At the IASP congress in Montreal, it was stated metanalysis show epidural steroid block do not work. I mentioned the fact putting the bad side down can near double its effectiveness:
Steroid Epidurals – Why Some Work And Some Not So Well
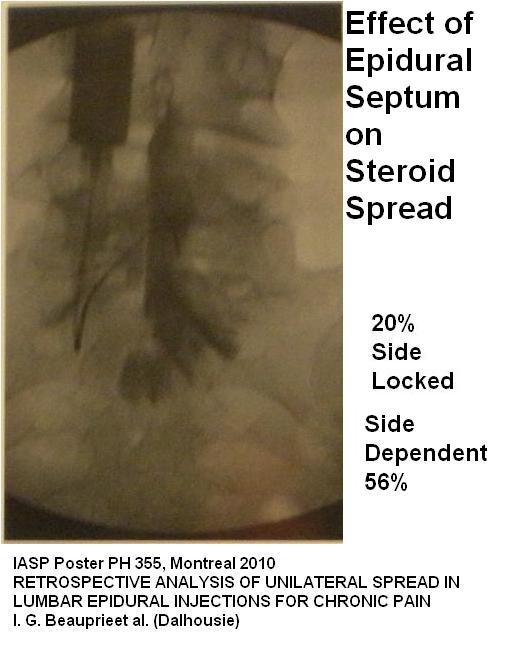
Now it appears there is a midline septum and the injected contents tends to stay on the side the needle is closer to. This has been confirmed with a recent article at end.
IASP Poster PH 355, Montreal 2010
RETROSPECTIVE ANALYSIS OF UNILATERAL SPREAD IN LUMBAR EPIDURAL INJECTIONS FOR CHRONIC PAIN
I. G. Beauprie1, A. Milne1, W. J. Maloney2, R. Hernandez1, 1Anesthesia, Dalhousie Univ., Halifax, NS, Canada, 2Diagnostic Imaging, Dalhousie Univ., Halifax, NS, Canada
- 93 lumbar epidural hilighted with dye during injection
- Midline septum seen on dye study during injection
- Unilateral or side dominant spread of injectate correlated with the side needle tip was closer to in 76% of cases
- In 20% the septum was impermeable and dye could not get to the other side.
- 5 mls would get a spread 3 levels and 10 mls 4 levels
Comment – So now not only do you have to put the patient bad side down and keep them there 15 min +, you have to aim your needle to that side as well – good luck with that… Wonder if the same happens with caudal blocks…
Might be able to get needle on right side of septum by paramedian approach were you are off to side and angle it in (particularly if you angled so hit lamina on other side and then walk it in):
I have included a further abstract form dalhousie as it is not well published:
RETROSPECTIVE ANALYSIS OF UNILATERAL SPREAD IN LUMBAR EPIDURAL
INJECTIONS FOR CHRONIC PAIN.
Hernandez R, MD1, AD Milne, MD, MSc1, Maloney WJ, MD2, Beauprie IG, MD1
1. Department of Anesthesia 2. Diagnostic Imaging, Dalhousie University
Introduction: The burden of chronic low back and sciatic pain in society is enormous in terms of both, patient suffering and cost. Interlaminar epidural steroids/local anesthetic injection is a common technique with limited evidence for efficacy outside of acute radicular pain. The ability of blind interlaminar injections to deliver medication to the putative pain generator is unclear, as is the ideal level of injection and volume of injectate. Our current practice is to routinely perform these blocks in the prone position under fluoroscopic visualization with contrast agent added to the steroid/local mixture. Several studies previously addressed the spread of contrast in lumbar epidural blocks1-3. However, none of these studies examined the effects of previous back surgery, needle tip position relative to midline or different volumes of injection on the spread in the epidural space.
Methods: We calculated the frequency of radiologically apparent septation seen on fluoroscopic images recorded from 93 lumbar epidurals which were performed on 73 consecutive patients. Images were reviewed by a panel of observers including; a senior anesthesia resident, a staff radiologist and 2 staff anesthesiologists. Flow of contrast was deemed as unilateral, side dominant or bilateral after both 5 ml and 10 ml of injectate. We also recorded final needle tip placement (left/midline/right) from the images. Demographic data including prior back surgery was extracted from the patient charts.
Results: The prevalence of a radiologically apparent septum was evident in 68/93 (73%) and 78/93 (84%) of images after 5 and 10 ml of injectate respectively. Unilateral or side dominant spread of injectate correlated with the initial side of needle placement in 76% of the images after 5 ml and 67% of the images after 10 ml of injectate.
Discussion: This study demonstrates a high prevalence of radiologically visible septation in the lumbar epidural space. Unilateral or preferential one sided flow of injection was also common. Epidural injections under fluoroscopic guidance can be an invaluable aid in pain management for documenting the presence of septation and spread of medication to the targeted region for assessing therapeutic effect. If the flow is clearly seen to the affected area without any clinical response then the clinician can consider to other pain management strategies. Thus making patient care more efficient and avoiding discomfort from non-productive procedure that at the same time is not exempt from complications.
References:
1. Renfre W. DL, et al, Correct placement of epidural steroid injections fluoroscopy guidance. AJNR AM J., Neuroradiology 1991;12:1003-1007.
2. E.L. Whitlock, et al. Influence of needle tip position on injectate spread in 406 interlaminar lumbar epidural steroid injection. Radiology 3, 2007 pp 804-811.
3. Fluoroscopy Analysis of Lumbar Epidural Contrast Spread after lumbar interlaminar injection. Lawrence Weil MD and et al. Archives at Physical Medicine and Rehabilitation. Volume 89, Issue 3 March 2008 pages 413-416.
Addendum – in 2016 article published and call this septum “Plica Mediana Dorsalis (PMD)”
Anesthesiology. 2016 Jan 20. [Epub ahead of print]
Plica Mediana Dorsalis: Unilateral Epidural Anesthesia and the Use of Bilateral Double Epidural Catheter Technique.
Ginosar Y(1), Davidson EM
http://www.ncbi.nlm.nih.gov/pubmed/26797154
- They state that “though computed tomography and necroscopy have demonstrated some degree of PMD in almost all patients,2 this is rarely a completely intact membrane.
2 Savolaine ER, Pandya JB, Greenblatt SH, Conover SR: Anatomy of the human lumbar epidural space: New insights using CT-epidurography. Anesthisiology 1988; 68:217–20 - They present a case where they had to put in two epidural catheters to achieve pain control – one on either side of septum.
This was confirmed by another study:
A Computed Tomography-Guided Demonstration of the Unilateral Distribution of Low-Volume Epidural Injectate
Semih Gungor et al
Pain Practice 2017 in press
- called it the Dorsa-median dural fold (plica mediana dorsalis)
- , , , , . Fluoroscopic analysis of lumbar epidural contrast spread after lumbar interlaminar injection. Arch Phys Med Rehabil. 2008;89:413–416.
“showed under fluoroscopic guidance that if the needle tip was lateral to the width of the spinous process in lower lumbar epidural space, the spread of injectate was unilateral 75% of the time.”
- their case with bilateral sciatica required two catheters to get bilateral epidurals


Pingback: Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica? | Pain Medical Musing