Various desperately in pain cases have written me wondering how useful it actually is. The answer is not easy and runs like this – “It depends”. Firstly, I feel sick to find that people are being gouged $2,000 – 5,000 dollars for a simple blind paraspinous injection that anyone could give – it spreads so well from paraspinous subcutaneous injection that the relief occurs within 20 minutes. Having said that, since the wild enthusiasm of Tobinick’s initial cases, the enthusiasm of etanercept injections has not taken off in the literature as one would have thought.
The success of initial cases were not epidural steroid failures as much as the were augmented by prior epidural steroids. Even in Tobinick’s big study:
Efficacy of etanercept delivered by perispinal administration for chronic back and/or neck disc related pain: a study of clinical observations in 143 patients
Edward Tobinick and Susan Davoodifar
CURRENT MEDICAL RESEARCH AND OPINION VOL. 20, NO. 7, 2004, 1075–1085 free article here
- 69% had had 3 steroid epidurals prior.
The trasnforaminal failure study mentioned below made an important point:
- Enbrel works on Tumor Necrosis factor inhibition
- Steroid effects “are primarily due to the inhibition of enzyme phospholipase A2, with resulting reduced formation of inflammatory mediators, prostaglandins and leukotriens”
Source: redOrbit (http://s.tt/162xf).
It seems likely that both mediators need to be dealt with to get maximum effects
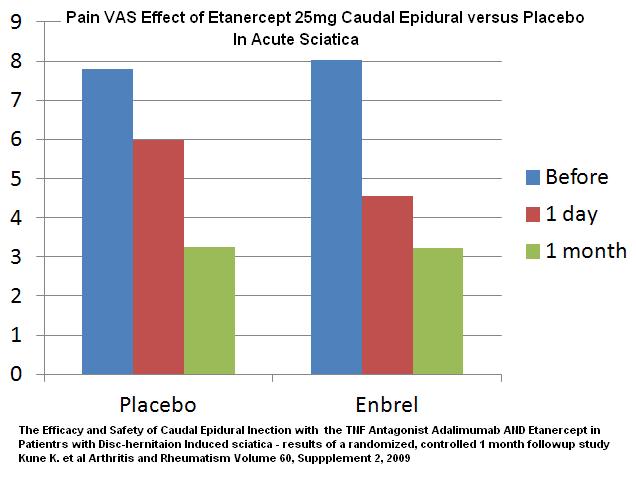
It seems clear that ONE enbrel shot does not have much lasting effect. One study gave enbrel by caudal block:
The Efficacy and Safety of Caudal Epidural Injection with the TNF Antagonist Adalimumab AND Etanercept in Patients with Disc-herniation Induced sciatica – results of a randomized, controlled 1 month followup study
Kune K. et al
Arthritis and Rheumatism Volume 60, Suppplement 2, 2009 no abstract
acute severe sciatica – this might not be fair because these will be more mechanical pressure cases then ones where the irritation is strictly chemical like most bulging disc sciaticas.
Enbrel 25 mg flouroscopically guided single cadual epidural – doesn’t say what volume it was injected in.
I could probably get better results with Caudal Intrathecal midazolam and it would be much cheaper.
Another study gave 25 mg transforaminally at L5/S1 and did not notice any benefit until steroid was injected 3 weeks later:
Anaesthesia and Intensive Care,2007 Apr;35(2):301-2
Epidural Etanercept for Lumbar Radiculopathy
Malik, K free article here
Even in the initial study it took over 2 shots on average to get the results you were after – given one week apart. One study gave 3 in 1 week The big study had average 2.3 shots.
The extent of benefits is not clear and may be suspiciously not that good. In the big study, only 55% had improvement and 27/143 = 19% had sustained drop of over 1.9/10 severity at one month – not that many
There were “golden cases”that threw away their crutches and walked – they present them in their articles.
Now we get to the “depends” -I have one patient who was having his wife administer enbrel shots – he said it would give relief but it only lasted 7-10 days. I knew something was not right so I examined him carefully and found:
- Right sided piriformis syndrome – using transverse finger stretching 10 min followed by massage I was able to remove that temporarily. – he will need work on it 2 X week for next 3-6 weeks.
- Iliac crest points – despite being a big man, tightness of the quadratus lumborum muscle must have dragged the right ribs down onto his iliac crest and gave him some exquisitely tender cluneal nerve pain spots on the iliac crest (though some could have come from Thoracolumbar – though he was not tender there). I injected these areas on crest with steroid and local and it temporarily completely removed his pains – I will see next week but suspect at least 1/2 of his pains there will be gone.
In the neck, I saw a case today with severe scalene spasm thoracic outlet syndrome with even hand colour changes. He has a radiculopathy in neck as well. He will not gain much relief until both thoracic outlet and radiculopathy are contended with. As well, he also has a very elevated left shoulder and multiple facet level tenderness which will also need attention before patient will feel any better ( I inject botox into facet joints and it helps considerably..)
Bottom line:
– better to have a steroid epidural first (I have published how shots need to be on the proper side and patient needs to lie down 20-30 min with bad side down – after the injection)
– your family doctor can cheaply give a subcutaneous paraspinous enbrel injection – don’t get fleeced
– It takes TWO enbrel shots a week apart to get any results
– I would not have enbrel shots unless someone is prepared to “turn out the lights” of other problems left behind – quadratus lumborum and piriformis spasms, iliac crest rub points, and in the neck – facets and spastic scalene/1st rib area pains with thoracic out syndrome. People are so disappointed that one treatment does not give them results – I point out that most people have 5-10 issues and they will not feel better until most , if not all are dealt with (It only takes 1-2 problems to take a pateint to “ceiling” of their pain).
Don’t forget, intrathecal midazolam shots can augment lumbar radiculopathy improvements as well.
I hoped to expand on this and lilnk to articles where I refer to other treatments..
Any comments?

I was wondering if you have any idea whether Humira would work in the same way as the Enbrel for low back pain? I have several of the Humira dose pens 40mg from when my daughter took it for Crohns disease. Also, do you know whether the Enbrel injection would help SI joint pain (my pain is to the right of the spine)
Thank you for any information you can give me.
I would think it would depend on what we are actually treating:
– Sacroiliac pain could be coming from significantly other sources – Thoracolumbar facets and muscles, quadratus lumborum, low lumbar facets, cluneal and sacral dorsal nerve roots, sacral ligaments, gluteal bursitis, piriformis syndrome, and sacroliac instability. I wrote some about that here:
Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica? – http://painmuse.org/?p=1891
A confusion with SI joint pains is the sacral ligaments and I wrote about that here:
Chronic Low Back Pain Injection Spot discussed here – http://painmuse.org/?p=1034
Actual inflammation can come from rhuematic diseases of the back and SI joints in ankylosing spondylitis, and spondylitis associated with colitis, psoriasis, and even celiac disease.
Concerning a rheumatic condition – A good indication Back is inflamed if 4/5 below perameters are positive:
– Age at onset < 40-45 years - Insidious onset > 3 months duration
– Improvement with exercise
– No improvement with rest
– Pain at night (with improvement upon getting up) – so maybe getting up at night
Other important factors:
– certain associated pains – plantar fasciitis/heel pains, frank joint arthritis (swollen hot, painful), painful swollen hands (dactylitis), rib pains
– certain associations – diarrhea (colitis), History red eye (uveitis in ankylosis spondyliltis), urinary symptoms (reiter’s)
– having psoriasis is an important association – I held off treating a chronic pain patient’s scalp problem until she saw a dermatologist who diagnosed her with psoriasis of scalp – now she will potentially be be eligible for enbrel shots for arthritis confirmed by rheumatologist
– having a family history of a rheumatic condition suggests inflammatory issues
– Having a positive response to anti-inflammatory drugs is very helpful though some do not have it.
– CRP or ESR blood tests may be elevated;
– with colitis, leukocytes in stool might be visible – our lab will no longer do them though…
– A positive Body tissue typing for HLA B27 is very helpful and cuts down the number of required findings in half. It can be more useful than MRI in the spine in diagnosis:
Clinical features of axial undifferentiated spondyloarthritis (USpA) in China: HLA-B27 is more useful for classification than MRI of the sacroiliac joint
November 2011, Vol. 40, No. 6 , Pages 439-443
Z Liao, Z Lin, M Xu, Z Hu, T Li, Q Wei, S Cao, J Huang, Y Pan, Y Wu, J Gu, abstract here: http://informahealthcare.com/doi/abs/10.3109/03009742.2011.585348
Unfortunately, where I live. testing for that is stictly regulated.
– MRI of SI joints and spine can be 80% accurate but rather useless in patients who have had cortisone injections – I have one patient, waiting to see a rheumatologist, that I would love to help by injecting her SI joints- but this would make image testing on MRI useless.
Ankylosing spondylitis is the hardest to diagnose. Features:
– age onset <35 years especially. This gets very confusing if had a back injury that never went away.
- > 3 months back pain – Sacroiliac belt line pain
– persistence from onset – usual disc disease has a waxing and waning pattern
– Radiation of pain in back to knees only
– no relief lying down; Stiffness when lying in bed
– >/= 1/2 hour morning stiffness
– relief with exercise
– Buttock pain that can alternate one to another
– Ligament “Enthesitis” spine and ribs – rib and spinal pains
– 25-40% get uveitis red eye;
– more rigid spine with restricted sidebending back
– HLA B27 antigen 90% vs 8% in normal population
– MRI sacroiliacs accurate in 80% already diagnosed but?
Whole body MRI maybe more accurate – WHOLE BODY MRI FOR ASSESSING INFLAMMATORY ARTHRITIDES: STATUS AND POTENTIAL. U. Weber Rome Eular 2010 conference poster SP0123
A recent analysis of studies has showed that physical exam is poor at making a diagnosis and history is more valuable sometimes..
Why my emphasis on SI arthritis?? – certainly in rheumatic diseases, this can be relentless and one shot very little effect – one study on anklyosing spondylitis found 40 mg adalimumab given every second week worked very well after 12 weeks of continued use:
Adalimumab significantly reduces both spinal and sacroiliac joint inflammation in patients with ankylosing spondylitis: A multicenter, randomized, double-blind, placebo-controlled study†
Robert G. W. Lambert et al
Arthritis & Rheumatism Volume 56, Issue 12, pages 4005–4014, December 2007
free pdf here: http://onlinelibrary.wiley.com/doi/10.1002/art.23044/pdf
For other Sacroiliac issues – it would depend on what the diagnosis really was…
Evidence the SI joint is actually inflamed can be determined by a variety of certain physical tests – usually if several are all positive:
Sacroiliitis Tests Not Great tests described – http://painmuse.org/?p=122
Never a simple answer… – if you try it, lets us know if it helps…
Well, I went today to one of these guys in Florida who charge $1750 for an injection of etanercept. He said I would most likely need two. So, my question(s). One, I have to run this by my oncologist since I have been treated for CLL leukemia and I understand that this could up my white counts and lower my immunity to illness…so what is your opinion on my even trying it considering the CLL? Next, can and will a regular MD inject me with the drug, and if so, what should I expect to pay? I too thought “how much can this drug cost to be so expensive per shot?” My chemo was $30K per treatment, but that was covered by insurance, this is not since it’s being used off label.
Comment – I’m sorry to see you burdened with both cancer and pain. The real answer is – I don’t know. There are some disturbing comments of etanercept used in cancer patients with constant use in CLL:
Leukemia 23, 912-918 (May 2009) | doi:10.1038/leu.2008.385
A phase I/II study of rituximab and etanercept in patients with chronic lymphocytic leukemia and small lymphocytic lymphoma
J A Woyach, T S Lin, M S Lucas, N Heerema, M E Moran, C Cheney, D M Lucas, L Wei, M A Caligiuri and J C Byrd
link – http://www.nature.com/leu/journal/v23/n5/full/leu2008385a.html
A combination of rituximab 3 times a week and enbrel twice a week is associated with “transient cytopenias and grade 3 infections in 14% of the patients”. Grade 3 are severe and undesirable [is there desirable ones?] adverse reactions.
They, however, then stated that “Infectious adverse events were also rare and generally mild, with most infections not associated with neutropenia and no grade 4 [lifethreateneing]–5 [death related] infections. None of the adverse events were treatment limiting. In addition, we did not observe any opportunistic infections with this regimen.”
Though Rituximab is generally safe, it could be part of the problem:
Int J Infect Dis. 2011 Jan;15(1):e2-16. Does rituximab increase the incidence of infectious complications? A narrative review.
Kelesidis T, Daikos G, Boumpas D, Tsiodras S.
link – http://www.ncbi.nlm.nih.gov/pubmed/21074471
In multiple Myeloma ( a blood cancer) ,etanercept, used regularly, may be associated with shortened survival:
Leukemia Research Volume 29, Issue 12, December 2005, Pages 1459–1463
Evidence of a mechanism by which etanercept increased TNF-alpha in multiple myeloma: New insights into the biology of TNF-alpha giving new treatment opportunities-the role of bupropion
R.E. Kast
http://www.sciencedirect.com/science/article/pii/S0145212605001931
“Contrary to expectations, etanercept resulted in increased levels of TNF and possibly shortened survival. ”
Both of these were with regular use… and etanercept for disc disease is often 2 shots, a week apart, every 10-12 weeks
Perhaps your oncologist can advise further…
good luck…
On June 6 of 2012 I went to Florida , to see a Dr. —–, because he had invented a treatment for back pain, with an injection of Enbrel Etarnecept Anti TNF Treatment, today is October 3 2012, i have very bad symptoms, tingling, numbness on my arms and legs dizziness , nausea, jaw pain,pain in my eyes, it Sucks !
He charge me 5000 dollars, and told me that more than 3000 patients have had the treatment, that the worse thing that could happen is that it did nt work. I regreted so much ! I spent more than 15000 in the last 3 months to find out whats happening to me, because i call the drs. Office but he dosent answer the phone or returns the calls.
I just did a blood test call Biophysical 250, which suppose to tell me if anything is wrong, i cant wait for the results, i will have them on October 16, this test its 3400 dollars, i will post the results when i get them. But we should all get toguether and put a law suit against this Dr. And the company that makes this drug which is so dangerous.
Today is November 14 2012, the Dr dosen’t answer my phone calls, i tryed to call him many times.,how unprophetional, now i have pain in my joints in my fingers, and on my knees and ankles in the mornings, and Dizziness most of the time,sore throat, and like burning or tingling sensation on my fore arms and sheens, 3 months after the shot , with the dizzieness someone told me it was high sugar, so i did the test and had prediabetes, now taking med for that, does it affect with Enbrel ?.
Today i fly to Mexico City to get into a hospital to do some tests, to find out whats happening to me since that stupid shot, any suggestions ? . .?
Sounds horrible. Hope you have better luck.
I have written a whole blog note on enbrel failures:
Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica?
http://painmuse.org/?p=1891
BTW enbrel works mostly on sciatica rather than just back pain …
-Admin
Is your blog still running? Are you still giving advise about back pain
hello!
i`ve watched a youtube video showing a woman recieved instant cure on her 2 year sciatica pain,with the perispinal etanercept
i have my MRI finding as follows
L4-L5 broad based posterior disk herniation resulting to severe spinal canal and severe bilateral nueral canal stenosis
L3-L4 posterior disk bulge resulting to mild spinal canal and mild bilateral neural canal stenosis
now im in norway,is the treatment availble here?
thanks!hoping for your quick response regarding my case
————————-
Depends how bad the spinal stenosis is:
here is a questionnaire to give you some idea:
Swiss Spinal Stenosis Score (SSS)
In the past month, how would you describe
1. The pain you have had on the average including pain in your
back and buttocks as well as pain that goes down the legs?
None
Mild
Moderate
Severe
Very severe
2. How often have you had back, buttock, or leg pain?
Less than once a week
At least once a week
Every day, for at least a few minutes
Every day, for most of the day
Every minute of the day
3. The pain in your back or buttocks?
None
Mild
Moderate
Severe
Very severe
4. The pain in your legs or feet?
None
Mild
Moderate
Severe
Very severe
5. Numbness or tingling in your legs or feet?
None
Mild
Moderate
Severe
Very severe
6. Weakness in your legs or feet?
None
Mild
Moderate
Severe
Very severe
7. Problems with your balance?
No, I’ve had no problems with balance.
Yes, sometimes I feel my balance is off, or that I am not
surefooted.
Yes, often I feel my balance is off, or that I am not surefooted.
In the past month, on a typical day
8. How far have you been able to walk?
More than 2 miles
More than 2 blocks, but less than 2 miles
More than 50 feet, but less than 2 blocks
Less than 50 feet
9. Have you taken walks outdoors or around the shops for pleasure?
Yes, comfortably
Yes, but sometimes with pain
Yes, but always with pain
No
10. Have you been shopping for groceries or other items?
Yes, comfortably
Yes, but sometimes with pain
Yes, but always with pain
No
11. Have you walked around the different rooms in your house or
apartment?
Yes, comfortably
Yes, but sometimes with pain
Yes, but always with pain
No
12. Have you walked from your bedroom to the bathroom?
Yes, comfortably
Yes, but sometimes with pain
Yes, but always with pain
No
Obviously if you have noted weakness in legs, alteration of bowel/bladder function, significant balance issues, and significant numbness in legs, then surgery would seem necessary. You need a neurosurgical opinion.
my MRI shows bulging disk my surgeon told me good candidate for surgery my health insurance denied it don’t know what do next I know physical therapy will not work numbness in leg holding me down and an epidural is just a temporary fix I need to get back to work
This is the first intelligent discussion of both piriformis and neck issues I’ve read. I’ve been battling this since 1999, with no relief. I’ve done the PT, DO and injection route. They keep injecting my trochanter and saying it’s piriformis, SI and trochanter bursitis and they all go together. The right side of my neck constantly feels like there’s a large knot in it and I have limited range of motion. In 2008 I began experiencing numbness in my feet, actually broke my foot and toe as a result. I also had surgery on my left large toe in 2008 for a bony tumor, but when the surgeon opened it crystals spilled out. He assumed it was gout and did not send it to the lab. No one knows what it was, but they all suspect it’s impacting my joints. We do know it was not gout, my uric acid levels have always been low. 4 years ago I began experiencing fevers ranging between 99.4 – 100.4 daily, just saying it makes me feel like a hypochondriac. ? It’s incredibly annoying and all they’ve found is EBV virus. The past few months I’ve been dealing with heel pain. There’s a number of other things happening and I’ve jumped through hoops with supplements etc trying to deal with it. I’m beyond fed up with Drs, no offense, as a result. I understand they’re busy, but I also feel there has to be an underlying cause and no one cares enough to find it. It’s just drug and patch and I’m not interested in drugging and patching. I want to fix it. I tried to see a neurosurgeon a few weeks ago, but I have to have MRIs to walk in the door. Do you have any suggestions? I would love to be pain free or even pain reduced and would LOVE to stop having these fevers and the ensuing fatigue and headaches. I just want to be “normal”…
Dear Christi,
widespread pains affecting neck with stiffness, SI joint needing injection, heel pains, and I suspect chronic fatigue – I wrote about a possible diagnosis for that:
The Pain Diagnosis that Cannot be Made in Women – Spine Arthritis – Ankylosing Spondylitis
http://painmuse.org/?p=77
Now becoming more real now that they found 10% of Fibromyalgia victims have active spinal arthritis:
Ablin, Jacob N., et al.
Prevalence of Axial Spondyloarthritis Among Patients With Fibromyalgia: A Magnetic Resonance Imaging Study With Application of the Assessment of SpondyloArthritis International Society Classification Criteria.
Arthritis care & research 69.5 (2017): 724-729.
http://onlinelibrary.wiley.com/doi/10.1002/acr.22967/full
The heel pain could be an Enthesitis – inflamed end of ligament seen in active arthritis.
Blood tests are often negative and MRI’s are often negative as well – there is a great variance in competence to read inflammatory changes in spine/SI joints.
Some people with this disease show response to arthritis pills/NSAID’s – if you do have a decent response to them, then that could be used as leverage.
I have a page on many of the things that could be tried in chronic pain – maybe something there could help.
Reaching “Critical Mass” to Achieving Pain Control – Procedure Pearls
http://painmuse.org/?p=3421
There is a strange combination that I have seen and recently some of my colleagues as well – ankylosing spondylitis (AnkSp) picture and a history of hypermobility. AnkSp is supposed to be a stiffening disease and so finding the opposite is amazing. I have one lady in which the inflammatory issues have settled , leaving me with the hypermobility which I am doing prolotherapy on.
If your pain is severe, there is a technique that gets a response if you have AnkSp but it require high dose cortisone pills for 2 wks:
Ann Rheum Dis. 2014 Jan;73(1):243-6. doi: 10.1136/annrheumdis-2012-203055.
Efficacy of oral prednisolone in active ankylosing spondylitis: results of a double-blind, randomised, placebo-controlled short-term trial.
Haibel H(1), Fendler C, Listing J, Callhoff J, Braun J, Sieper J.
http://ard.bmj.com/content/73/1/243
randomized double blind trial
25 patients split between 20 mg prednisolone/day and 50 mg/day
“Oral prednisolone 50 mg per day, but not low dose prednisolone, showed a short-term response that was significantly higher than placebo.”
I have vainly tried lower doses of prednisone (dose equivalent to prednisolone) before without realizing it was inadequate. Recently used 50 mg tab one/day for 2 weeks with grateful remission symptoms.
Does anyone have any other ideas?
Do you Know any doctor in California who can inject Enberl for my backpain,I had one in 2009 by Dr. Tobonik which gave me immediate relive .