”; and was “negligent in not doing the intraoperative culures and bone scrapings”.
- Bottom line is I am left with excruciating pain for which I am on Dilaudid & morphine. Both are short-acting.
- The long-acting form of narcotics I have tried but had to stop because of severe depression in both cases were Opana ER for approx. 9 months, then off 6 weeks, atwhich point I returned to my undepressed self; then my Pain Dr. Prescribed Exalgo XL, which I took for 2 months at which point it became apparent the severe depression returned. I quit taking it and 9 days later I was back to my normal upbeat self in spite of the constant extreme pain, which I can control somewhat with the two short-acting pain meds without suffering from severe depression.
- Four months ago a neuro-opthamologist told me, after running all types of tests & scans, that the osteomyelitis did permanent damage to my right ocular nerve and said I might lose site in my eye over time. A neurosurgeon told me I am not a candidate for micro-decompression or rhizzotomy due to the ocular involvement, etc.
- I am desperate for relief from the intractable pain and do not want to live my life on pain medications. BTW: I also take 800 mgs. of Neurontin per day.
- My husband drove me 8 hours south to a pain medicine M.D. who said he would do what I asked for, which is Botox injections ( after researching Botox for this condition and checking him out too). I had the first set of 3 injections yesterday. It was terrible. I did not know that I would look like a stroke victim afterwards. He said it would go away in a half an hour – that was 38 hours ago and I still can only partially open my eye, maybe by 35%. There is still quite a bit of swelling. He injected me just above my right eyebrow; in the middle of my cheek and at the base of my skull. I wouldn’t mind the droopiness in my face if I had no pain. I had 80% relief for about 2 minutes, then it all rushed back in worse than before and that is where it remains as I type this. I got less than 5 minutes with the Dr. and asked as many questions as I could quickly.
- Two of those questions I pose to you as well: a. Can Botox really help me or am I wasting my time & money to do this every 2 to 4 weeks as the Dr. prescribed? b: I read of a particular type of laser that is supposed to help actually heal and regenerate the nerve myelin sheaths, over a period of time. There is a facility in South Carolina (I am in the northern part of California) that does this laser treatment 2-3 times per day for 2 weeks. The Dr. I was just treated by with Botox says that the laser is a gimmic and it doesn’t work. He also said that the Botox injections, which he would rotate injection sites along various parts of the nerves, on every visit, would actually Heal the nerves as the laser was reported to do. I cannot find anything about Botox healing the nerves, only sometimes killing the pain. Can anyone help me??? Please???
This is horrible situation. I know of no great ways to handle this and can only give some ideas you can try. Maybe someone out there has a better idea? I will cover some ideas – Drugs is near the end..
Firstly, I am not an expert of facial neuropathic pain and have not seen patient. I have ideas only that might give her hope…
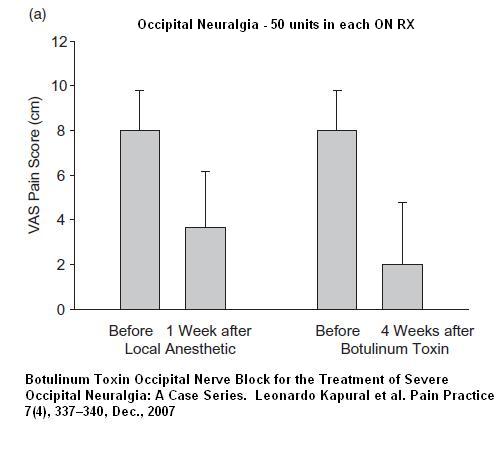
My lastest experiences with Botox have not found it not as good as I would like. Indeed, with occipital neuralgia the initial study showed mediocre results:
Botulinum Toxin Type-A (BOTOX®) in the Treatment of Occipital Neuralgia: A Pilot Study
Martin Taylor DO, PhD, Sachin Silva BS, Constance Cottrell RN, PhD
Headache: The Journal of Head and Face Pain Volume 48, Issue 10, pages 1476–1481, November/December 2008 abstract here
“The dull/aching and pin/needles types of pain reported by the subjects did not show a statistically significant improvement during the trial period. The sharp/shooting type of pain, however, showed improvement during most of the trial period except weeks 3-4 and 5-6.”
However, one was able to get results in one study by making sure they penetrated the nerve – testing to see if can get radiation when they used a nerve probe:
Botulinum Toxin Occipital Nerve Block for the Treatment of Severe Occipital Neuralgia: A Case Series
Leonardo Kapural MD, PhD1,*, Mark Stillman MD2, Miranda Kapural MD1, Patrick McIntyre MD1, Maged Guirgius MD1, Nagy Mekhail MD, PhD1
Pain Practice Volume 7, Issue 4, pages 337–340, December 2007 abstract here
In the sitting position, the superior nuchal line was identified in each of the patients and the occipital artery pulse palpated. After skin preparation, using a 24 G stimulating needle we pierced the skin nearby. Using an initial stimulating current of 1.0 mV, the needle was repositioned until a tingling sensation felt to the top of the occiput and maintained at 0.5 or less mV allowing the botulinum toxin to be delivered as close as possible to the greater occipital nerve… We used 50 U of BoNT-A per painful side.”
Note however the relief they got from just local – I doubt one would get that in the face…
In Trigeminal Neuralgia the best results have been obtained by injecting the trigger site. Without one, it is more difficult. The problem is, you cannot give injections frequently, otherwise allergic resistance to the compound can occur – though how frequent this occurs with the newer more purified formulation is unclear. Note – case report of injecting right into a chronic irritated tooth with botox has suggested benefit but I don’t know -may not be a good idea if infection involved…
Considerations:
- First. one would need to know the status of her infection – something that is not clear. – If there is still active infection then not much works for that sort of pain.
- Also, there is no indication whether she has a trigger zone – an area of extreme sensitivity that causes severe jabs when touched. – there, botox might work well
Most of experience I have with neuralgic facial pain of her type, would be from post herpetic neuralgia. I can’t imagine having the mid face injected without having topical Emla anaesthetic cream patch put on for a period prior – right under eye could be particularly painful. They will let you do it once or twice before they say no thanks…
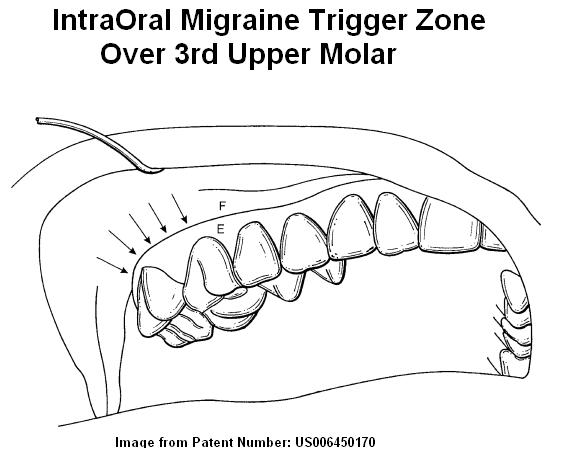
- I’m assuming it was the third upper molar that was affected –
This is a Hypersensitive Area:
The area over the third molar is especially sensitive and implicated in helping to perpetuate chronic migraines. A Dr. Mark Freidman has written several patents discussing how important this area is for migraines:
- 93% of migraine sufferers are tender over the top gum above the upper 3rd molar on the side the migraines are most affected.
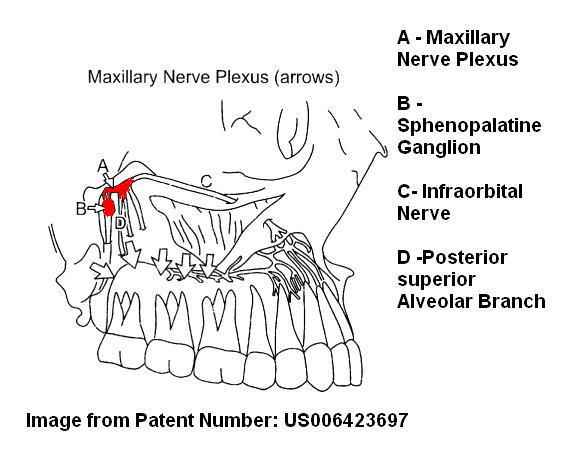
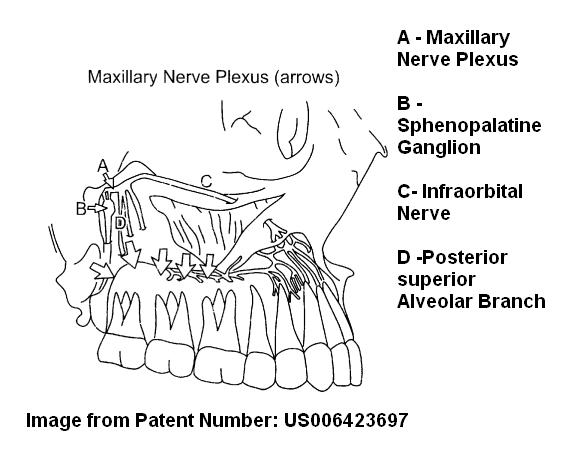
There is a nerve plexus there that is effected in this area:
Friedman treated this area with:
a laser apparatus:
– Treatment of vascular headache and atypical facial pain
and Treatment of migraine, post-traumatic headache, tension-type headaches, atypical facial pain, cervical pain and muscle spasm
a cold water pump apparatus:
Treatment of vascular and tension headache atypical facial pain allergic rhinitis and cervical muscle hyperactivity
and Treatment of vascular and tension headache, atypical facial pain, and cervical muscle hyperactivity
topical anti-inflammatories –
Intraoral topical anti-inflammatory treatment for relief of migraine, tension-type headache, post-traumatic headache facial pain, and cervical-muscle spasm
Use of topical agents has been progressed by a further patent : free pdf here
I suspect injury to this area would damage an exquisitely sensitive area and set up problems.
It would also be a site that could be treated as per various patent descriptions:
– a cold water assembly, cooling area, might give temporarly relief
– intraoral laser to area might be helpful
– Topical agents to area might be quite helpful:
For an abscessed tooth, I often use 5% clindamycin (one of the best oral agents for dental abscess), 5% lidocaine (local) in Pennsaid lotion ( a penetrating Dimethysofoxide (DMSO) formulation with voltaren =dicofenac in it). – a small piece of cotton ball is soaked with stuff and held onto area – is gross to use and drains down and freezes throat (careful eating until unthawed) but can kill pain in area and help infection.
If there was any infection still left in her case, It might be better with 3% iodochlorhydroxyquin (clioquinol), 5% lidocaine in Pennsaid lotion. The clioquinol is best known by doctors as the ingredient in Locacorten-vioform ear drops that fights both bacterial and fungal infections. I looked up re toxicity re clioquinol and all I could find was that it is a promising agent for treating Alzheimer’s – but not toxic
Cochrane Database Syst Rev. 2006 Jan 25;(1):CD005380.
Clioquinol for the treatment of Alzheimer’s Disease.
Jenagaratnam L, McShane R. abstract here
For just local pain, I had 10% lidocaine troches (small lozenges) made up once. You would break off a piece and put into chewed gum so in middle of gum but touching mucosa just above where 3rd molar was – hold until numb should help. Might however numb all the mouth and be unpleasant…
A more sophisticated technique involved apply topical agents under a plastic shield made. I discussed that here: (about 1/2 way down):
Trigeminal Neuralgia
——————————–
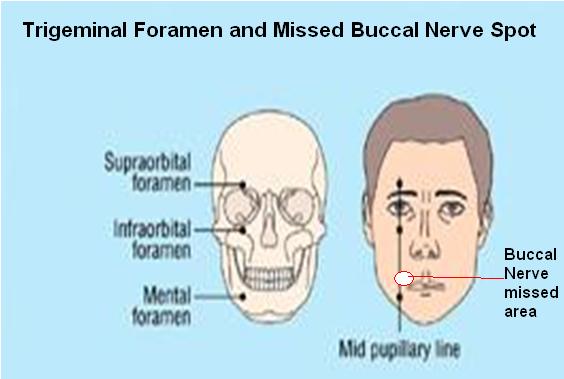
Facial Nerve Areas of Treatment: – nerve foreamen injections
- If the skin is tender to pinch anywhere, Just superficial injection of plain 5% dextroe (D5W) helps. This was the basis of a talk about treating certain residual trigeminal neuralgias presented at the Canadian Association of Orthopedic Medicine (CAOM) conference 2011. I use a 10 ml syringe 30 guage needle bent for horizontal injections and inject horizontal sweeps just under the skin where tender (called neuroprolotherapy) -surprizingly has freezing properties– needs to be done at least 3-6 times maybe every 5-7 days.
- Usually nerves that I have botoxed need to be injected with semineurolytic local to get full benefit:
Best article on use of nerve damaging local comes from:
The long lasting effects of peripheral nerve blocks for trigeminal neuralgia using a high concentration of tetracaine dissolved in bupivacaine.
Fumio Goto et al.
Pain 79(1), 1 January 1999, 101-103 abstract here
- 4% tetracaine dissolved in 0.5% bupivacaine (0.2 – 0.5 ml) into supraorbital or infraorbital foramen – relief for more than 3 months though other areas may need Rx
- Combo of tetraciane and bupivacaine worked best.
- Transient hypesthesia for 2 weeks
- Example – “0.2 ml of the mixture of tetracaine and bupivacaine was injected to both supraorbital and infraorbital nerves. Two weeks after block, pain was completely relieved. There were no sensory disturbances around the nerve block and complete pain relief continued for 2 months. Edema of the eyelids dissipated within 2 weeks.” [3 months later infraorbital nerve canal was reinjected with 0.2 mls and this lasted 3 months] .
- It’s a rellief that 0.2 mls could be injected supraorbitally without any ptosis…
The use of 4% tetracaine in 0.5% bupivacaine was repeated in 2001:
Clinical Journal of Pain. December 2001 17(4) 323-326.
High-Concentration Tetracaine for the Management of Trigeminal Neuralgia: Quantitative Assessment of Sensory Function After Peripheral Nerve Block
Radwan, Inas Abdel Moneim M.D.; Saito, Shigeru M.D., Ph.D.; Goto, Fumio M.D., Ph.D abstract here
- 5 cases – mean relief 2 months and “relatively safe” for elderly even
Local injections combined with Standard Trigeminal Nerve Trunk Blocks:
Standard nerve trunk nerve blocks combined with local sites using 10% lidocaine in 7.5% dextrose has been tried:
Efficacy and safety of high concentration lidocaine for trigeminal nerve block in patients with trigeminal neuralgia
K. R. Han, C. Kim, Y. J. Chae, D. W. Kim
International Journal of Clinical Practice Volume 62, Issue 2, pages 248–254, February 2008 abstract here
- “patients were treated with infraorbital nerve block (IONB), superior orbital nerve block (SONB), maxillary nerve (V2) block, mandibular nerve (V3) block or Gasserian ganglion block (GGB) with 10% lidocaine, depending on the location of the pain on their faces. V2 and V3 blocks as well as GGB were performed under fluoroscopic guidance.”
- Before the injection of 10% lidocaine, test blocks were performed using 1% lidocaine with an injection volume of 0.2 ml for GGB and 0.7 ml for the rest of the trigeminal nerve blocks.
- After the selected nerve had been completely anaesthetized, 10% lidocaine with the same volume as the test block was injected through a 21-gauge block needle (Neurotic nerve block needle, Hakko Medical C., Japan); 5 cm for SONB and IONB, 8 cm for V2 block and V3 block, and 10 cm for GGB.
- Results – Twelve of the 35 patients (34.3%) responded favourably to the treatment and were considered as success.
– Eleven patients experienced complete pain relief and one could tolerate pain without medication 1 day after the blocks, which lasted for 3–172 weeks.
– Four patients experienced mildly decreased sensation in the region of the face supplied by the nerve 1 day after the blocks; however, all recovered normal skin sensation in 6 months - Not the greatest results but for the lack of side effectrs, one should consider trying it first….
Alcohol Blocks Trigeminal nerve trunks:
NM, Patton DW.
Peripheral alcohol injections in the management of trigeminal neuralgia.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:12-7. abstract here
- last an average of 11 months
- left with some numbness which can sometimes be unpleasant
Rhizotomy Trigeminal nerve trunk blocks – beyond the scope of this article
Pulse Radiofrequency to Nerves – an exciting possiblity.
If trigeminal nerve foramen injections gave temporary benefits, then pulse radiofrequency treatment could be tried. I suspect it must knock out C fibers because you do not get much of the facial numbness of real rhizotomies – the temperature of the probe is brought to 45 degree centigrade – your water tap can probably go hotter then that. All they use is a fancy shielded soldering iron like tip applied to area for 120 seconds.
as per:
Pulsed radiofrequency ablation of the infraorbital and supraorbital nerves for treatment of chronic periorbital and facial pain
Nicholas P. McKernan, MD and Andrew J. McDavid, MD
poster online at http://www.painmed.org/files/poster236.pdf free poster here
- “The right IO[infraorbital] ridge and SO [supraorbital] notch were infiltrated with 1% lidocaine for local anesthesia and two 22-gauge 3.5 inch insulated radiofrequency needles advanced under fluoroscopic guidance to an osseous endpoint at the inferior and superior edges of the IO and SO foramina respectively. The RFA probes were then inserted and sensory testing achieved at 0.5mAmps. With the pulse setting, the probes were heated to 45°C for a total of 120 seconds in both locations.”
- “The resulting lesions provided our patient with over a year of relief from his facial pain, and caused a dramatic reduction in his headache symptoms. Pulsed RFA has been repeated four additional times over the past six years with similar results”
- This is a new technique and not widely accepted – one would have to go to a centre where this is done – I would probably talk to one of the authors and find out if you should go there or if they know anyone more local or whether it would be better to got there..
- I found a link for the second author Dr. Andrew Mc David at Scott & White Hospital and Texas A&M Health Science Center College of Medicine, Temple, Texas here
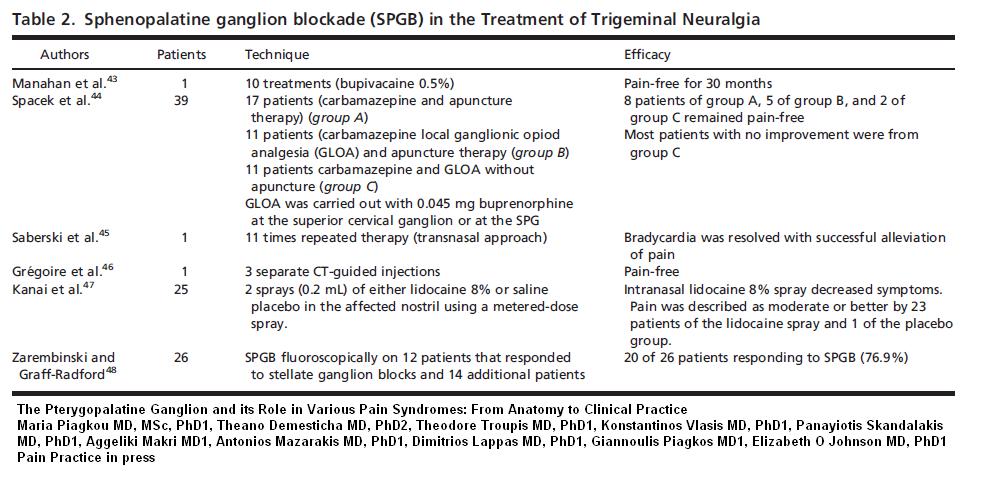
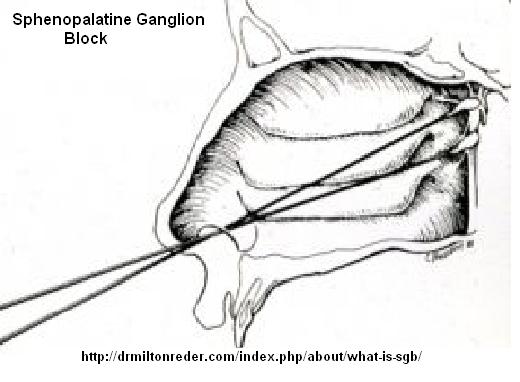
Sphenopalatine Ganglion Blocks (SPG blocks): – a maybe – could try and see
Various studies have tried blocking this ganglion in treatment Trigeminal Neuralgia:
The SPG is very close to this delicate maxillary nerve plexus:
I have use it to numb up the headache area supraorbitally though suspect could help mid face some too.
It is blocked thru the nose (note because I use concentrated local, one swab is usually enough – if held long enough):
Self administration Techniques:
Easiest Technique:
Commercially available Xylocaine 8% spray:
Intranasal lidocaine 8% spray for second-division trigeminal neuralgia
A. Kanai*, A. Suzuki, M. Kobayashi and S. Hoka
British Journal of Anaesthesia 97 (4): 559–63 (2006) free article here
- two sprays lidocaine 8% in the affected nostril
- patients were asked to lie in the supine position with their necks extended 30–45 degrees, and maintained the position for 30 s.
- dropped pain from 8/10 to 1.9/10 and lasted an average of 4.3 hours
Easy technique:
Reg Anesth. 1996 Jan-Feb;21(1):68-70.
Patient-administered sphenopalatine ganglion block.
Saade E, Paige GB. abstract here
- Patient lying supine(on back), a pillow under shoulders and head and neck completely extended. Head tilted to side being done a bit
- 2 mls 4% lidocaine dripped down outer side of nasal passage
- position maintained 15 minutes
- got 50-60% relief of cancer pain to area
More involved: ( ibid above)
- same position
- draw 1.5 ml 4% lidocaine local into 3 ml syringe attached to an IV plastic cannula.
- Insert cannula into nostril as far as tolerated
- By slowing pushing on plunger, drip contents into nose slowly over 15 minutes
- Do 3 times daily ?bilaterally
My technique – even more involved:
- Using 60% lidocaine soak a thin aluminum or plastic swab – not to use more than 0.2ml at a time..
- put into back of nose aiming up same direction as contour of nose.
- Should be able to hit back wall of upper nose (if aim too low get into back of throat)
- Hold in 20-30 minutes
Repeated use should eventually desensitize area from some of the pain as well.
A severe case is described that responded to facial pulse radiofrequency combined with self – administered SPG blocks:
Pulsed Radiofrequency V2 Treatment and Intranasal Sphenopalatine Ganglion Block: A Combination Therapy for Atypical Trigeminal Neuralgia
Michelle Nguyen, MD; Denise Wilkes, MD, PhD
Pain Practice, Volume 10, Issue 4, 2010 370–374 abstract here
- Pulse radiofrequency Procedure: ” nerve was located via the sensory stimulation mode at 50 Hz with 1 millisecond pulse duration. The voltage was increased in 0.1 V increments until sensory stimulation was felt in the maxillary distribution. Sensory stimulation was noted at 0.6 V, though only covered a small portion of her pain below her eye and laterally. The position of the SMK needle is shown in Figure 1. The duration of the pulsed RF treatment procedure was a total of 300 seconds using a duration of 20 milliseconds at a temperature of 42°C and a rate of 2
pulses/second. Two cycles were completed on auto-pulse mode. Following the pulsed RF treatment, we administered 4 ml of 0.125% bupivicaine with 16 mg dexamethasone. The SMK needle was then removed.” - SPG Block procedure: – used 4% lidocaine but vague beyond that – did self instruct patient to do.
- This program was combined with Methadone 5 mg twice daily and Pregabalin (Lyrica) 200 mg three times a day – the need for these 2 agents weaned over 2 years
- Article from Department of Anesthesiology and Pain Management, University of Texas Medical Branch, Galveston, Texas, U.S.A.; cannot locate authors
Laser Treatment
I cannot access reference so only have what was stated by another author:
Treatment of trigeminal neuralgia – A review
Jyothi Tadakamadla,* and Mamatha GP
Journal of Oral Health Research, Volume 1, Issue 1, January 2010; 9-18 free article here
They state:
“Laser treatment has also been used experimentally for trigeminal neuralgia. In a study, human subjects received irradiation of the skin overlying peripheral nerves with a helium-neon laser for 20 seconds to each selected site. The treatment was accompanied by irradiation of the skin overlying painful areas for 30 to 90 seconds. Control subjects received placebo treatment. Laser or placebo therapy was repeated 3 times weekly for 10 weeks. Subjects in the experimental group exhibited a statistically significant reduction in the intensity and frequency of painful episodes (35).
Eckerdal and Lehmann have observed from a double blind, placebo controlled study that low reactive-level laser therapy (LLLT) is effective in the treatment of trigeminal neuralgia. They have concluded that LLLT treatment is an effective method and an excellent supplement to conventional therapies used in the treatment of trigeminal neuralgia (36).”
35. Walker J. Relief from chronic pain by low power laser irradiation. Neurosci Lett 1983;43:339-44.
36. Eckerdal A, Lehmann Bastian H. Can low reactive-level laser therapy be used in the treatment of neurogenic facial pain? A double-blind, placebo controlled investigation of patients with trigeminal neuralgia. Laser Therapy. 1996; 8: 247-252.
Topical Agents:
The agents would be the same as used for post-herpetic neuralgia
- Repeated application of 5% lidocaine patches (in US) would gradually reduce the pain and help control it as well. This was noted in post surgical cases: see blog note: Lidocaine Patches For Post Surgical Chronic Pains
- I wrote a blog note on preparing your own using tinfoil or other backing with 10% lidocaine in gelatin – would suggest you will need to leave your formualtion a couple days until tacky or maybe double up on the strength of gelatin.See: Making Your Own Lidocaine Patches
- Another lidocaine topical is 5- 10% lidocaine in Uremol lotion – the urea helps the penetration and makes it work better
- Another combo that has been found useful involves the use of topical ketamine: Topical Ketamine For Post-herpetic Neuralgia. I concluded that Amitriptyline 4%, Ketamine 2%, and lidocaine 5% in Lipoderm might be the best combo with adding 1% hydrocortisone might be useful in easily irritated cases. Special note – do not use PLO gels as way too irritating for face – use lipoderm
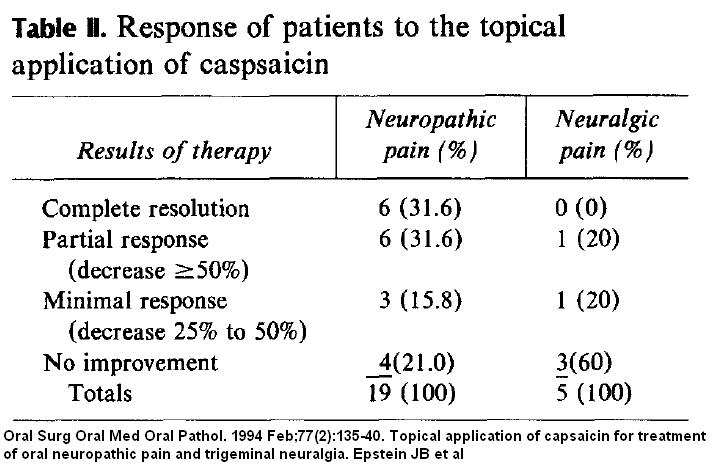
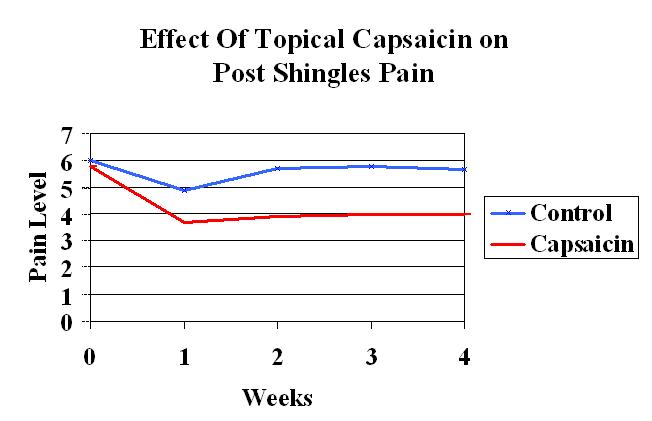
Capsaicin – red pepper extract – it exhausts the pain transmitter in the skin if used REGULARLY and continued so.
Early study:
Oral Surg Oral Med Oral Pathol. 1994 Feb;77(2):135-40.
Topical application of capsaicin for treatment of oral neuropathic pain and trigeminal neuralgia.
Epstein JB, Marcoe JH. abstract here
- most neuropathic pain of mouth mucosa, tongue, jaw, or periodontium
- “Patients were instructed to apply capsaicin cream (0.025%) (Zostrix GenDerm Corp, Northbrook, Ill.) to the site of discomfort four times a day.”
results:
- Note it worked much better for the neuropathic pain than the sharp shooting neuralgic pains with a mouth trigger.
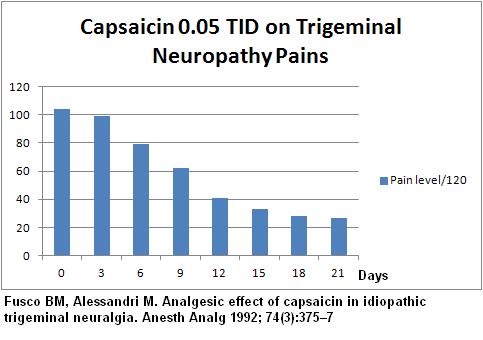
These results seemed too good to be true but this techniques was repeated again:
Fusco BM, Alessandri M. Analgesic effect of capsaicin in idiopathic
trigeminal neuralgia. Anesth Analg 1992; 74(3):375–7 abstract here
- used 0.05% Capsaicin applied 3 times daily – note the pains are out of 120 because I added up results of 12 people with a score of 0-10 – sorry just too lazy to convert to 10..
- 2 out of 12 did not respond and 4 of remaining relapsed in 95-149 days – still that means there is a 50-50 chance that capsaicin could control pain…
Results:
- It hurts in the eye (like pepper spray) so use gloves on hands and maybe consider wearing googles when applying…
Another Capsaicin technique involved hitting severe pains spots ONCE with high concentration 8% patch and “burning out” an area of pain:
Pain Med. 2011 Jan;12(1):99-109.
A multicenter, randomized, double-blind, controlled study of NGX-4010, a high-concentration capsaicin patch, for the treatment of postherpetic neuralgia.
Irving GA, Backonja MM, Dunteman E, Blonsky ER, Vanhove GF, Lu SP, Tobias J; abstract here
- Left on for ONE HOUR ONCE – usually pretreeated with topical anesthetic and given oral opioids to help with pain…
The Complex Regional Pain Issue:
This case is so severe, damaged to the nerves handling the blood vessels and sympathetic nervous system has probably occurred.
- Stellate ganglion blocks may be helpful here and botox into the stellate might give more lasting results
- IV pamidronate infusions can break CRP syndrome pains and I have wrote about it here:
Pamidronate and Clodronate – hope for Reflex Sympathetic Dystrophy (aka CRPS) and Back Pain - IV magnesium is a simple possibility:
New Hope For Complex Regional Pain Syndrome I – 5 days Magnesium Infusions
I have scaled down use to 2 gms in 20 mls D5W given over 40 minutes by syringe pump – I use the leg veins as it is hard on veins – It burns a little. It helped control one gentleman with mild facial neuropathic pain and comorbid migraines with just one day’s worth at a time… This case might need 5 days…
Occipital Nerve Blocks:
- about 1/2 of trigeminal neuropathic pains will respond very temporarily to occipital nerve blocks; if area occipitally very tender, then injections and work to area should be considered.
Treating Occipital Nerve Pains helps trigeminal pains:
J Headache Pain. 2012 Mar 3. [Epub ahead of print]
Occipital nerve block is effective in craniofacial neuralgias but not in idiopathic persistent facial pain.
Jürgens TP, Müller P, Seedorf H, Regelsberger J, May A. abstract here
Treat Peripheral triggers:
TMJ – triggers in masseter, temporalis, lateral pterygoid, and sternomastoid muscle need to be dealt with. – don’t forget lateral pterygoid is unseen but very important.
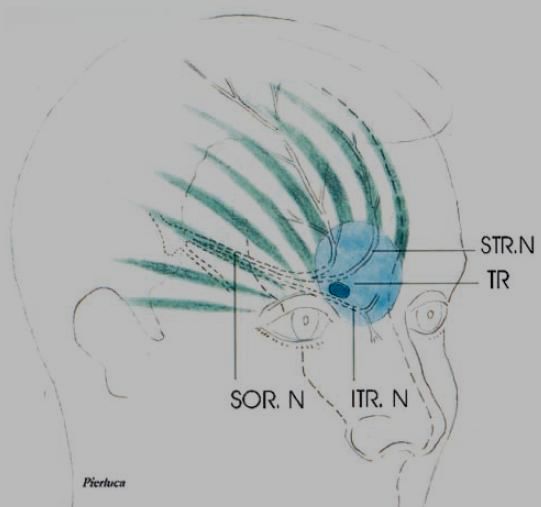
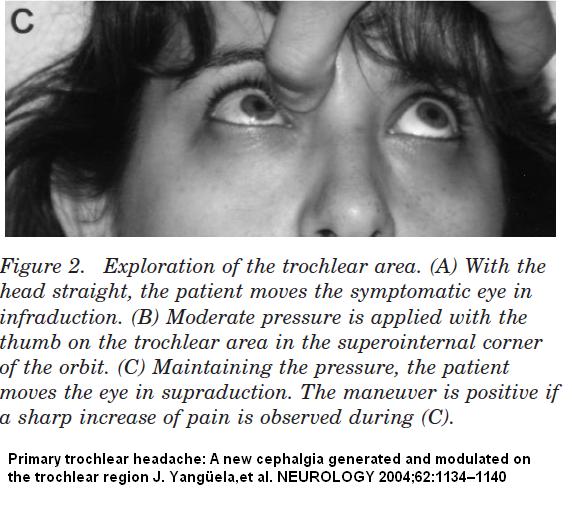
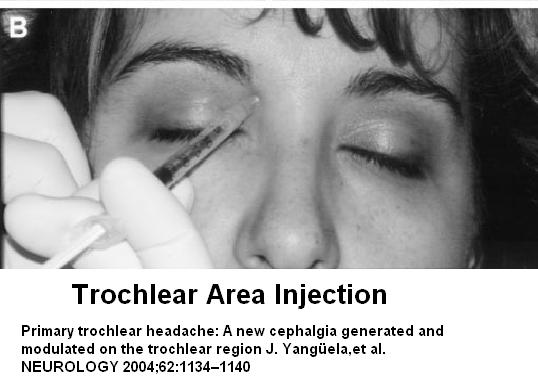
If there is much pain in troclear area, then injection into trochear muscle needs to be done:
Primary trochlear headache: A new cephalgia generated and modulated on the trochlear region
J. Yangüela, MD*; M. Sánchez-del-Rio, MD*; A. Bueno, MD*; A. Espinosa, MD;
P. Gili, MD*; N. Lopez-Ferrando, MD; F. Barriga, MD*; J.C. Nieto, MD; and J.A. Pareja, MD, PhD*
NEUROLOGY 2004;62:1134–1140 abstract here
It originates from the upper inner eye socket and radiates to temple and forehead
Tip-off is tenderness to upper inner eye socket that is worse on looking up:
It is injected thus:
- Patients were given a 1-mL injection (25G 0.5-inch needle) containing 3 mg of dexamethasone and 3 mg of methylprednisolone targeted to the symptomatic trochlea
(Celestone Cronodose, Schering-Plough Laboratories). (I must admit I give 40 mg Kenalog basically because they complain that recurence is common and I want to prevent that.) - Works amazingly well for side locked frontal headaches where tenderness is in trochlear area.
Peripheral Field Stimulation:
When most measure have failed, a peripheral nerve stimulator has been used:
An early article was here:
Peripheral Stimulation for Treatment of Trigeminal Postherpetic Neuralgia and Trigeminal Posttraumatic Neuropathic Pain: A Pilot Study
Johnson, Mark D. M.D., Ph.D.; Burchiel, Kim J. M.D.
Neurosurgery: July 2004 – Volume 55 – Issue 1 – pp 135-142 abstract here
Articles since include:
Trigeminal and occipital peripheral nerve stimulation for craniofacial pain: a single-institution experience and review of the literature
KONSTANTIN V. SLAVIN, M.D., M. EFKAN COLPAN, M.D., NAUREEN MUNAWAR, M.D., CHRISTIAN WESS, M.D., AND HRACHYA NERSESYAN, M.D., PH.D.
Neurosurg Focus 21 (6):E6, 2006 free article here
Drugs
Subcutaneous B12 – I originally came across 2 articles that found Frequent B12 injections were useful in chronic pain:
Chronic Back Pain Help – Forgotten B12 Injections and What Else Good For…
Since B12 supplementation augments the effects of gabapentin in rats:
Proc West Pharmacol Soc. 2004;47:76-9.
Oral administration of B vitamins increases the antiallodynic effect of gabapentin in the rat.
Reyes-García G, Caram-Salas NL, Medina-Santillán R, Granados-Soto V. abstract here
I suspected it helped the neuropathic component – and this seems the case – people with pain just in their sacral ligaments do not get benefit whereas people with postlaminectomy chronic radiculopathy do. I have since found it seems to have subtle neck radiculopathy as well. People say it seems to take down the background noise pains and just leave them with their primary pains. Unfortunately, the super-high levels need to be maintained and people find it wearing off after 2-7 days. Given that it has zero complications, it might be worth a try here. I teach patients to give their own shots and eventually sell a box of 1 cc needle at cost -much less then the drug store charges!
There are a variety of anti-neuropathic pain drugs available –
TCA’s – amitriptyline and nortriptyline if sedation an issue
SNRI’s – Venlafaxine at high dose; Cymbalta;
Gabapentin and pregabalin
3rd line agents like Zanaflex
For pain, tramadol if mild – opioids otherwise – and for the severity in this case, perhaps Methadone.
For sleep, amitrptyine would be useful and if not effective, perhaps Zanaflex or nabilone (a synthetic cannabinoid) could be useful.
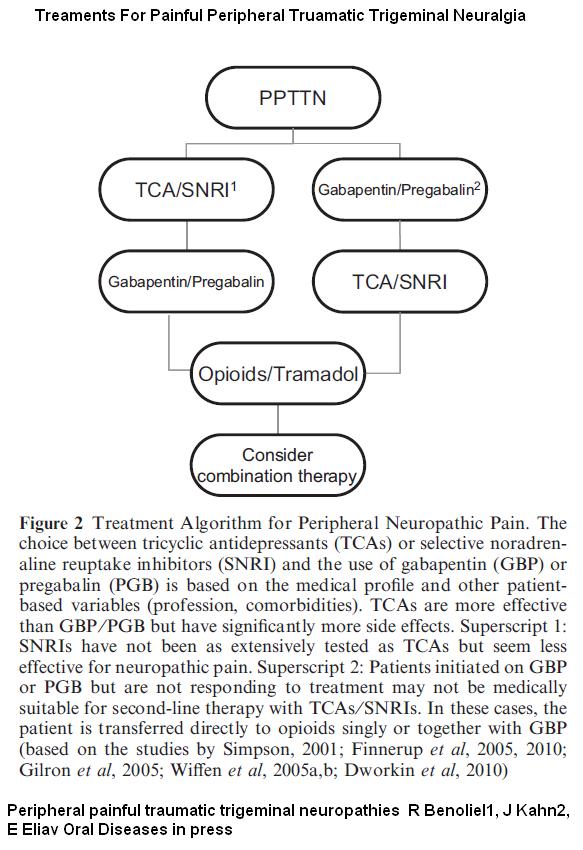
An article in Press gives a potential algorithm for treatment:
Peripheral painful traumatic trigeminal neuropathies
R Benoliel1, J Kahn2, E Eliav
Oral Diseases in press (excellent review) abstract here
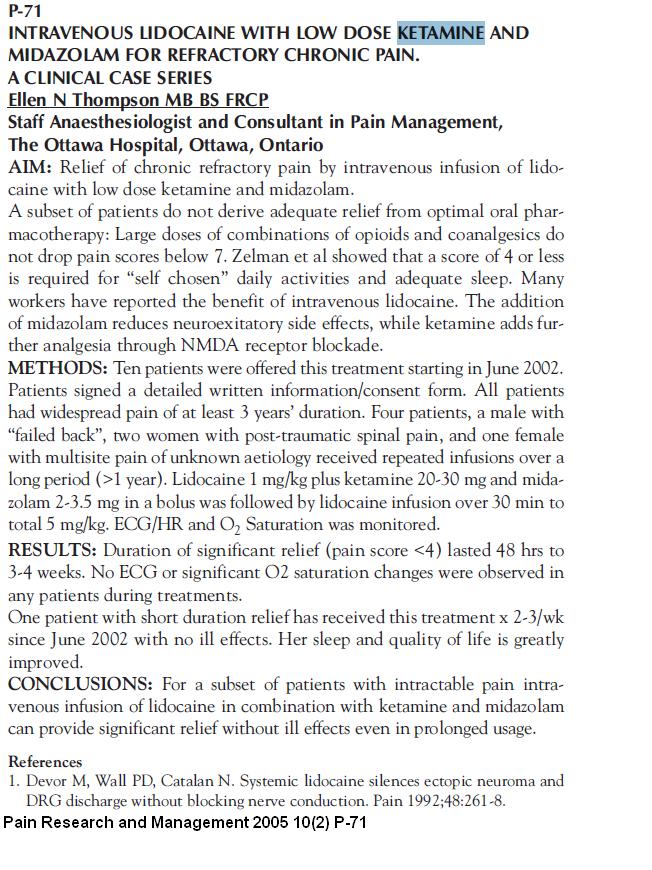
For the desperate:
IV lidocaine infusions give 1-3 days relief (get it done in the leg veins – it’s hard on veins)
Ketamine 10-15 mg IM in deltoid – 3 doses 15 minutes a part will give you 2-3 days relief of pain and depression but you have to have continued access otherwise you relapse.
INTRAMUSCULAR (IM) KETAMINE FOR TREATING MIGRAINE AND NEUROPATHIC PAIN IN THE CLINIC
John Claude Krusz, PhD, MD, Stephanie Hall, BS, MPH, Jane Cagle, LVN
Anodyne Headache and PainCare, Dallas free poster here
One bright lady found she could combine the 2 and get a week + relief:
Motor cortex Brain Stimulation – Electrodes are placed over the motor cortex on the surface of the brain – a relatively simple procedure as you do not have to go into the brain:
Motor Cortex Stimulation for Central and Neuropathic Facial Pain: A Prospective Study of 10 Patients and Observations of Enhanced Sensory and Motor Function during Stimulation
Brown, Jeffrey A. M.D.; Pilitsis, Julie G. M.D., Ph.D.
Neurosurgery: February 2005 – Volume 56 – Issue 2 – pp 290-297 abstract here
- Helped half of cases and reduced pain over 50%
- There were some potentially serious side effects – one had a medullary stroke leading to more pain and one had more pain for no reason; 2 were not helped.
- The technique seems to have improved with only a few cases of seizures mentioned:
Summary:
Brown and Pilitsis 8 cases – 75% relief
Nuti et al. 31 cases 39.2 % relief
Velasco et al. 8 cases 63.25% relief
Still working out to about 50% relief…
This is a work in progress – I will put down other ideas as they come to mind…
Addendum:
I’m assuming there has been a complete worked up:
- Diabetes would complicate the situation and needs treatment
- Smokers – I have written blog notes about how smokers are 1.5 – 2.0 times worse off. The worst- resistent cases I have are all smokers. New patients of mine who are smokers are put on 3 months probation – they either quit (and there are drugs to help) or I will not continue to see them…
- Deficiencies – If vitamin B12 is low, supplementation will help. If Vitamin D levels are low, supplementation may help.
- If iron ferritin levels are low, chronic pain is much more likely – and these cases are much more likely to have restless legs:
Subjects with thalessemia minor with low ferritin are 3X more likely to have chronic pain:
Clinical Rheumatology 27(9), 1103-1108,
An increased prevalence of fibromyalgia in iron deficiency anemia and thalassemia minor and associated factors
Gülsüm Emel Pamuk et al
and
Ferritin levels below 50 ng/ml associated with a 6.5 times risk of developing fibromyalgia:
European Journal of Clinical Nutrition 64, 308-312 (March 2010).
Association between serum ferritin level and fibromyalgia syndrome.
O Ortancil et al
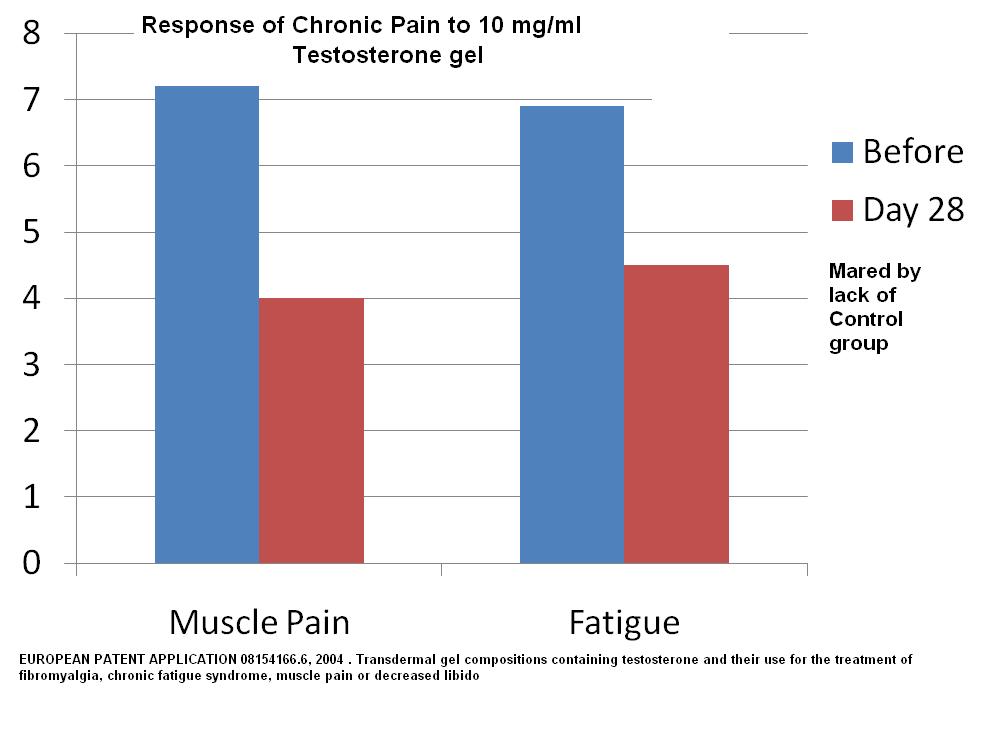
the connection between low iron ferritin and chronic pain is not clear but part might be related to fact some of these subjects are occult celiac cases needing treatment. - Low testosterone in women with chronic pain is 100% – I test levels and they are unmeasurable – I suspect lack of sleep drives them down (is low in sleep apnea). Supplementation helps and in one patent scenario – use of Testosterone gel 10 mg/ml (like Testim) gave significant results:
EUROPEAN PATENT APPLICATION 08154166.6, 2004 . Transdermal gel compositions containing testosterone and their use for the treatment of fibromyalgia, chronic fatigue syndrome, muscle pain or decreased libido:
In women I use 0.2-0.3 mls of testim gel/day – I give them a 1 cc needleless syringe to measure first dose. Again, like the frequent B12, I find it helps the background noise of pain and leaves subjects with more discrete pain issues that are easier to cope with. Testosterone gets partially converted to estrogen so helps night flushes in perimenopausal – however, a woman would need regular mammograms when on..
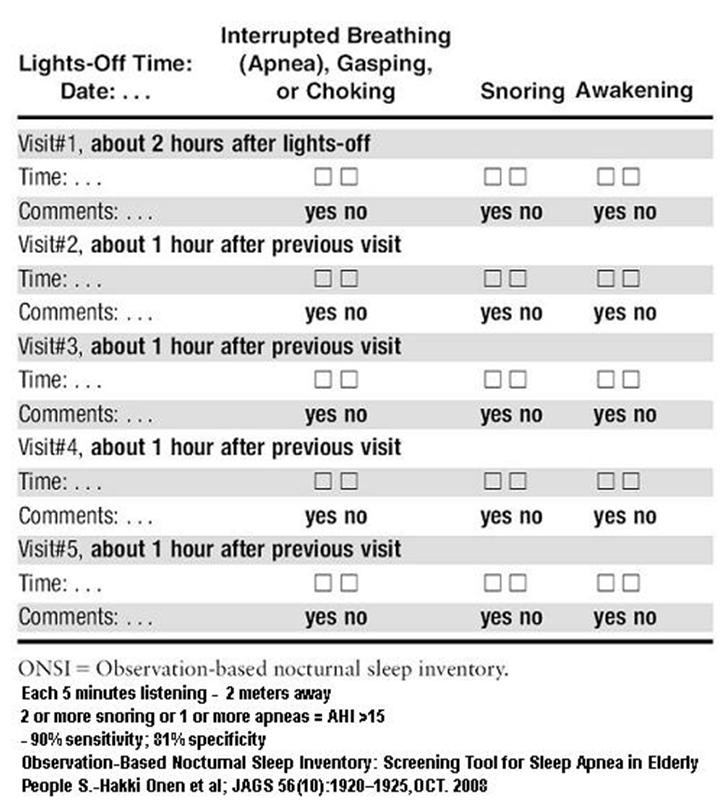
If short acting opioids help but long acting make you sick, then I would suspect you might have sleep apnea which long acting opioids aggravate during the night – I t doesn’t make sense that the same inigredient in long acting form should make any difference otherwise.. Here is a questionnaire to suggest it:
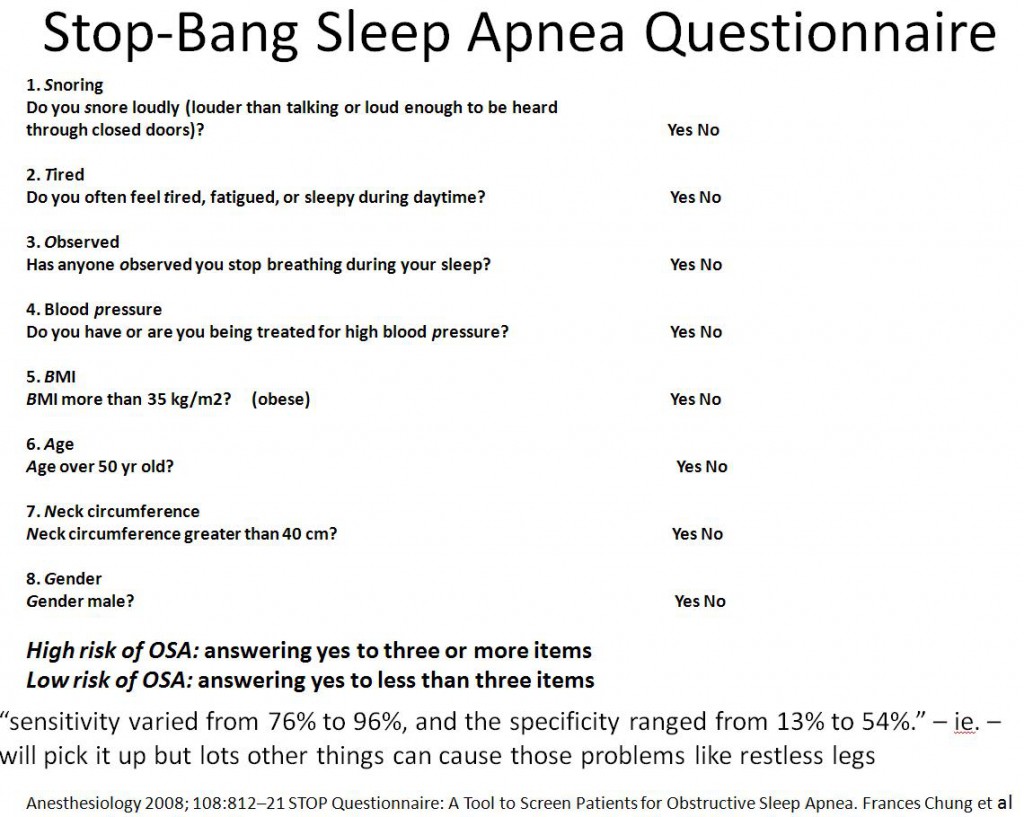
I would have your husband monitor your breathing during the night using the following template:
If positive, weight loss, a sleep apnea nightshirt, and a cpap machine might be in your future..
Short acting opioids are addicting and you will confuse the buzz with relief and crave that feeling – That is why they took oxycontin off the market… If you get depressed on long acting opioids, you should probably be on a SNRI type antidepressant anyway, and if you cannot tolerate it, S adenosylmethionine (SAMe) 400 mg 3 times a day(not cheap), EPA in Omega 3 supplement 1.2 gms/day, and DHEA 100 mg 3 times a day – herbals that have antidepressant properties.
I would appreciate input from people with more experience here…

Pingback: Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica? | Pain Medical Musing
My case is similar, but more of a horror story of a dentist who extracted 30 with a large cyst attached, then 31, broke my tooth sockets, stuffed unidentified cadaver bone in socket without my permission or a consent form, then lied about the cyst, etc………. for the money he could make and collaborated with the dentist who broke my teeth by doing him a favor at my expense……………later oral surgeries under general anesthesia, cracked teeth, nerve studies. No drugs as I chose not to be pharmaceutically controlled.
What finally worked after failed implant removal was Acupuncture with electric stime, by a Neurologist. Be patient the first 14 or 20 treatments with relax you and ease the daytime pain………..later more treatments and my sleep improved. It works.
what made me feel better was revenge since no lawyer would take the case since its just not a good buisness decision as winners are loosers in court with measly settlements. I spent over 35,000. K of my savings, and it destroyed my eyesight………… and my husband became my caretaker. But at least now even if I loose the court case if public information with all their lies on PDF public docs at a PA court of common please.
My case is similar, but more of a horror story because the dentist injured me intentionally, he extracted 30 with a large cyst attached, then 31, broke my tooth sockets, stuffed unidentified cadaver bone in socket without my permission or a consent form, then lied about the cyst, etc………. for the money he could make . He also collaborated with the dentist who cracked my teeth 28 1nd 29, later root cannaled, by doing him a favor by removing them, then informing him of his successful removal of 2 cracked teeth, at my expense……………later oral surgeries under general anesthesia, nerve studies. lots of ice, no sleep, permanent crippling pain, no drugs as I chose not to be pharmaceutically controlled. i lost a great deal of my eyesight from the pain and hypertension increasing my macular degeneration.
What finally worked after failed implant removal was Acupuncture with electric stime, by a Neurologist. I can almost function normally, with some continued nightly pain. Be patient the first 14 or 20 treatments with relax you and ease the daytime pain………..later more treatments and my sleep improved. It works.
I spent over 35,000. K of my savings, and it destroyed my eyesight………… my husband became my caretaker. The case dockets on both dentists with their medical records, along with all my docs Ctscans and digital data, is filed in the public access court system of Bucks County Pennsylvania. Its public information now and will continue as long as I can hold out as a Pro Se plaintiff against 2 huge law firms…………one listing 35 lawyers.
I believe what you said made a lot of sense. But, what about this? suppose you added a little content? I am not suggesting your content isn’t solid., however suppose you added a headline that grabbed a person’s attention? I mean Chronic Facial Pain Needs Help | Pain Medical Musing is a little vanilla. You could look at Yahoo’s home page and watch how they create news headlines to grab viewers to open the links. You might add a related video or a related picture or two to get people excited about what you’ve got to say. In my opinion, it might bring your posts a little bit more interesting.
Thanks for sharing, this is a fantastic blog post.Really looking forward to read more. Want more.
I blog quite often and I really thank you for your information.
This article has really peaked my interest. I will book mark your website and keep checking
for new information about once per week.
I subscribed to your RSS feed too.
Pingback: Facial Swelling After Root Canal In Austell Ga | Atlanta Root Canal