Listened to talk by Dr. Anthony Kaufman.He does probably the largest amount of Trigeminal nerve microvascular decompressions in Canada (~50/year) and helps run the Winnipeg Centre for Gamma Knife Surgery.
He has a web site with detailed descriptions here
Here are some points made:
1) Defined as sharp severe instantaneous jabs on one side of face.
Takes several years to diagnose and efforts often misdirected
Dental – root canal or extraction
TMJ arthritis
Temporal arteritis
Headaches/Migraines
Head/Neck ca
Chronic Otitis Media
Shingles
Psychiatric – hard to believe could be considered such but I had a patient with glossopharyngeal neuralgia (jabs in neck when swallow) spend time in a psychiatric ward before she saw me and was put on Tegretol (language difficulties).
2) Cause primarily vascular irritation (90%) from nearby pulsing vessel. MS and trauma are two other frequent causes. Triggering events include dental work or facial injury in 1/3 cases.
3) Some cases have a component of atypical facial pain – constant achy component. This might amount to a neuralgia – severe form of constant pain or atypical facial pain – a poorly understood lesser pain. Given that this group has a neuropathic (nerve damage) component, they do not do well with procedures that damage the nerve more.
4)Investigation involves plain MRI (dye enhanced only for MS or tumor cases). 90% of time can see compressing blood vessel. 5%+ time small vessels not seen. One can do CISS sequence procedure to do millimeter slices of area on film.
5) Medications include Tegretol (Carbamazepine) – useful and cheap so used first but most have some side effects from (drowsy, drugged, unsteady). Neurontin (gabapentin), Dilantin, and Lyrica are alternatives. I asked re oxycarbamazepine (Trileptal) which is a type of tegretol with less side effects. It is expensive and like our Saskatchewan plan, the Manitoba plan will not cover it. Baclofen, a central acting muscle relaxant used in MS etc., is sometimes used but only as an add-on. Adding two drugs otherwise is NOT worth-while and doctors are discouraged from attempting it and it just multiples the side effects. Medications will only worth 1/2 of time. More description here
Drugs used as described by:
Trigeminal Neuralgia:Diagnosis and Treatment;William P. Cheshire,
Current Neurology and Neuroscience Reports 2005, 5:79–85
Carbamazepine – often 100 mg 2-3 times daily works. Typically 300 – 800/day maintenance. Helps 80% initially but decreases to 50% over time
Dilantin – 200 – 400/day. Helps 60% initially but decreases to 25% over time.
Gabapentin (Neurontin) – half the efficacy of carbamazepine but more tolerable. Start with 100 mg three times daily and increase by 300 mg every 3rd day up to 2700 mg/day
Baclofen is started at 5 mg three times/day and increase by 10 mg EOD until 20 mg three times daily. Used more as add-on – efficacy disappears in 20% of responders.
Oxcarbazepine is started at 150 mg twice daily. It is “increased as tolerated by 300
mg every 3 days to a typical maintenance dosage of 300 to 600 mg twice daily.
Lamotrigine “started at 25 mg twice daily and increased slowly by 100 mg/d every 1 to 2 weeks, aiming for a daily dosage of 100 to 400 mg divided twice daily.” – found to help in a 14 case crossover study not relieved by carbamazepine and dilantin.
Topiramate “started at 25 mg twice daily, and the daily dosage may be increased by 25 mg every 3 days as tolerated to 100 to 400 mg divided twicedaily.” – promise in two pilot studies
“Sodium divalproex, clonazepam, and tizanidine have demonstrated at least limited efficacy in several small series.”
———
Other invasive techniques are discussed here
6) One alternatives includes various destructive nerve techniques . At their centre, they favour Percutaneous Balloon Compression Rhizotomy for destructive techniques. – A wired is fed up to the trigeminal nerve ganglion and a balloon inflated for one minute. Glycerol injection and radiofrequency denaturation are alternative destructive techniques. 10% are left with an unpleasant feeling in the face and a small proportion actually have pain there. About 50% will get full recurrence of pain, often within several years. Whatever the approach, medications work better on these recurrences that they did prior to surgery.
7) Gamma Knife surgery is an alternative that is becoming very popular because it is easy to do but the long term results are no better. 30% will end up with excellent results. 50% will need additional meds or another procedure after 3 years or so. Destructive effects of radiation may not become apparent for a year with progressive numbness.
8) Microvascular decompression – opening up area behind ear, lifting blood vessel from nerve, putting 6 tufts of teflon fibers between blood vessel and nerve. Although in one breath mentioned there were minimal side effects, did say side effects varied with how many procedures were done per year. Some of the sites doing surgery were Vancouver (24/yr), Calgary(11/yr), Edmonton (7/yr.), Winnipeg (over 50/year), and eastern Canada sites including Toronto, London-Ont., Mon?, and Halifax. Winnipeg did more procedures than anywhere else. Had one small recovered stroke and that was it – although 10% can gain some lifelong unpleasant feeling in face. Relief rates drop to 75% with time and 10% need more surgery.
9) Odd as it might seem, cases of prior surgery often do well with re-surgery, something he is in the process of publishing.
———–
What else can you do?
Injection of neurolytic strengths of local anesthetic can give some lasting benefit:
Pain. 1999 Jan;79(1):101-3. The long lasting effects of peripheral nerve blocks for trigeminal neuralgia using high concentration of tetracaine dissolved in bupivacaine. Goto F, Ishizaki K, Yoshikawa D, Obata H, Arii H, Terada M.
The management of trigeminal neuralgia in older patients who do not want neurolytic block and/or surgical treatment may be problematic. This paper describes three patients who had first and/or second division trigeminal neuralgia. The analgesic effects of infraorbital nerve block using 0.5% bupivacaine or 1% mepivacaine dissipated within a few days, however, the effects of nerve blocks using 4% tetracaine dissolved in 0.5% bupivacaine continued for more than 3 months. Hypesthesia was observed in two patients within a week following the block, but sensory level returned to normal within 2 weeks and there were no further complications in any patient.
Clin J Pain. 2001 Dec;17(4):323-6.
High-concentration tetracaine for the management of trigeminal neuralgia: quantitative assessment of sensory function after peripheral nerve block.
Radwan IA, Saito S, Goto F. Department of Anesthesiology and Reanimatology, Gunma University School of Medicine, Maebashi-shi, Japan. inasdr@med.gunma-u.ac.jp
OBJECTIVE: This study examined the effects of peripheral nerve block with high-concentration tetracaine for the management of trigeminal neuralgia, and evaluated sensory function by measuring the postblock current perception threshold.
METHODS: Five infraorbital nerve blocks were performed in five elderly patients using 4% tetracaine dissolved in saline or 0.5% bupivacaine. The authors used a neurometer to compare postblock current perception threshold between the block side and the contralateral healthy side, and used cold tests to assess the sensory level.
RESULTS: The analgesic effect of tetracaine blocks continued for a median period of 2 months (range, 1.5-months). Hypesthesia was observed in all patients after the block but resolved within a mean period of 2.2 weeks. Although differences in current perception threshold values between sides were not significant in any patient, block-side values in two patients were clinically higher than contralateral-side values (250 vs. 5 Hz) for some time before returning to normal levels.
CONCLUSION: Peripheral nerve block with high-concentration tetracaine is a relatively safe and useful technique in the management of trigeminal neuralgia, particularly among older patients and those with systemic problems.
You can get 20 mg Tetracaine powder for reconstitution. I dissolve it in o.5 mls spinal 5% lidocaine which makes it 4% tetracaine and 5% lidocaine.
5% liodocaine has neurolytic effects as well:
The use of 5% lidocaine for prolonged analgesia in chronic pain patients: A new technique . Regional Anesthesia and Pain Medicine , Volume 23 , Issue 1 , Pages 96 – 100Y . Choi , J . Liu
For mid- facial neuralgia, the infraorbital nerve can be injected. It can be found:
1) at pupil positioning vertically:
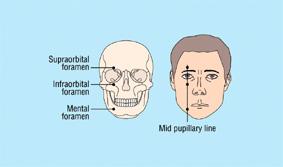
2) 5-6 mm under orbital margin although this could vary (see here)
another study states:
(in men) the mean distance between the infraorbital foramen and the inferior orbital rim was 8.5 ± 2.2 mm. In women, this was 7.8 ± 1.6 mm. as per here
Inject ON foramen not in. (Warning – intravascular injection could be hazardous and procedure best done in a hospital setting). Pulling back on syringe to see if in blood vessel is NOT reliable.
The mental block though I see it too is vertically in pupil line.
one found it 28 mm from midline and 14-15 mm from inferior bony edge
another found it 27.6 (22-31 mm) from midline and 12 mm (9-15) from inferior boney border.
as per here
You might be abole to feel foramen and as you hit it, patient will let you know it’s sore..
Supraorbital block with neurolytica strength local would result in unacceptable ptosis (lid droop).
Quite some years ago now, I used neurolytical local on a desperate elderly gentleman – worked so well had it repeated once and has been managed on minimal medication since.
Intra-oral plastic shield
There are some cases where there is an intraoral tic triggering zone. Putting medication under a plastic shield can have real benefits.
Diagnosis and Management of Trigeminal Neuralgia and Chronic Paroxysmal Hemicrania in a 43-Year-Old Woman – Oral and Transmucosal Pharmacologic Medications
G. Heir et al.
International Journal of Pharmaceutical Compounding Sept/Oct 2004; 8(5);337-343
- A plastic acrylic shield is fabricated “similar to a denture base that is custom-fitted to the soft tissue in the region. “
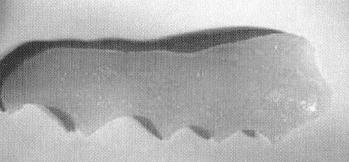
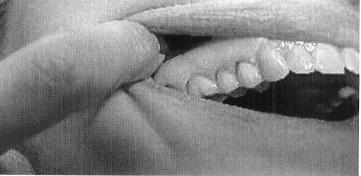
- “A thin coating of the medication was placed in the shell of acrylic and was applied to the target area, where it was held in place by adding Orabase to the PLO. Mixing this material into the compound gives it an adhesive property.”
- “Initially the compound was changed every 4- 6 hours.
- Usually 3 medications are used and can be varied depending on response. Possible meds include. (They do not give concentrations so here are values I think could be good)
- amitriptyline 2%
carbamazepine 2%
lidocaine 5%
capsaicin 0.02%
clonidine 0.2%
ketoprofen 10%
ketamine 2%
gabapentin 6% - “Within approximately 10 days the activity of the trigger zone was diminished and remained so for 2 week. The frequency of use of the compound was reduced slowly to twice daily and then discontinued after 8 weeks.”
- A variety of medication is made up in PLO gel and orabase added to make the shield stick when applied under it
Botox injection
Piovesan, E J. MD; Teive, H G. MD; Kowacs, P A. MD; Coletta, M V. Della MD; Werneck, L C. MD, PhD; Silberstein, S D. MD, FACP
An open study of botulinum-A toxin treatment of trigeminal neuralgia. Neurology. 65(8):1306-1308, October 25, 2005. abstract
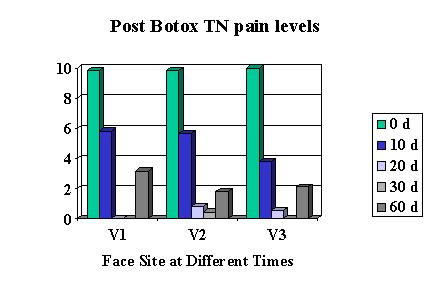 V1 received 6.83 units of BoNT/A, V2 received 6.45 units, and V3 received 9.11 units
V1 received 6.83 units of BoNT/A, V2 received 6.45 units, and V3 received 9.11 units
Basically it gave relief in 10 days and lasted over 60 days.100 units is $400; using about 1/10 that would be theorically $40.00 but you would need 10 patients lined up to use it all… The injection is intradermal – blebbed up in the skin so skin goes white as injected. – multiple sites. Now only if Botox would come out with the 50 unit vial they promised…
There is another form of botulinum: “The relative potency of BOTOX® units to Dysport units is approximately 1:4” ref here
Have used it on one patient with benefit – lasts 12 weeks to the day and then comes violently back. Make sure you have plans to give a repeat at 8-10 weeks to avoid that.
Another study used much more Botox:
Clin Neuropharmacol. 2005 Jul-Aug;28(4):161-2.
Botulinum toxin and intractable trigeminal neuralgia.
Türk U, Ilhan S, Alp R, Sur H. Department of Neurology, Dr. Lütfi Kirdar Kartal Research and Education Hospital, Istanbul, Turkey. uturkboru@hotmail.com
The effects of botulinum toxin have been demonstrated in pain syndromes such as migraine, tension headache, and postherpetic neuralgia. With this background data in hand, the authors planned a randomized, open-ended study to investigate the efficacy of botulinum injections in cases of refractory trigeminal neuralgia. In 8 patients with trigeminal neuralgia, 100 U botulinum toxin was injected into the region of the zygomatic arch. The results of their statistical analyses demonstrated that the medication can be effective in treating trigeminal neuralgia. The patients did not develop any significant adverse effects. Botulinum toxin can be used in the treatment of refractory trigeminal neuralgia.
Another study using the alternate form of botulinum used a vaery small dose:
Clin Neuropharmacol. 2002 Sep-Oct;25(5):260-2.
Beneficial effects of botulinum toxin type a for patients with painful tic convulsif.
Micheli F, Scorticati MC, Raina G.
Botulinum toxin is a well-known therapy for patients with diverse movement disorders. Its application has been extended to other disorders. Here, we document the case of a 70-year-old man with hemifacial spasm associated to trigeminal neuralgia secondary to an ectatic basilar artery. He was treated with botulinum toxin type A, 2.5 mouse units over five sites at the orbicularis oculi and one over the buccinator muscle. After botulinum toxin injections, relief was gained not only from twitching but also from pain. When the effects of the toxin vanished, spasms and pain recurred. Further infiltrations were given every 12 weeks following the same response pattern. This observation further validates the increasing role of botulinum toxin in pain management.
Another study confirmed its benefit especially if associated with hemifacial spasms:
Rev Neurol. 2006 Jun 16-30;42(12):729-32.
Painful tic convulsif and Botulinum toxin
Boscá-Blasco ME, Burguera-Hernández JA, Roig-Morata S, Martínez-Torres I.
INTRODUCTION: Painful tic convulsif is a rare disorder that associates trigeminal neuralgia (TN) and ipsilateral hemifacial spasm (HFS). These two disorders are the most common examples of hyperactive cranial rhizopathy and are frequently caused by vascular compression of these cranial nerves at the nerve root entry and exit zone in the brain stem, which leads to paroxysmal ephaptic transmission. CASE REPORTS: We report the cases of four patients with combined TN and HFS out of a total of 247 patients with HFS who were treated with botulinum toxin. One patient had TN that was contralateral to the HFS, while the other three were ipsilateral, and one of these had bilateral HFS. In all four cases both the HFS and the TN improved with botulinum toxin treatment.
CONCLUSIONS: These four patients with TN and HFS suggest a common aetiology for the two disorders, due either to central neuronal hyperactivity or to vascular compression of several cranial nerves. The beneficial effect of botulinum toxin in both disorders supports the idea of this toxin having a central mechanism of action that acts by controlling neuronal hyperactivity in the brain stem, as well as its peripheral action.
My Conclusion – Botox works and if one can figure out how to give a small amount economically (?leftovers) then could be cost-effective but must be given every 2-3 months
————–
Trigeminal neuralgia Emergencies
1) Intranasal Lidocaine 8%
Intranasal lidocaine 8% spray for second-division trigeminal neuralgia A Kanai, A Suzuki, M Kobayashi, S Hoka – British Journal of Anaesthesia, 2006; 276-277
“0.2 ml of lidocaine 8% applied to the sphenopalatine ganglion, which lies just posterior to the middle turbinate, provides effective pain relief for approximately 4 h.”
2) IV dilantin (fosphenytoin)
from: Trigeminal Neuralgia: Diagnosis and Treatment
William P. Cheshire,
Current Neurology and Neuroscience Reports 2005, 5:79–85
Usually a full loading dose of 14 mg/kg is required. Pain relief lasts 1 to 2 days, during which time
oral medication can be initiated and titrated, or arrangements can be initiated for surgical treatment.
Dr. Kaufamn suggested 100 mg quickly followed by 1 gm over ? 1 hour
3) Topical lidocaine (ibid Cheshire)
“Lidocaine, applied transcutaneously as a patch or intraorally in the form of viscous gel, or ophthalmic
instillation of 0.5% proxymetacaine drops, also may provide temporary relief”
Given that there is no Xylocaine patch in Canada, that means making up 5-10% lidocaine in lipoderm (Do not use PLO gel – will irritate the face too much)
4) Has suggested an anesthetist may need to be called to give ketamine & fentanyl until relief is achieved.
Addendum:
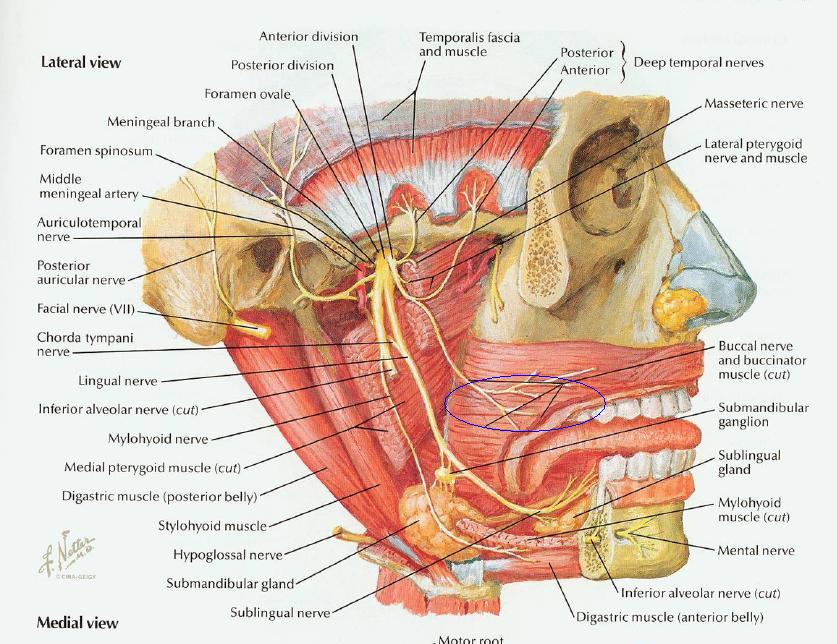
I found my semineurolytic injection into infraorbital and mental nerve did not help one pateint that continued to have pain lateral to his lip. I now realize ther is a third lower facial sensory nerve:
the buccal nerve:
He could not tolerate carbenazepine but finally settled on Oxycarbenazepine although the drug plan refused to cover it.

Pingback: Pain Medical Musing » Blog Archive » Botulinum / Botox for Neuralgia/Neuropathic Pain
my father lives in Thunder Bay and he has been suffering with trigenial neuralgia for 15 years! He is having difficulty being referred for treatment such as balloon compression rhizotomy, or other less invasive treatment. How can my dad get referred to the Health Sciences Centre for treatment. He’s already experiencing hearing loss and who knows what neurological damage that may be irreversible. Please help. My dad is an Italian immigrant who may not be able to clearly articulate the pain. I live in Ottawa and I am unable to accompany my father to any of his appointments. From what I’ve read, Dr. Anthony Kaufman is very experienced. How can my dad get a medical appointment to see him?
I feel that this is what I have–the pain is terrible –just had CT scan done–waiting for results
You could definitely see your skills within the work you write. The world hopes for even more passionate writers like you who aren’t afraid to say how they believe. Always follow your heart.
My brother recommended I may like this blog. He was entirely right. This publish truly made my day. You cann’t believe simply how so much time I had spent for this info! Thank you!
Pingback: Chronic Facial Pain Needs Help | Pain Medical Musing
Pingback: Botox For Tmj Winnipeg | Botox Effects
I have had TN for about 25yrs,It was manageable for a number of years and then became intolerble. My family Dr. referred me to Dr. Koffman in Heahth Science Centre in Wpg. Following interviews with him I had Gamma Knife for treatment.It was successful and now after a few years It has returned and getting much stronger Very difficult and so much chronic pain now and the nerve is so angry it has caused a lesion on my cheek.
I am 85 and also have a pacemaker which I understand from my pacemaker clinic cannot have gamma knife again as an MRI guides this procedure and is out for a pacemaker. Finding carbemezapine (tegrotol) is not any where near helping.