I am trying to put together a list of steps for prescribing Marijuana. This is version 1.1 – please provide additional steps. Our province dos not cover this drug even for palliative care patients (yes, we are in a bible belt…). However, the military will cover cases for PTSD. Please add advice/comments. I am using Cannimed – a local supplier as an example but could sure use something cheaper… Step are included below:
First of all, Canadian guidelines:
https://www.camh.ca/en/research/news_and_publications/reports_and_books/Documents/LRCUG.KT.Professional.15June2017.pdf
I have relied heavily on :
Wilsey, Barth, et al.
The Medicinal Cannabis Treatment Agreement: Providing Information to Chronic Pain Patients via a Written Document.
Cell 916 (2014): 402-2270.
http://journals.lww.com/clinicalpain/Abstract/2015/12000/The_Medicinal_Cannabis_Treatment_Agreement_.10.aspx
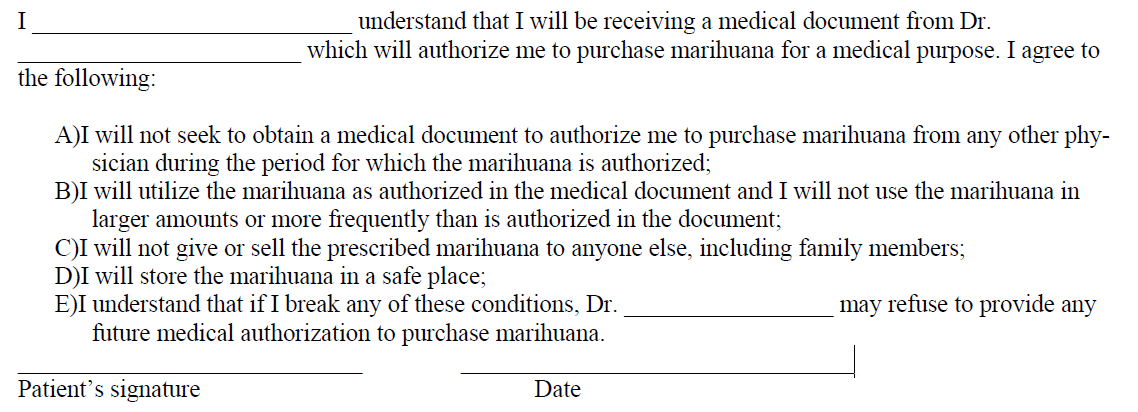
I have enclosed the agreement necessary by my college and that one worked out by above as adapted by B. Fischer:
Fischer B, Jeffries V, Hall W, et al..
Lower Risk Cannabis use Guidelines for Canada (LRCUG): a narrative review of evidence and recommendations.
Can J Public Health. 2011;102:324–327
http://journal.cpha.ca/index.php/cjph/article/viewFile/2758/2485
Enclosed is a printable agreement here in word format: (works better if you right click it and tell it to open in new tab)
cann_agree
Some steps:
1)Document reason for use and keep a separate record of use in chart long with indication. Usually this involves the failure of a specialist to help. It is assumed that they have failed medical treatment including opioids though that is a bad standard given opioids can kill and Marijuana does not. Had a recent referral that had saphenous neuropathy from leg injuries. I was interested in using nerve blocks, tender skin nerve perineural D5W injections, TENS, along with standard treatments but she was not interested so failed to qualify. ( I wonder if in a needle phobic this could be bypassed)
2) Assess addiction risk – opioid risk tool ORT though I got to admit I will ask more questions re possible ADHD and bipolar disease.
Simple Opioid Risk Tool http://painmuse.org/?p=35
Bipolar is common and occurs in 20% of Fibromyalgia cases for example:
Kudlow, P. A., et al.
Prevalence of fibromyalgia and co-morbid bipolar disorder: A systematic review and meta-analysis.
Journal of affective disorders 188 (2015): 134-142.
http://www.researchgate.net/profile/Paul_Kudlow/publication/281712395_Prevalence_of_fibromyalgia_and_co-morbid_bipolar_disorder_A_systematic_review_and_meta-analysis/links/56022f1f08aeb30ba7355af7.pdf
My daughter and I poster presented how bipolar is missed to the Canadian Pain Society:
- In the bipolar subgroup, many can remember never being happy rather than having periods of hypomania.
- a family history of bipolar or a very angry dysfunctional parent helps.
- People with chronic pain, lack of sleep, and poverty may not get a happy manic phase or go on sprees – just too tired and poor.
- They will however, perhaps remember a turbulent youth where they may have left home early, gone through a dark phase with drugs, teen pregnancy, and failed school.
- They may also notice that antidepressants alone either fail or put then into an agitated state.
- Typically they are much more likely to has spells of a mixed state – more agitated, can’t sleep, can’t think, and angry. These can be horrible and can worse than their pain.It can last up to months + and spring is a common time.
- Asking them to explain how in their youth they went from being happy to very sad in one day or visa versa (rapid cycling in adolescence) might help get their attention.
- Some have never had a good sleep. Family history, suicide ideation or attempts, and prior hospital admissions clinches the diagnosis. ADHD features are common.
3) Go over risks – I use government Canada risk and print it out
http://www.hc-sc.gc.ca/dhp-mps/marihuana/info/cons-eng.php
especially
“Health Canada has stated that Professional Standards and Guidelines – Marijuana for Medical Purposes May 5, 2015 (revised July 30, 2015) driving, operating heavy equipment, or other activities involving alertness and coordination may be unsafe for up to 24 hours following a single consumption, depending on the dosage, the delivery route, and the patient’s age and other health factors. It is important to discuss with patients that their reactions to the substance and to different formulations are individual, and that it is important to go slowly with the treatment until a stable, effective dose is reached. A similar caution should be provided to any patient in a safety-sensitive occupation such as health professionals and the supervision of children.”
https://www.cpsbc.ca/files/pdf/PSG-Marijuana-for-Medical-Purposes.pdf
A recent article quoted the addiction rate at 9%
he Medicinal Cannabis Treatment Agreement Providing Information to Chronic Pain Patients Through
a Written Document
Barth Wilsey, et al.
Clin J Pain 2015;31:1087–1096
4) Recent article
Wilsey, Barth, et al.
The Medicinal Cannabis Treatment Agreement: Providing Information to Chronic Pain Patients via a Written Document.
Cell 916 (2014): 402-2270.
http://journals.lww.com/clinicalpain/Abstract/2015/12000/The_Medicinal_Cannabis_Treatment_Agreement_.10.aspx
set exclusions for:
- pregnant or child bearing age
- middle age or older with know heart or heart rhythm disease -“In middle-aged users, the cardiovascular risk of cannabis is less benign. In a case-crossover study, the risk of myocardial infarction was 4.8 times higher in the hour after cannabis use than at baseline. Furthermore, middle-aged users increase their annual absolute risk of a cardiovascular event by 1.5% to 3%.”
- Serious mental illness – schizophrenia, delusions, hallucinations, mania hx
5)Fill out agreement (taken from Sask College of P&S)
6) document in chart
- diagnosis
- reason for cannabis
- that risks discussed
- cannabis provider
- opinion whether this is therapeutic or palliative
7) keep a separate record
The physician must retain a single record, separate from other patient records, which can be inspected by the College, and which contains:
A) The patient’s name, health services number and date of birth;
B) The quantity and duration for which marijuana was prescribed;
C) The medical condition for which marijuana was prescribed;
D) The name of the licensed producer from which the marijuana will be obtained, if known to the physician
I’m not sure what online physicians are supposed to do…
8. Physicians who prescribe marijuana will be required to provide the College with the information referenced in # 6:
A) Every twelve months if the physician has prescribed marijuana to fewer than 20 patients in the preceding 12 months;
B) Every six months if the physician has prescribed marijuana to 20 or more patients in the preceding 12 months.
7) The Canadian Medical Protective Association has a”Release form for medical practictioners”
8) Patient needs to fill in a form for producer and form might depend if has stable address and whether drug is coming to medical office.
Cannimed in Saskatoon forms:
http://cannimed.ca/pages/applying-for-medical-marijuana
more generic sample form:
http://www.hc-sc.gc.ca/dhp-mps/alt_formats/pdf/marihuana/info/med-eng.pdf
9) Doctor needs to fill in form for what mix and how many grams a day (1 up to 3 gm/day seems standard but would be less in elderly). Often one is unsure re what mix and might be best to let them sample several types. Cannimed has a Starter pack which includes CanniMed® 17·1, 9·9, 4·10 mixes. Proved handy with my last case as the mix with high THC proved too psychologically altering. If you put repeats for a year they will get such.
10) Probably start with air vaporizer -Cannimed has their “Arizer”
http://cannimed.ca/products/arizer-air-vaporizer
– you put some in it, it heats up quickly and you inhale. Oral cookies might require 3 times the dose and given it costs $7-10 dollars/day by inhalation – the price seems too great.
There is a plastic bag device as well:
Volcano medic ( it is more expensive)http://cannimed.ca/pages/our-products
11) Fax patient and your forms and call them to make sure they got it ( had one they “lost”). They don’t need to register your fax number online as long as fax number is on forms.
12) This goes without saying drug needs to be kept in a safe place away from children.
One recent article made this their number one concern:
Wilsey, Barth, et al.
The Medicinal Cannabis Treatment Agreement: Providing Information to Chronic Pain Patients via a Written Document.
Cell 916 (2014): 402-2270.
http://journals.lww.com/clinicalpain/Abstract/2015/12000/The_Medicinal_Cannabis_Treatment_Agreement_.10.aspx
The aspect of driving does bother me and I would suggest that a Marijuana subject may not be able to drive if at all affected and certainly would not be able to drive with any alcohol co-use. W. Barth makes it clear by stating:
“I will not drive a car or operate heavy machinery for 3 to 4 hours after use of medicinal cannabis, or longer if large doses are used or the effects of impairment persist. I will use a designated driver for automobile transportation if I have to go out sooner than 3 to 4 hours after taking this medicine.”
12) Patient should be cautioned to avoid use in public places and might have trouble with urine drug testing.
They need to be aware it is not a great drug – it will drop pain 1-1.5/10 only – however I have a couple cases where living at 7-9/10, this is a big plus.
I would appreciate any additions I should put into this.

Pingback: Reaching “Critical Mass” to Achieving Pain Control – Procedure Pearls | Pain Medical Musing