Article in press reviews literature and treatment measures for osteitis pubis

Treatment of Osteitis Pubis and Osteomyelitis of the Pubic Symphysis in Athletes: A Systematic Review
Haemi Choi, Michael McCartneyThomas M Best
Br J Sports Med in press abstract here
- Type of groin pain in midline lowest abdomen – either groin or pelvic pain
- Factors involved:
- Athletics involving sprinting, kicking, twisting, and cutting – this means soccer, football, ice hockey, running and rugby – apparently without much history of trauma
- Urinary tract infections – had one case with a UTI that remitted some once the infection was treated
- Associated with orchiaglia – painful testicles – had a case that required injection of ilioinguinal and genitofemoral nerves, and pubic joint to remit his pain;
- Associated with pregnancy when those joints become very unstable anyway
- Rheumatic diseases – Rheumatoid arthritis, and more interestingly, Ankylosing spondylitis.
In:
Resnick, D; Dwosh, I L; Goergen, T G; Shapiro, R F; Utsinger, P D; Wiesner, K B; Bryan, B L.
Clinical and radiographic abnormalities in ankylosing spondylitis: a comparison of men and women.
Radiology. 119(2):293-7, 1976 May.
found 61% of women with Ankylosing spondylitis had this – often the were HLA B27 positive. - Variety of lower abdominal, urologic and gynecologic surgeries – prostatectomy, cystectomy, transrectal prostate needle biopsy, abdominoperineal resection and inguinal hernia repairs.
- pregnancy: came across a link that discusses this: here
- Question is whether this is a localized form of Complex regional pain though there is suggestion of blood flow abnormalites to area as well.
Symptoms:
- Symptoms may occur 1 to 8 weeks after the triggering event. The primary symptom of pain varies in severity and duration.
- pain in the pelvic region with extension to the inner thighs – may bve abrupt onset .
- aggravating factors could include coughing, sneezing, micturition, defecation, walking, sitting, getting up to standing, and stairs.
- May “waddle” from pain and a sensation of tightness in adductors.
Signs:
- Local tenderness would be the big one.
- palpable or audible click over area
- adductor spasm leading to reduced hip abduction (swinging out)
Differential Diagnosis:
- Sacroiliac (SI) disease – with SI instability you can find one pubic ramus higher than the other. A simple exercise can help distinguish: With knees separated try pushing them together with either you wrist to elbow or a beach ball separating them. Then hold your knees together and try separating them. Repeat three times and then check to see if pubic pain has resolved. This sort of instability might require an SI belt or prolotherapy, recently been found helpful in a British study of SI disease.
- Osteomyelitis of the pubic symphysis – more sudden onset, fever, and more sick.
Treatment:
- Special compression shorts:

From: http://bracesupport.com/compress/pelvic-shorts.htm
though I am sure there are plenty of other sites
McKim K, Taunton J. The Effectiveness of Compression Shorts in the Treatment of Athletes with Osteitis pubis. NZJSM 29:70-73
“VAS scores for pelvic and groin pain were significantly reduced while wearing compression shorts during exercise, however no improvement in athletic performance was noted.”
- Antiinflammatories – Ibuprofen 800 three times daily, and indomethacin 25 mg were two mentioned specifically
- cryomassage (fill a styrofoam cup with water, freeze, peel down the rim and massage like deodorant stick over area)
- massage, trigger therapy – The pyramidalis muscle can be sore and has been shown to contibute to pelvic pain:
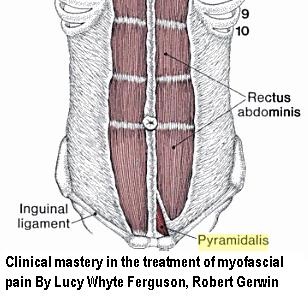
In:
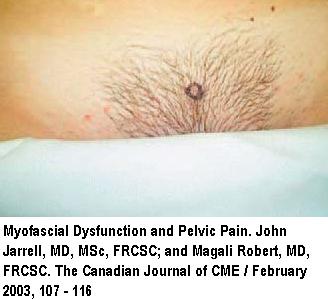
Myofascial Dysfunction and Pelvic Pain
John Jarrell, MD, MSc, FRCSC; and Magali Robert, MD, FRCSC
The Canadian Journal of CME / February 2003, 107 – 116 free article here
They injected a pyramidalis associated with pelvic pain:
Hip adductor muscles will also need work
- physio – laser, ultrasound
- Steroid Injections – I think this should be the first choice unless the joint is obviously unstable. in one metanalysis, 58.6% of athletes were able to return to sports following use after an average of 8 weeks. 20.7% were complete non-responders.In another study:
Symphyseal Cleft Injection in the Diagnosis and Treatment of Osteitis Pubis in Athletes
Martin J. O’Connell, Tom Powell, Noel M. McCaffrey, Denis O’Connell, Stephen J. Eustace
AJR:179, October 2002, 955-959 free article here
“Fourteen (87.5%) of the 16 patients experienced immediate relief of some of the symptoms
and were able to resume sporting activities 48 hr after the procedure.” There was some relapse however, later.I use 40 mg Kenalog plus local. The cleft will only hold 1 – 1.5 mls fluid so no point on using large volume. One steroid injection protocol Here Osteitis Pubis Treatment & Management
One steroid injection protocol Here Osteitis Pubis Treatment & Management
– Inject in middle of the pubic symphysis in an AP (front-back) direction.
– Insert in “approximately 1 inch until a pop is felt as the needle enters the joint.”
– “The author’s suggested preference is to use a 1.5-inch 20-gauge needle with a 3-mL syringe that is filled with 1 mL each of betamethasone injectable suspension (6 mg/mL), 2% lidocaine, and 0.5% bupivacaine. )”. Agian, I use a 25 guage 1 inch and use kenalog 40 (I let the steroid settle out, discard the supernatant, suck up the steroid precipitate and mix with 1 ml local)
– “Postinjection, the patient remains out of activity for 1 week.”
– “Occasionally, a second or third (rare) injection is required at intervals of 2-3 weeks.” - Prolotherapy:
- As per:
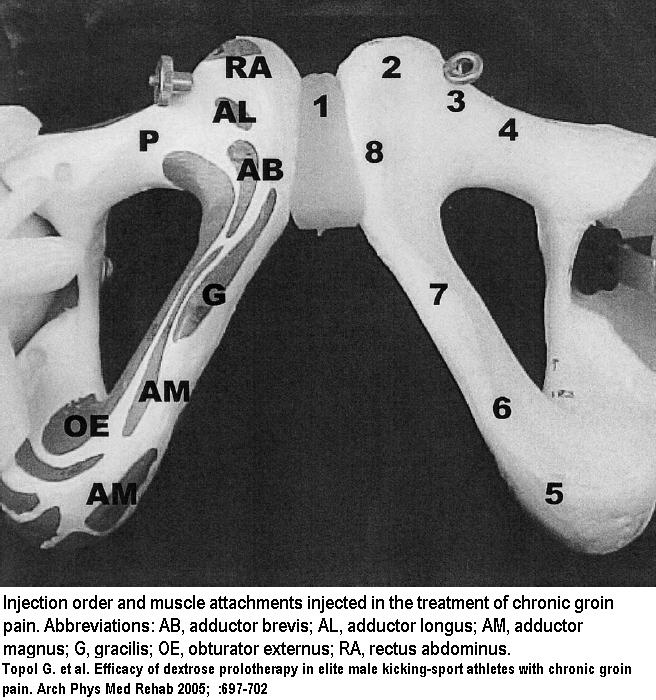
Topol G. et al. - Efficacy of dextrose prolotherapy in elite male kicking-sport athletes with chronic groin pain. Arch Phys Med Rehab 2005; 86:697-702 abstract here
-
- 24 male athletes – average symptoms duration 15.5 months
- monthly injection average 2.8 injection (2-6)
- mixing 8mL of 1% preservative- and epinephrine-free lidocaine with 8mL of 25% dextrose solution in a 20mL syringe
- pubic symphysis – 23-gauge needle at a depth of 2 to 4cm – 2 mls
- points 2-4 along pubic rim 1 cm apart – 1 cc each – covering the pectineus origin and pyramidalis insertion and external oblique insertions. “the needle was directed off the edge to confirm location at the top of the rim, and then the needle was redirected back onto bone for the injection.”
- ischiopubic ramus (points 5–8), covering attachments of the adductors – this hits adductor magnus, gracilis, adductor brevis, adductor longus origins, and the insertion for the rectus abdominis on the pubic tubercle. -have patient extend opposite leg. Hold injected leg flexed and externally rotated with the foot against the opposite leg – 1 ml each
- It gets complicated:
– “For injection into the ischiopubic ramus, the needle entry was in a caudocephalad direction to ensure a better sense of distance from the midline. – The line of needle insertion points was vertical rather than angled to ensure that bone contact occurred rather than the needle falling off bone medially at first insertion.
– The depth of injection was similar for each ischiopubic ramus injection site and the typical distance off midline for entry in ischiopubic ramus injections was about 4cm. Due
to tissue depth, it was sometimes necessary to use 2 fingers, 1 on each side of the needle, to indent the soft tissue to allow needle contact with bone. However, this was done without skin traction to avoid altering mediolateral orientation.” - Picture of lower injections points done:

- After 9 weeks from 1st injection, 91.7% were able to return to sports; 8.3% failed to respond.
- Recent article that goes over this technique available free :
Regenerative Injection of Elite Athletes with Career-Altering Chronic Groin Pain Who Fail Conservative Treatment A Consecutive Case Series
http://prolotherapy.com/Topol_Regenerative%20Injection%20of%20Elite%20Athletes%20with%20Career-Altering%20Chronic%20Groin%20Pain%20Who%20Fail%20Conservative%20Treatment_2008.pdf
Surgery Includes:
- curettage of the pubic symphysis – 72% success
- polypropylene mesh placement into preperitoneal retropubic space – 92% success and fastest return to sports (7.2 wks)
- pubic symphysis stabilization – 100% results minus one drop out
Scrotal bruising and intermittent swelling only side effect.
Comment – I have never had to go beyond steroid injection. The prolotherapy seems intensive but if you are desperate, it works.
Addendum –
EFFECTIVENESS OF METHYLPREDNISOLONE INJECTION TO PUBIS SYMPHYSIS IN POST PARTUM PUBIS SYMPHYSIS DYSFUNCTION:FOUR CASE REPORTS
C. Fernando
IASP poster DM 397. Montreal 2010
- 4 women with severe post-partum pubic symphysis dysfunction
- Depo-medrol 40 mg and 1 ml of 0.5% Bupivacaine injected resulted in rapid relief
Addendum – steroid injections
Br J Sports Med. 2010 Nov 3. [Epub ahead of print]
Treatment of osteitis pubis and osteomyelitis of the pubic symphysis in athletes: a systematic review.
Choi H, McCartney M, Best TM abstract here
- “It is thought that osteitis pubis is caused by repetitive twisting/cutting manoeuvres with stress at the pubic symphysis from restrictive hip movement.”
- “Imbalances between the hip adductor and abdominal muscles have been thought to contribute
in the development of osteitis pubis.”:
(ref – Fricker PA, Taunton JE, Ammann W. Osteitis pubis in athletes. Infection, inflammation or injury? Sports Med 1991;12:266–79.) - “an active rehabilitation programme assisting “the coordination and strength of muscles that act on the pelvis” helps in chronic groin pain
(ref – Wollin M, Lovell G. Osteitis pubis in four young football players: a case series
demonstrating successful rehabilitation. Phys Ther Sport 2006;7:153–60.) - Review of cortisone shots found people had average of 1.24 shots – range 1-3 – no consisent mix
Addendum – neagtive steroid case where instability may have been more an issue
Pain Med. 2011 Nov 14. [Epub ahead of print]
A Retrospective Study on the Efficacy of Pubic Symphysis Corticosteroid Injections in the Treatment of Pubic Symphysis Pain.
Fitzgerald CM, Plastaras C, Mallinson T. abstract here
- In cases to this tertiary center, and where 7/10 were post pregnancy cases, Injections of steroid did not work
- Comment – Instability would be a big issue (and more severe to make it to a tertiary center)and prolotherapy with or without platelet rich plasma might be a better place to go
As a matter of fact, in the non-athlete, conservative measures by themselves work in most cases:
Open Orthop J. 2011;5:331-4. Epub 2011 Sep 12.
Treatment of osteitis pubis in non-athlete female patients.
Kavroudakis E, Karampinas PK, Evangelopoulos DS, Vlamis J. free article here
Addendum – platelet rich plasma success
PLATELET RICH PLASMA AND MSK TREATMENTS
Dr. Erik Ouellette in Vancouver 2011 CAOM
- Case of 17 year old with pubic tenderness for 6 months – could not play hockey
- Tenderness to Symphysis pubis , right Iliolumbar ligament and right Posterior sacro iliac ligaments.
- Rx – Manipulation, stretch adductors
- Platelet rich plasma to Symphisis pubis, Ilio lumbar and posterior sacro iliac ligaments
- 3 treatments at 4 weeks intervals
- Results – Could participate to off ice training after 1st; Could participate 85% activities after 2nd; Back to play without pain after 3rd
A 2014 study confirmed that IV pamidronate (a bone building IV med that works on the bone edema that is often presents) can work well if given at least 3 times in my opinion:
Treatment of Resistant Osteitis pubis with Pamidronate
http://painmuse.org/?p=3857
Addendum:
A severe post pregnancy case was treated with a spinal stimulator:
J Pak Med Assoc. 2012 Jan;62(1):71-3.
Management of chronic symphysis pubis pain following child birth with spinal cord stimulator.
Idrees A. Department of Anaesthesia & Pain, Our Lady of Lourdes Hospital, Drogheda, Ireland. abstract here
- “Incidence of [actual] diastasis (defined as abnormal wide gap greater than 10mm between the two pubic bones) of pubic symphysis following child birth is very low and varies from 1 in 600 to 1 in 3400 deliveries” (Normal disatnce in pregnancy 4-5 mm)
- 39 year old with a 21 mm gap
- Pains 7/10 despite multiple meds – neuropathic in nature
- Lidocaine infusion gave relief for a few days – confirming more likely neuropathic
- Peripheral nerve stimulation procedures SENS (Subcutaneous Electrical Nerve Stimulation) – did not work
- “spinal cord stimulator with dual octrode leads were put in at T10 level” – gave complete relief
- pubic symphysis innervated by genitofemoral (L1-2) and pudendal nerves (S2-4)
- states “Conservative management include pain medications (e.g. NSAIDs and Opioids), strict bed rest, use of pelvic binders or braces, later on physiotherapy and pelvic exercise” . No mention of what exercises though.
- Does look like a spinal stimulator could be considered in neuropathic cases – ie good response to lidocaine infusion temporarily.
Any other treatments or comments?

I have been suffering from osteitis pubis since dec 09 but it wasn’t diagnosed till aug 27 /10 by a WCB doctor in winnipeg. The doctor examined me for maybe 5 – 10 m in then said osteitis pubis.. for treatment he recommended i return to my job underground mining as a diamond driller and put restrictions at exactly what the job says it demands lifting 50 lbs..
I complained that i was unable and they said it will be a trial period..and wouldn’t offer physio, I said my reserch of osteitis reccommends physio and they said the opposite but if i could find a specialist that would say it in writing they would consider.. the pain was too much for me to handle after 7, 8 hour shifts i feel i have damaged myself possibly even more than the original injury…i am a typical case of wcb doctors causing more problems by forcing the worker back to work with unrealistic healing pracitces.. I was not offered physio and even told by the dr that it was unavailasble in my area.. which ended up being untrue… iam currently in great pain and have hip problems as well… any advice..
Dr. Hayes cured my osteitis pubis.
http://www.drbradhayes.com/bradhayes/staff.asp
The technique took 10 minutes, I could then walk up and down stairs without pain.
So sorry for your pain.
admin says:
You can manipulate the pubic joints by pushing your knees together with a beach ball or your hand to elbow between knees. Sacroiliac torsions and upslips could put strain on pubiis and correcting them could help temporarily. Could you describe what you had done? I am reluctant to advertize names but can’t knock success…
Scott,
So sorry to hear you are suffering BUT there is HOPE! See a chiropractor, one specializing in ART therapy (active release). Google that, there are several in Winnipeg. Give it time too. It is said that it takes 1 – 3 years (average of 9 months to resolve) with just taking NSAIDS. (Be careful though as I now have an ulcer from taking too many pain meds over the year).
Doctors really don’t know much about this as it is a rare condition in Canada. Much more prominent in countries such as Norway (where women are genetically predisposed to cartilage disorders (I’m 25% Norwegian – how ironic), and in Australia where kicking sports are played frequently). If you get desperate enough, Gary Mitiris is a physiotherapist that treats this in Melbourne, Australia. Several people rave about him on the net and you wouldn’t be the first Canadian to shell out your life savings in hopes for a cure. I actually emailed him and he responded but said he would have to actually see me to treat me and did not feel comfortable giving tips to my chiro.
You should definently NOT be lifting anything heavy. Can you request “light duty” or a desk job? I am also suffering this hideous condition. There is a clinic in the city called Natural Pain Solutions (Dr. Cesear) that does prolotherapy. I’m thinking of trying it, but a little leary as I am doing heaps better and don’t want to have a set back or spend money unnecessarily. From what I’ve read, I think the ART therapy is your best shot. Prolotherapy is said to work 80% but in some cases only temporarily and it depends on the dammage done.
Have you had a “stork” exray (plain radiograph in which one leg is positioned like a stork” to show sclerosis or instability in your joint? Note: A regular exray of your pelvis will likely show nothing. I have a 6mm gap and instability while bearing weight on my left leg (0-1mm is normal and those over 10mm need surgery with a steel plate). What about a bone scan to show inflammation of your pubic symphysis? Maybe you need to see a different doctor, perhaps at the Pan Am Sports Clinic? If I lived here, I would have tried that first.
I live 8 hours away from Winnipeg and was very fortunate to have a chiropractor in my small town that knew about this (after my obgyn basically told me the pain was in my head and all the other doctors I ran accross had no clue and some even said maybe it was because I was anxious (They’d be “anxious” too if no one knew why they couldn’t walk and were still responsible for caring for thier child…. all the lifting!- Be very fortunate you are a man, as I am sure your pain isn’t belittled. My husband even had to take three months off of work to help care for our 8 month old. I still am so angry towards some of those docs. That being said, you need a second opinion. You need to see an orthopedic surgeon as well for a proper diagnosis, although Dr. J Engel was the locum I saw and he was little help which is probably a good thing as he didn’t try to talk me into a surgery. If it is severe the osteopath will suggest surgery.
Now for the positive: You WILL get better. Maybe not 100% ever, but it will get better. Last Christmas I couldn’t even go grocery shopping or lift my son without wincing. Now I can get around no problem, but do still get stabbing pains and groin/lower abdominal discomfort, but it is milder and I don’t need NSAIDs all the time anymore. I haven’t had the opportunity to do the ART therapy but my chiro does dry needling in my adductors (HUGE HELP) which is also active release, and I can have several days in a row without major pain. Good luck and stay positive.
Hi Soremamma and Scott,
I am sorry to hear about your pain. Did the ART treatment hurt? I have been doing physio but it has increased the pain, so I am concerned it may be doing more damage. From what I hear of Garry Miritis in Australia he sounds like a miracle worker! I am looking for treatment in Canada, i will post what I find out.
Best wishes, Cynthia
try acupungert, it worked , no more sore pubic bone, but still tightness in inner thigh area, slowly getting better with pysotheropy. sorry for the bad spelling.
Hi, I’m 22 and have Osteitis Pubis for 5 years. I played alot of sport (tennis and Basketball) so thats probably where it came from. Was only diagnoesed last year, because I have had it so long it was quite severe. I have seen so many physios/osteos/doctors but none of this was working, ended up needing surgery which i had 5 months ago and still in alot of pain. I have a great surgeon and he says the bone is healing well, but the cartidge inbetween the joint is not healing the way it needs to so he is now in the process of giving me platlet injections. This is a new kind of treatment from what i know with good results, but I am still feelin pretty bad and not sure if they will work. I can’t work and can’t be up for more then 2/3 hours. So i spend alot of time lying down resting. Does anyone know of these platelet injections or anything about them? If they don’t work i think I’m looking at another operation to fuse the joint!! Thanks for everyones posts!
Hi Hannah,
How did your PRP go? did you have a series of 3-4 injections ?
I have been suffering with the same condition for 3yrs now , I am sick to death of the pain and having to put my life on hold . I have 3 young children .To date I have had 3 mri and 3 x ray plus a year and half of physio and other treatment .I have to use walking aids to get around . I am currently thinking of surgery but I am scared in case it doesn’t help please help
————-
Your condition sounds tragic. The severity you have makes me want to know several things:
1) Do you have a back ache, morning stiffness, and chronic fatigue – all pointing to a subclinical ankylosing spondylitis. This issue might show up in a bone scan…
2) Is there bone edema obvious on MRI? – this is tissue swelling in the bone – common and associated with pain.
Both these conditions respond to IV biphosponates like pamidronate – a bone building drug that also has anti-inflammatory properties.
-Used in Osteitis pubis longstanding from unkown or inflammatory cause:
J Rheumatol. 2001 Dec;28(12):2754-7.
Treatment of refractory symphysitis pubis with intravenous pamidronate.
Maksymowych WP1, Aaron SL, Russell AS.
http://www.ncbi.nlm.nih.gov/pubmed/11764231
2 cases of unknown cause got better; one cause of known arthritis got better.
– Use in Bone marrow edema (internal swelling in the bone):
bone marrow edema is common in osteitis pubis. Bone marrow edema in other areas has responded to biphosphonates (of which pamidronate is a member):
Rheumatol Int. 2013 Jun;33(6):1397-402.
Bisphosphonates or prostacyclin in the treatment of bone-marrow oedema syndrome of the knee and foot.
Baier C1, Schaumburger J, Götz J, Heers G, Schmidt T, Grifka J, Beckmann J.
http://www.ncbi.nlm.nih.gov/pubmed/23143557
They found: “Regarding bisphosphonates, four patients described pain release after the first infusion, another three after the second treatment and another two not until the third application,
leaving one non-responder in the bisphosphonate treatment group.”
In order to use a biphosponate, you have to have decent teeth as it can rarely cause bone loss in the jaw.
It was monthly in both cases
In the former pamidronate 60 mg in 250-500 mls saline/D5W over 4 hours.
In latter, “Ibandronate was administered once monthly in a dosage of 6 mg for three consecutive months.” – this drug is not available in Canada so you are stuck with pamidronate monthly.
People who use biphosponates must be prepared to feel sick and achy (flu-like)for up to a week after so not for the faint of heart.. Rarely, it can induce a hip fracture.
It has gotten considerably cheaper since a generic form is available so don’t get name-brand..
There is a new study that confirms its benefits even with inadequate amounts:
Treatment of Resistant Osteitis pubis with Pamidronate
http://painmuse.org/?p=3857
Hello,
It’s been a while since anyone posted here, but because I came across this in my research, I thought I’d add to the string.
Two good resources in the US for groin pain are Dr. Bill Brown in Fremont, CA. and Dr. Meyers at the Vincera Institute in Pennsylvania.
Best of luck.
Ik wil heel graag mijn verhaal kwijt.
Ik ben een 55 jarige vrouw en woon in Nederland.
Toen ik 19 jaar was heb ik een auto ongeluk gehad met aktie aan rechter boven been ,richting osteitis pubis.
Na 4 zwangerschappen en natuurlijke bevallingen.
Altijd veel pijn ,voelde zwaar,gloeiend en vermoeid.
Na verschillende artsen,fysiotherapeuten en manuele arts eindelijk een orthopeed die een mri aan ging vragen.
Daarop was te zien dat er veel onrust was.
Ik heb een injectie gehad en 6 weken onbelast in bed.
Nog 6 weken herstellen.
Klachten zijn gebleven.
En ben ik geopereerd.
Deze operatie heeft een lang herstel nodig maar DE pijn die ik had is eindelijk na 30 jaar weg!
I really want to share my story.
I am a 55 year old woman living in the Netherlands.
When I was 19 years old I had a car accident with action on the right upper leg, towards osteitis pubis.
After 4 pregnancies and natural deliveries.
Always a lot of pain, felt heavy, glowing and tired.
After several doctors, physiotherapists and manual doctor, finally an orthopedist who was going to request an MRI.
It showed that there was a lot of unrest.
I had an injection and 6 weeks without weight in bed.
6 more weeks to recover.
Complaints have remained.
And I have had surgery.
This operation needs a long recovery but THE pain I had is finally gone after 30 years!