Trochanteric side of hip pain is common yet rarely properly diagnosed. Actual Gluteal tears can be a cause and by age 60, 10% of people have them. Twenty Percent of chronic back pains (average age of 54 yrs) have trochanteric pain. Proper treatment depends on extent of tears yet they have eluded recognition up until now.
Lequesne M.
From “periarthritis” to hip “rotator cuff” tears. Trochanteric tendinobursitis. Joint Bone Spine. 2006 Jul;73(4):344-8. editorial
Symptoms:
- It is more common in women and can occur as young as 37 years old. Mean ages are in 50’s or 60’s depending on study.
- Lateral hip/buttock pain perhaps radiating to thigh
- It usually develops gradually and hence diagnosis is delayed.
- Stair and uphill climbing is painful as is getting up from a chair.
- It hurts during the hip extension phase of walking.
- In elderly this could precipitate falls.
- NSAID’s, phsiotherapy and steroid injection often give a temporary benefit but may only last weeks if tears are present.
- It could take 41 months to diagnosis though doctor familiarity and use of ultrasound can cut that to 6 months
Signs:
- Trochanteric area tenderness
- Pain on external rotation with hip flexed 90 degrees
- Pain with standing on affected leg after 10- 30 sec. “virtually always present”
- Trendelenburg gait is seen in ½ -3/4 of cases and is thought an important finding.
- Pain on resisted abduction seen in 50-70% cases
- abductor weakness
- Calcifications near trochanter can be seen on Xray in 15-40% cases.
A survey of French Orthopedic surgeons found this condition was undiagnosed except if incidentally found at time of hip surgery.
It was suggested Trochanteric pain lasting or recurring over a 3 month period should have an US. Bursitis is rarely isolated finding and is usually associated with tendonitis. In persistent cases would suggest there are unrecognized tears. Partial anterior gluteus medius and gluteus minimus tears are the typical pattern.
Diagnosis can be confirmed by Positive guided injection test – injected by radiologist under imaging.
Treatments include conservative –
- NSAID’s
- physio
- weight bearing reduction
- Steroid injection can be successful if tears not evident:
abstract here
“Peritrochanteric infiltration with glucocorticoids mixed with 2% lidocaine relieves patients from their symptoms for a long period of time. Recurrence should always be expected, but treatment may be repeated.” - Surgical repair works in 6/7 tear cases in selected patients.
If hip OA is seen on xray the chances of recovery are cut 4.8 times: abstract here
Comment – Gluteal/trochanteric pains are common in chronic pain sufferers. If tenderness is just isolated to the top of the trochanter, I would think trochanteric bursitis may be more isolated. Injecting one spot will hit the bursa only ½ of the time: abstract here
I circle the tender area and inject 10- 20 mls 0.5% lidocaine with 40 mg Kenalog into multiple spots until no tender areas persist.
Trochanteric pain with pains posterior or cranially is much more complex. Lack of early availability of Ultrasound and uncertainty of findings makes it even harder for me. I find patients with trochanteric pain almost always have back pain. Maybe it is natural to hike up the hip with lateral Quadratus lumborum back muscles to compensate for the trendenburg. Yet others may have pain coming from the back.
Addendum:
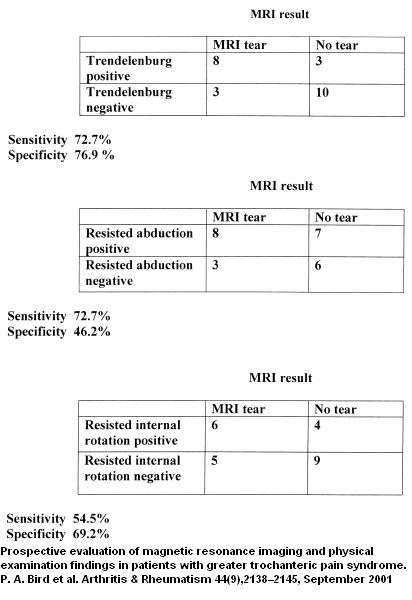
Physical findings in Gluteal tears:
Lack of trendenberg makes it safer to assume bursitis and inject with steroid ..
I would be interested in other people’s management of these cases. I would also be interested on how often this happens post MVA as some patients can even develop pelvic fractures from such.

This has been extremely helpful.
Pingback: Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica? | Pain Medical Musing
Age 47 . I have just been looking about possible causes of pain that I am having in my lower back / hip and extending in cases to my foot. Sciatica was my first thought, but although having been a long time sufferer of LBP this is somewhat different: After hurting my lower back a couple of weeks ago, it eased over several days, but now I have symptom, hitherto not experienced by myself. When I go to bed, I generally fall asleep OK, but in about 2 hours or so, I am jolted out of my sleep when I attempt to roll over, by a searing cramping pain running from the buttock to as far as the foot. It is almost unbearable to straighten the leg and get out of bed (burning cramp like feeling) at one point it felt like my femur was going to break, so bad was the pain. Then when out of bed, it is a struggle to get upright and try to walk. I fear that I might actually fall due to what feels like an unrealiability of the leg as I extend it to walk. Usually after about 5 – 10 minutes of limping / sitting down/ standing and then trying to walk a bit, it eases somewhat, but continues to be mildly sore. Thereafter, I am given to sitting up for the rest of the night. By morning I am almost totally mobile again, and this continues for the rest of the day, before the cycle begins again that night. The biggest problem for me is the feeling of something almost tearing when I attempt to turn over in bed resulting in the pain and sleeplessness. I am wonering if this sounds at all symptomatic of a hip rotator cuff tear, or am I just getting a severe sciatic attack? ( BTW, I have had sciatica many times in the past, but although similar, nothing compares to the severity of this).
I have had 3 back surgeries, the last in 2007. I have since the beginning been complaining of hip and outside of thigh pain. Over the last year it continues to get worse. Walking, sitting, standing, bending all cause the burning to become unbearable. I am in constant pain throughout the day, sleeping is next to impossible. My pain doctors just say you should exercise more. I just saw my back surgeon with a MRI from June he wanted hip MRI, yes I have abductor tears on both sides. I have been researching this and I fit every category there is. I am angry that I feel I just get blown off to just exercise more.
———————
Rosann:
You are describing rather severe neuropathic pain (burning esp). I would be looking for other sources of pain besides abductor tears. With 3 back operations I would suspect the back is involved and hence some may respond to lumbar epidural injections given by a pain specialist.
Another suspicion would be that you will have pain on the top of your iliac crest bones laterally in what is known as cluneal entrapment – sometimes as the result of ribs rubbing there. Injections there could confirm and treat that.
Somtimes, the problems are at the Thoracolumbar junction (TL) (level where ribs end – that level will refer to buttocks) – called Maigne’s thoracolumbar syndrome. I have a device called an activator and when I manipulate the Thoracolumbar levels with it, people are amazed that I am sometimes then able to massage out residual soreness left post-manipulation in the buttock, implicating the TL junction as the cause of the pains.
The piriformis can pinch the sciatic nerve and cause gluteal pains – a pelvic exam should show tenderness in the Greater sciatic notch.
These and other potential causes (including Quadratus lumborum flank back spasms which refer to hip) I discussed in:
“Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica?”
at
http://painmuse.org/?p=1891
Today. I saw a young lady with severe hip pains. She had 2 negative MRI’s – both of them worthless because there were no hip injected dye enhancement done with the procedures (though I had one patient have a hip dye injected MRI and still miss her labral tear = Plastic like rim of hip joint). The hip muscles tug on the joint and pull it out some (as per Diane Lee in her books) – I needled the muscles in the buttock around her hip (8 spots) and electrically stimulated it for 25 minutes. Afterwards I massaged the muscles painfree and could hear a loud clunk when the hip resumed its normal position. I hope that will give her some relief for a while – she will need labral tear surgery though.
Another lady today had a bad piriformis. While she was lying on her tummy, I had her drop the leg down over edge of bed 90 degrees and had her rest her knee on a stool by bed while it is down. This relaxed the piriformis in a technique called functional release (putting muscle in shortest position will make it forget it was supposed to be angry). The leg had to be tweaked so that knee was pushed into bedside some and once the sweet spot was found, I held it there 90 seconds. It can give momentary relief for 1-8 hours – good to do when going to bed and needing relief. There are positions to functionally release the gluteal muscles as well – finding someone who knows how to do this might help you find ways to turn off the pains for a short while.
Most often, the people I see will have at least 3 of above problems combined.
Finally, people with severe pain always make me nervous that something serious is being missed -I have done a few Bone Scans to Rule out any cancer deposits in those cases.
Good luck!