Over the past couple years there is growing evidence that maybe 1/3 of Fibromyalgia patients with IBS actually suffer from non-celiac gluten sensitivity and respond to gluten free diet – some within a few month, and some “gradually… over many months”. Gluten free diet could be life changing with remission of symptoms and back to work.
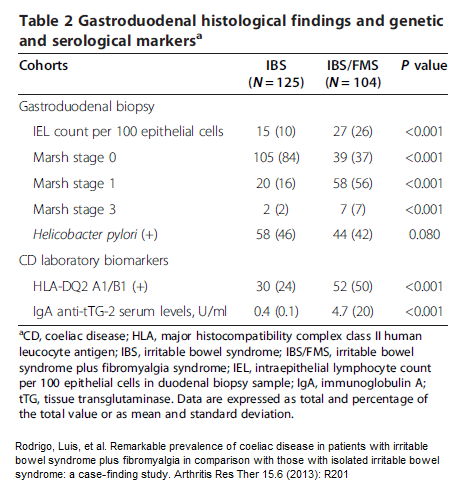
First of all, 6.7% of FM cases were found to have frank Celiac disease:
Rodrigo, Luis, et al.
Remarkable prevalence of coeliac disease in patients with irritable bowel syndrome plus fibromyalgia in comparison with those with isolated irritable bowel syndrome: a case-finding study.
Arthritis Res Ther 15.6 (2013): R201.
http://www.biomedcentral.com/content/pdf/ar4391.pdf
Also, Intraepithelial Lymphocyte counts (villi immune cellularity) is over twice as likely in FM plus irritable bowel vs irritable bowel alone
 Some of those with FM plus Irritable bowel respond gradually to gluten elimination:
Some of those with FM plus Irritable bowel respond gradually to gluten elimination:
Isasi, C., Colmenero, I., Casco, F., Tejerina, E., Fernandez, N., Serrano-Vela, J. I., … & Villa, L. F.
Fibromyalgia and non-celiac gluten sensitivity: a description with remission of fibromyalgia.
Rheumatology international, 34(11), 1607-1612; .2014
http://link.springer.com/article/10.1007/S00296-014-2990-6/fulltext.html
- Though this study zeros in on 20 responder cases, they state they are following 246 FM cases – “Clinical response has been observed in 90 of them “[off gluten]
- typical FM average duration 11.9 years.
- response either in few or many months so lack of control group makes this difficult to interpret.
- 17/20 gastrointestinal disorders with irritable bowel, esophageal reflux, constipation, dyspepsia, hiatus hernia, lactose intolerance, nonspecific colitis(likely with diarrhea)
- 8/20 depression. 8/20 migraine. 3 hypothyroid; 5 undifferentiated spondyloarthritis; 1 psoriasis
- 11/13 tested had DQ2 or DQ8 though 7 only one allele. Most celiac have this allele.
- 15/20 complete remission with back to work
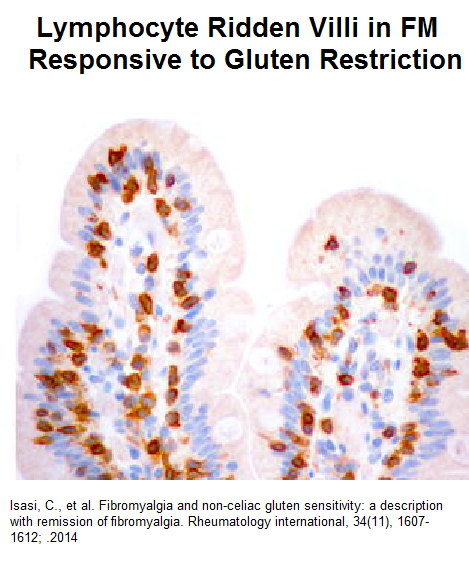
- Staining duodenal villi did not show atrophy seen in celiac but showed lymphocyte deposits
- Some were on a lactose free diet and vitamins including vitamin D
- 7/20 noted relapse on gluten
- Did mention that 1/2 of known celiac patients lack prominent gastrointestinal symptoms so easily missed
Since this study, Further elucidations have been been written up by same group:
García-Leiva, Juan Miguel, et al.
Celiac symptoms in patients with fibromyalgia: a cross-sectional study.
Rheumatology international (2014): 1-7.
http://link.springer.com/article/10.1007/s00296-014-3110-3
50-70% of FM cases have gastrointestinal problems:
- alternating constipation-diarrhea 63%
- abdominal; distension 59Z%
- dyspepsia 50%
- nausea 21%
- constipation 12%
- diarrhea 9%
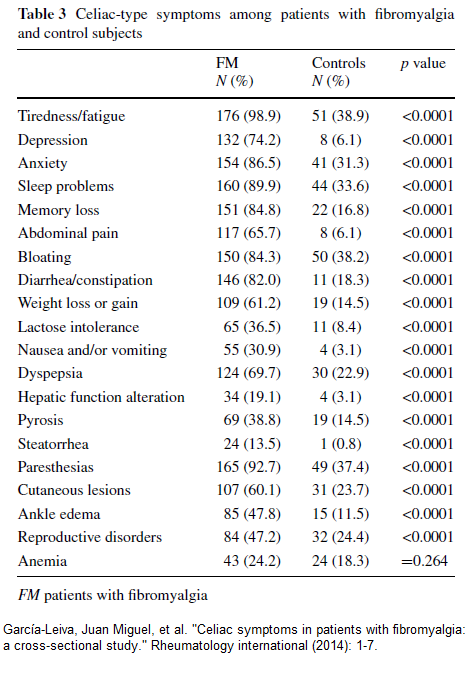
Does have a fascinating analysis of FM symptoms more than controls:
The high frequency of cutaneous lesion is interesting given that 70% of chronic urticaria have fibromyalgia and the association of celiac with dermatitis herpetiformis/chronic itch and aphthous ulcers. The ankle edema is interesting in its association with sleep apnea and the recent finding a diuretic, spironolactone, helps FM. The paresthesias is interesting in its potential association with small fiber neuropathy found in perhaps 40% FM cases. The high rates of reproductive issues could in part be related to association with Polycystic Ovaries(PCO) and how endometriosis can trigger central sensitization. Low ferrritin is strongly associated with FM and a common cause of that is malabsorption which Celiac ca do; anemia is much more common in celiac. Memory loss, depression, and fatigue are also more common in FM than celiac.
A comparison with gluten sensitivity cases gives this picture:
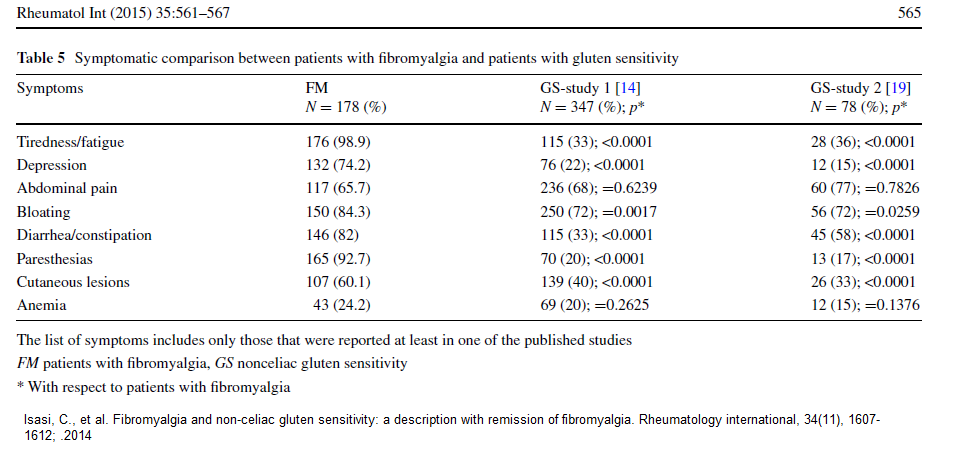 It would seem the features more related to gluten intolerance would be less fatigue, less depression, less diarrhea/constipation, less paresthesias, and less sick lesions.
It would seem the features more related to gluten intolerance would be less fatigue, less depression, less diarrhea/constipation, less paresthesias, and less sick lesions.
- given multiple sensitivities seen in FM, gluten sensitivity would be a natural progression
Comment -The problem is the lack of serological tests and the fact duodenal biopsies are not done on these cases. I have one lady with increased cellularity observed on Villi biopsy totally ignored by her gastroenterologist that concluded she was hysterical – so biopsy results may just be ignored. I have over the years been surprised by how many FM subjects had noted that wheat bothered them. I have had mixed results about gluten elimination but often that period of elimination would not have been long enough to have helped the FM much. It looks like subjects with FM AND Irritable Bowel might want to eliminate gluten for an extended period, particularly if they note wheat bothers them some. This picture is changing rapidly:
Slim, Mahmoud, Elena Pita Calandre, and Fernando Rico-Villademoros.
An insight into the gastrointestinal component of fibromyalgia: clinical manifestations and potential underlying mechanisms.
Rheumatology international (2014): 1-12.
http://link.springer.com/article/10.1007/s00296-014-3109-9
Vitamin B6, B12, and E can be deficient in celiac and it would be prudent to take
- B6 100 mg/day (no more as 400/day can cause neuropathy)
- B12 1000-2000 u/day
- vitamin e 100 u/day (no more as higher implicated in strokes)
Cases of Vitamin E deficiency have occurred in Celiac and are associated with Neuromuscular problems:Kleopa, Kleopas A., et al.
Reversible inflammatory and vacuolar myopathy with vitamin E deficiency in celiac disease.
Muscle & nerve 31.2 (2005): 260-265.
- Celiac can be associated with polyneuropathy and leg edema:
World J Gastroenterol. 2007 May 14; 13(18): 2636–2638.
doi: 10.3748/wjg.v13.i18.2636
Celiac disease manifested by polyneuropathy and swollen ankles
Zlatko Djuric, Borislav Kamenov, and Vuka Katic
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4146831/
- 2/3 of established celiac cases will have sacroiliitis for which I would steroid inject their SI joints..
Rheumatol Int. 2010 Feb;30(4):455-60.
Back pain and sacroiliitis in long-standing adult celiac disease: a cross-sectional and follow-up study.
Vereckei E, Mester A, Hodinka L, Temesvári P, Kiss E, Poór
http://www.ncbi.nlm.nih.gov/pubmed/19504097
- rarely polyarthrtis can be the only symptom of celiac:
Journal of Clinical Rheumatology: June 2010; 16(4) 195-196
doi: 10.1097/RHU.0b013e3181dfcffd
Silent Celiac Disease Presenting With Polyarthritis
Efe, Cumali MD*; Urün, Yuksel MD*; Purnak, Tugrul MD†; Ozaslan, Ersan MD†; Ozbalkan, Zeynep MD‡; Savaşs, Berna MD§
http://journals.lww.com/jclinrheum/Citation/2010/06000/Silent_Celiac_Disease_Presenting_With.15.aspx
Addendum – the very next day I had an old Fibromyalgia pain patient come in for a physical. I had not seen her for some time so needed to get out the old paper chart (electronic 5 years). She had multiple chemical sensitivities and an irritable bowel but tested negative for celiac though wheat did bother her some. She has been off wheat for some years and her pains gradually disappeared except for some neck-shoulder mechanical issues. This is why she has not needed to come in..
Another patient that morning, again a widespread pain with irritable bowel, has chronic nausea/vomiting and has been worked up by a gastroenterologist and was negative for celiac. Her pains do not respond to any treatment. She has however, been off wheat for 2 weeks (boyfriend a chef had helped do this). Her nausea is better and I wonder if we wait some months whether her pains will improve as well…
I am certainly a believer that there is something to this wheat issue. I had failed to procure major results with pain before because most would give up gluten free diet after a couple weeks. – If it takes months + to get better that could be an issue.

Pingback: Reaching “Critical Mass” to Achieving Pain Control – Procedure Pearls | Pain Medical Musing
Pingback: Recurrent Abdominal Pain (RAP) in Children – More Than it Seems | Pain Medical Musing
Pingback: A Multisystem Disease Problem Case | Pain Medical Musing