Presentation at Canadian Pain Society Winnipeg 2013 found only 23.7% of severe neuropathic pain victims responded to Canadian Pain Society drug protocols for neuropathic pain. It is time to look outside the box for treatment measures.
Neuropathic Pain Sig Meeting
Canadian Pain Society
Winnipeg, Canada May 2013
later published in:
Moulin, Dwight E., et al.
Long-term outcome of the management of chronic neuropathic pain: a prospective observational study.
The Journal of Pain 16.9 (2015): 852-861.
http://www.jpain.org/article/S1526-5900%2815%2900703-8/fulltext
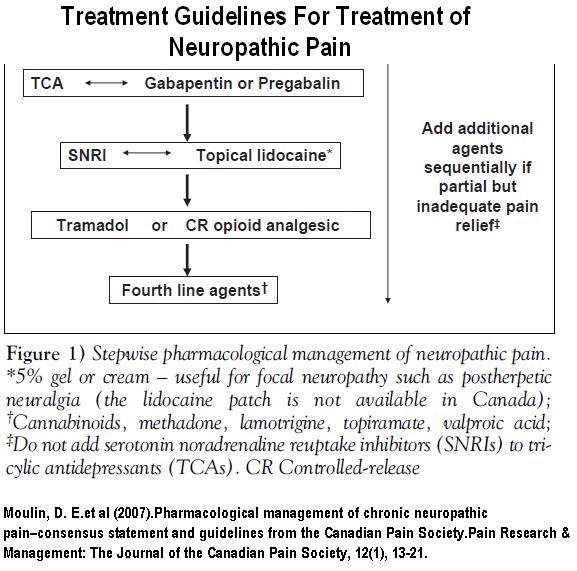
treatment was based on protocol worked out here:
Moulin, D. E., Clark, A. J., Gilron, I., Ware, M. A., Watson, C. P. N., Sessle, B. J., … & Velly, A. (2007).
Pharmacological management of chronic neuropathic pain–consensus statement and guidelines from the Canadian Pain Society.
Pain Research & Management: The Journal of the Canadian Pain Society, 12(1), 13-21.
http://www.canadianpainsociety.ca/pdf/PharmacologicalManagementChronicPain_CPS-GUIDELINES.pdf
Their protocol is pictured as such: – though later version uses marijuana early
Only 23.7% were controlled by these measures. An article in press also states this very succinctly:
[re Complex Regional Pain Syndrome (CRPS)] –
“The existing data from treatment trials conventional analgesics, anti-neuropathic pain medications or nerve blocks have been largely disappointing [3, 4]”
3. Rowbotham MC. Pharmacologic management of complex regional pain syndrome. The Clinical journal of pain 2006; 22: 425-9.
4. Cossins L, Okell RW, Cameron H, Simpson B, Poole HM, Goebel A. Treatment of complex regional pain syndrome in adults: A systematic review of randomized controlled trials published from June 2000 to February 2012. European journal of pain 2013; 17: 158-73.
“and much of the emphasis in treatment is on functional rehabilitation …. The limitations of existing treatments means that a substantial cohort of CRPS patients… is left with refractory, long-term severe pain causing significant disability.”
An example of infectiveness of oral treatments comes into light with a study on gabapentin, the jewel of neuropathic pain treatment, on neuropathic pain in 2002:
Pain. 2002 Oct;99(3):557-66.
Gabapentin in neuropathic pain syndromes: a randomised, double-blind, placebo-controlled trial.
Serpell MG; Neuropathic pain study group
http://www.ncbi.nlm.nih.gov/pubmed/12406532
Though they talk glowingly about summations of certain findings, the overall pain was not statistically better than placebo after 6 weeks (the lack of stars at bottom). I have extended the graph to the bottom and it is obvious changes are not great.
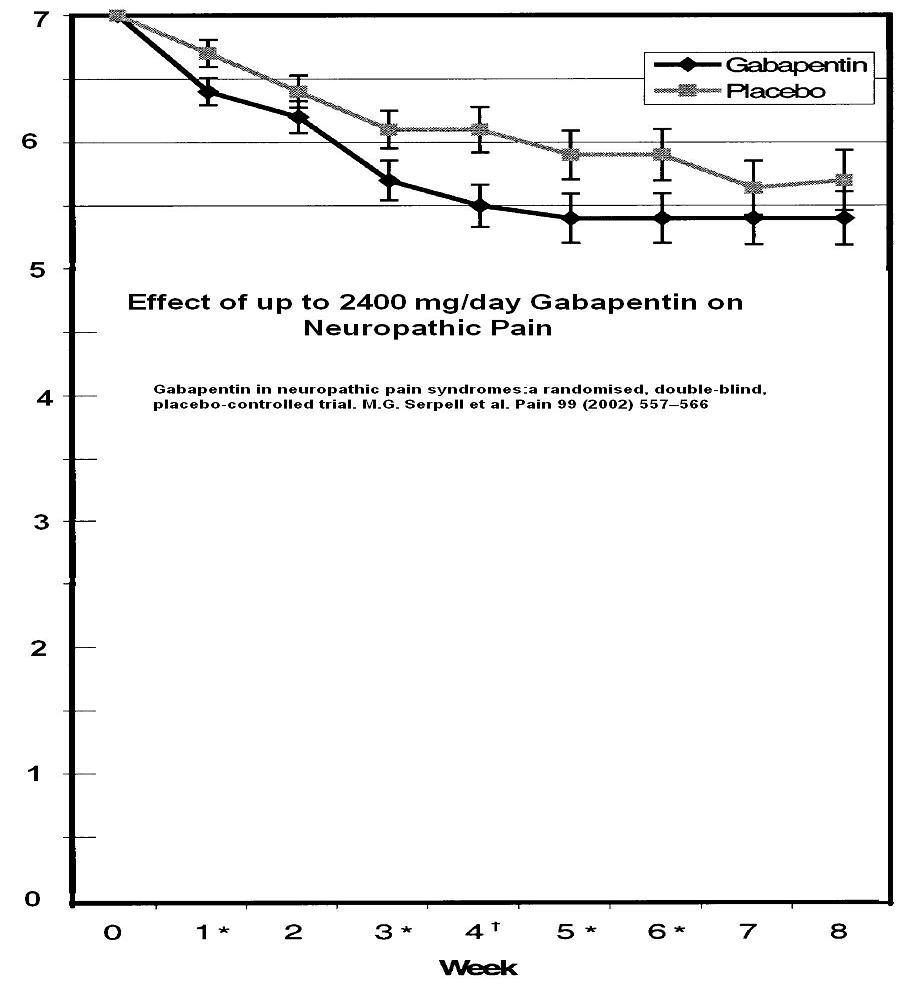
To be fair however, there was a 20% subgroup that did get over 50% improvement though I cannot say if it would last..
Also it is common to take patients to 3600 mg/day now though how many can tolerate that I do not know.
The other Jewel was pregabalin. It failed to show longterm effectiveness in a recent trial of chronic sciatica pain – what 1/2 of neuropathic pain patients suffer from.
Sciatica Pain Is Different and Does NOT Respond Much to Pregabalin (Lyrica)
http://painmuse.org/?p=341
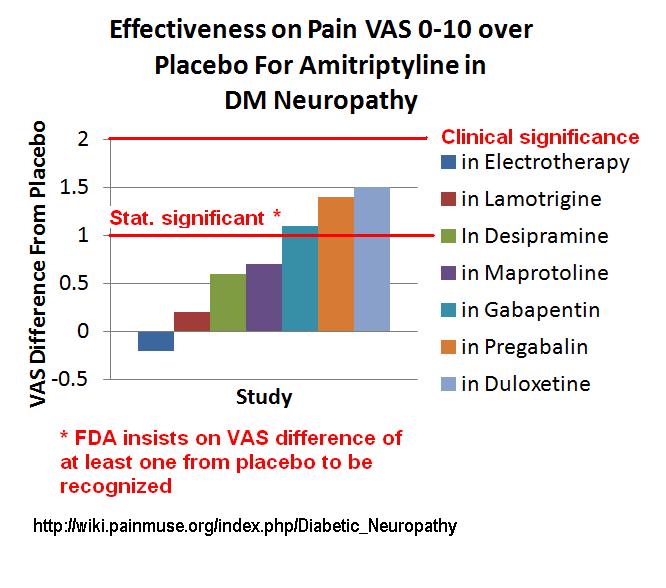
Much of the effectiveness of Tricylic antidepressants comes from a study where by frequent calls and support, subjects were worked up to 125 mg of amitriptyline for diabetic neuropathy pain. No study since has been able to get subjects past 25-75 mg and at that level, response is inadequate. I have a long-winded discussion about this here:
http://wiki.painmuse.org/index.php/Diabetic_Neuropathy
Below is the effectiveness of lower dose amitriptyline in various studies: A drop of 2 is considered CLINICALLY significant. However, I had a discussion with Dr. R. Dworkin, one of the heads of the US neuropathic pain group, about this clinically significant level and he contends if the drug is clinically safe and tolerable, then less effect is still important. – so try it and see.
Concerns raised re treatment guidelines:
- Valproic acid probably not as effective as other 4th line measures; Topical lidocaine maybe not as effective.
- (Raised by me) Neuropathic pain drugs do not work well on radiculopathy pains which constitute nearly 1/2 of chronic neuropathic pains.
- (My concerns) – fails to consider entrapments –
– tarsal tunnel syndrome considered by some an integral part of diabetic neuropathy requiring surgery – as per
Electrodiagnostically, Tarsal Tunnel Syndrome Rampant in Diabetics
Surgery For Diabetic Peripheral Neuropathy – Another Option Not Available Here
Nerve Entrapment in Diabetic (DM) Peripheral Neuropathy – Surgery Helps Foot Ulcers and Charcot Foot Syndrome
– piriformis entrapment – in chronic back and post-laminectomy pain, division of piriformis was successful in 85% of cases in relieving pain:
Mizuguchi T.
Division of the pyriformis muscle for the treatment of sciatica. Postlaminectomy syndrome and osteoarthritis of the spine.
Arch Surg 1976;111:719 –722. abstract poor HTML from google cache
Various injections and physiotherapy techniques could be used but are vigorous
Enbrel Failure – So What Else Can You Do For Chronic Back Sciatica?
– Scalene and Pectoralis minor contributions to cervical/whiplash radiculopathy – a topic in its own
- Nerve Blocks regional and epidural are considerations. I feel midazolam epidural/intrathecal could be offered when epidurals wear off between steroid injections:
http://painmuse.org/?p=2527.
Epidurals are fraught with the need for subject to lie down for 20 minutes after injection with bad side down, and the issue the shot could get on the wrong side of epidural septum. The mineralcorticoid effects of the steroid are pro-inflammatory which could blunt response. I feel the day of steroid alone shots should be over and steroid plus entanercept shots should be done -with the original successful 25 mg – not like a recent negative pathetically-dosed 4 mg study used recently. - The Canadian Pain Society also has documentation on interventional injections:
NERVE BLOCKS FOR NEUROPATHIC PAIN SUMMARY OF THE LITERATURE
http://www.canadianpainsociety.ca/pdf/nerve_blocks_final_report.pdf
At the conference, I bought up a series of options that could be potentially useful:
- Therapeutic B12 levels (around 1,200 ng/ml) – 2 weeks of B12 1000 ug/day, subcutaneously given by patient , for 14 days can bring levels up quickly to that level (not achievable for several month on oral meds). Shots are there maintained on need basis (1-7 days). As per findings here:
Chronic Back Pain Help – Forgotten B12 Injections and What Else Good For… - Ketamine shots – have found 10 mg ketamine given twice or 3 times into deltoid muscle – separated by 15 minute each – could capture significant control of pain and mood. Depersonalization side effects could be avoided by terminating shots should subject start feeling”funny”. One subject had an episode of bladder frequency on 15 mg X 3 divided by 15 minutes each, but when retried 6 months later, has never had a problem with 10 mg X 2 (a dose she had originally been on and managed well on). However, still not a drug of people with bladder issues.
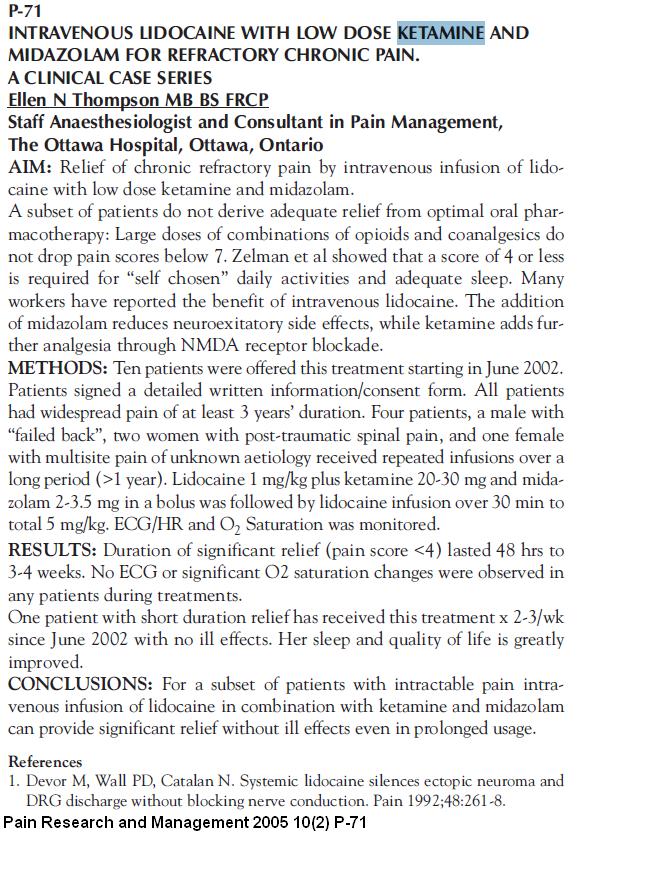
- A one shot IV version of ketamine – lidocaine is promoted by an Ottawa anesthesiologist, Dr. Ellen Thompson. It involves considerable sedation and I have not done it. I have persuaded Dr. Mike Lang of anesthesia to do it at Regina General Hospital for select patients:
- Treatments for Complex Regional Pain:
– IV biphosponates- despite a trial finding one infusion did not work, prior, and subsequent trials have found it useful in severe regional pains when given 3 times:
Pamidronate and Clodronate – hope for Reflex Sympathetic Dystrophy (aka CRPS) and Back Pain
Pamidronate Works Again – For Childhood Leg Pain – Complex Regional Pain
C0nfirmed Again – Biphosphonates Work In Complex Regional Pain–
One of the studies with Three consecutive day infusions of 1 mg/kg/day (= 80 – 90 mg for people around here…)
They found” On the 45th day after the beginning of the treatment, total disappearance of pain was obtained in 25 patients (86.2%) and functional improvement was obtained in 14 out of 20 patients (70%).”
Rheumatology (Oxford). 2001 Dec;40(12):1394-7.
Treatment of reflex sympathetic dystrophy with pamidronate: 29 cases.
Kubalek I, Fain O, Paries J, Kettaneh A, Thomas M.
http://rheumatology.oxfordjournals.org/content/40/12/1394.full.pdf
- 5 Day Infusions: – mentioned the 5 day treatments to one anesthetist – his comment – “never going to happen”. It will take legislature to make it happen because the medical community will not spare the resources.
-IV Magnsium :
New Hope For Complex Regional Pain Syndrome I – 5 days Magnesium Infusions
-IV Lidocaine
No Hope Severe Neuropathic/CRPS Pain?- 4-5 Day IV Lidocaine to Rescue
– IV ketamine:
IV Ketamine – Pain Rescue For Refractory Pain Flareups – http://painmuse.org/?p=489 -mentions how some had daily infusions for 4 days – (suspect 5 would be better).
Recent review high-lighting prolong ketamine infusion advantage:
Br J Clin Pharmacol. 2013 May 23.(in press)
Prolonged ketamine infusion as a therapy for Complex Regional Pain Syndrome:Synergism with antagonism?
Pickering AE, McCabe CS.
http://www.ncbi.nlm.nih.gov/pubmed/23701138A good update review of IV treatments for chronic pain can be reviewed free here:Pain Physician. 2013 May-Jun;16(3):231-49.
Intravenous infusions in chronic pain management.
Kosharskyy B, Almonte W, Shaparin N, Pappagallo M, Smith H.
http://www.painphysicianjournal.com/2013/may/2013;16;231-249.pdf
- Treatments for pains with paresthesias – even in Fibromyalgia, the addition of paresthesias brings up the possibility of Chronic Demyeliniating Inflammatory Neuropathy (CIDP) for which pulse steroids, immunoglobulin infusions , and plasmaphoresis could be helpful:
-Use included Dexamethasome 4 mg – 4 am, 4 lunch, 2 supper = 40 mg/day – for 4 days
Pulsed high-dose dexamethasone versus standard prednisolone treatment for chronic inflammatory demyelinating polyradiculoneuropathy (PREDICT study): a double-blind, randomised, controlled trial
Ivo N van Schaik MD a , Filip Eftimov MD a, Pieter A van Doorn MD c, Esther Brusse MD c, Leonard H van den Berg MD d, W Ludo van der Pol MD d, Catharina G Faber MD e, Joost CH van Oostrom MD f, Oscar JM Vogels MD g, Rob DM Hadden MD h, Bert U Kleine MD i, Anouk GW van Norden MD i, Jan JGM Verschuuren MD j, Marcel GW Dijkgraaf PhD b, Marinus Vermeulen MD a
The Lancet Neurology, Volume 9, Issue 3, Pages 245 – 253, March 2010
http://www.thelancet.com/journals/laneur/article/PIIS1474-4422(10)70021-1/fulltext#article_upsell– - Use IV blood plasma gamma globulin:
Caro, X. J., Winter, E. F., & Dumas, A. J. (2008).
A subset of fibromyalgia patients have findings suggestive of chronic inflammatory demyelinating polyneuropathy and appear to respond to IVIg.
Rheumatology, 47(2), 208-211.
http://rheumatology.oxfordjournals.org/content/47/2/208.full.pdf+html
“Fifteen FMS/CIDP subjects were subsequently treated with IVIg (400 mg/kg each day for 5 days). Pain (P=0.01), tenderness (P=0.001) and strength (P=0.04) improved significantly. Fatigue and stiffness trended towards improvement.” - Injecting myofascial triggers – I often use 5% lidocaine to get longer lasting results but stay clear of spine – results are often much better when combined with ketamine shots.
- Massage related techniques – some people have never had their knots taken out and are like wood to start with – takes time
- Prolotherapy – Backs that tire out standing or sitting too long make one suspect that is an issue. I have been experimenting with dilute testosterone injection which are less painful.
- Facet injections – also difficult to get done here
- Pulsed Radiofrequency to nerve root ganglion – an audit found it helped maange 1/4 low back pain sciatica cases:
Pulsed Radiofrequency Treatment Adjacent to the Lumbar Dorsal Root Ganglion for the Management of Lumbosacral Radicular Syndrome: A Clinical Audit
Koen Van Boxem et al
Pain Medicine Volume 12, Issue 9, pages 1322–1330, September 2011
http://onlinelibrary.wiley.com/doi/10.1111/j.1526-4637.2011.01202.x/abstract;jsessionid=9E84FA7C1DE69582A5D13C1DE16268EC.d01t01?deniedAccessCustomisedMessage=&userIsAuthenticated=false
Not seen at all here. - Physio techniques – Strength training has been shown to play a prominent place in chronic knee pains and is too big a topic to go into here.
- Methadone – because of its dual mode of action (NMDA block and opioid mu receptor effects), it is the king of painkillers. One of the palliative care doctors might be willing to be involved.
- Spinal and peripheral nerve stimulation – a possible 3 year wait if at all here.
A poster example :
Greene, M., & Sugar, R. (2009). Poster 273:
Resolution of Intractable Bilateral Neuropathic Lower Extremity Pain of Unclear Etiology: A Case Report.
PM&R, 1(9), S222.
– 75% reduction of undetermine pain in legs with spinal cord stimulation in this case - Botox injections – significant relief reported in piriformis syndrome and selected cases of back pains.
- acupuncture
- intradermal D5W injections – If one is careful, one can feel the nerves under the skin in painful areas as being tender – If you pucker the skin and inject above it ever cm or so with D5W superficial to nerve, the soreness will temporarily remit. Repeated injections can make it more lasting.
- HCG injections – recent investigations found this can help and reduce opioid consumption 20-100%
- IV pamidronate for chronic back pain – infusions can reduce pain but 40% or more in recent studies
- antibiotics for chronic back pains – oral clavulin or flouroquinolone for 100 days can potentially reduce pains 50% a year later
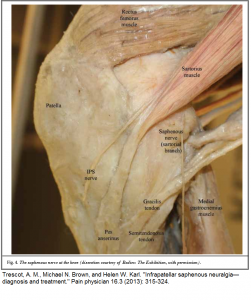
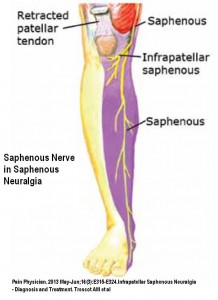
Comment – had a case late last week subsisting with pains about 8/10 – could barely touch her anywhere. Among widespread pains was shoulder buristis bilaterally limiting elevation arm to less than 90 degrees. Apparently she was blood tested and steroid tried briefly but then taken off because it stopped working. She had had ulcers when young and was not on any arthritis NSAID’s. She was so bad, I gave her 2 shots of ketamine 10 mg 15 minutes apart, then gradually worked out here piriformis on one side. She had severe pain down inner aspect right knee going into meidal shin of neuralgic intensity much like saphenous neuralgia:
I injected saphenous nerve at adductor tunnel and it gave dramatic relief of pain except a patch just above kneecap – making me think this was maybe more obturator nerve too.
 I taught her functional release (counterstrain) for psoas and piriformis on other side – you put the muscle in a short painfree position for 90 seconds, and the muscle will temporarily forget it is in pain… I ran blood work for inflammatory issues and started her on a steroid pulse (40 mg dexamethasone/day in divided doses – note don’t use this dose on a diabetic). I considered getting in touch with Dr. Carmen Johnson – one of our palliative care doctors to use methadone. By the next morning her ESR came back as 42 and the pulse steroid was already lowering her pain levels. I referred her to a rheumatologist (No temporal arteritis symptoms so will have to wait) re Polymylagia Rheumatica. She will start on 20 mg/day Prednisone after the pulse. Given that the steroid effects seem to wane after the last use, I wonder if methotrexate (not favored by out rheumatologist) or etanercept should be added. A biphosphonate will be added once sure of stomach tolerance to steroids. Will need to check blood pressures and glucose levels. I imagine I will have to deal with here knees (restricted knee flexion and probable OA knees) – and multiple triggers – especially piriformi and subscapularis. B12 shots were taught for this lady.
I taught her functional release (counterstrain) for psoas and piriformis on other side – you put the muscle in a short painfree position for 90 seconds, and the muscle will temporarily forget it is in pain… I ran blood work for inflammatory issues and started her on a steroid pulse (40 mg dexamethasone/day in divided doses – note don’t use this dose on a diabetic). I considered getting in touch with Dr. Carmen Johnson – one of our palliative care doctors to use methadone. By the next morning her ESR came back as 42 and the pulse steroid was already lowering her pain levels. I referred her to a rheumatologist (No temporal arteritis symptoms so will have to wait) re Polymylagia Rheumatica. She will start on 20 mg/day Prednisone after the pulse. Given that the steroid effects seem to wane after the last use, I wonder if methotrexate (not favored by out rheumatologist) or etanercept should be added. A biphosphonate will be added once sure of stomach tolerance to steroids. Will need to check blood pressures and glucose levels. I imagine I will have to deal with here knees (restricted knee flexion and probable OA knees) – and multiple triggers – especially piriformi and subscapularis. B12 shots were taught for this lady.
I want people to realize there are always new options (heck, I have started 3 fairly severe back pain cases on 100 day antibiotics given a positive study on it use).
There however, needs to be the political will to make it happen. Given that every third household has significant chronic pain issues, it is an invisible tip of the iceberg. Our coping-training pain clinic in Saskatoon is closing down due to lack of funding; and our anesthetists have to impose on post operative care (much to the dislike of some staff) to do their blocks in Regina as there is no pain clinic here. Sadly, the same people who ignore this issue will have it slammed in their face – by old age where chronic pain can run rampant – and in if you get dementia, possibly cruely untreated. – So ironic. The medical community will not spare the resources necessary to make 5 day infusions or other advanced treatments possible. This needs to be addressed politically at election time.
Hey – I’m sure I missed plenty – did not tackle psychological treatments and so forth. Surely some people would have stories of what worked for them or their patients…
Addendum:
One review put drug success in Neuropathic pain at 30-40%
Per T. Hansson, et al.
Toward a definition of pharmacoresistant neuropathic pain,
European Journal of Pain, 13(5),2009, 439-440.
“In evidence-based studies on pain it is customary to consider “responders” to treatment those patients that report a pain relief amounting to 30–50%. Meta-analysis (Finnerup et al., 2005) as well as experienced clinicians claim that this goal is obtained in only 30–40% of patients across diagnostic entities where all evidence-based pharmacological strategies have been tried.”

Dear Administrator,
I have had four lumbar surgeries since 2000. The first two were laminectomies/ discectomy of the L-4 / L-5 discs. Both of these were successful. In 2010 I hurt myself lifting an object and compressed my L-5 nerve root. I underwent decompression surgery in 2011 of the L-4, L-5 and S-1 nerve roots and again in 2012 adding spinal stenosis to the list at the L-3 and L-4 levels. Neither one of these surgeries has given me any relief. I have pain along both ankles, the left foot and around my right hip area. I am trying to find out if you can recommend a physician ( in the USA or outside the USA ) who can take a look at my test results and diagnose correctly what is going on with me and hopefully propose a treatment. I recently had an MRI, an EMG and a CT Myelogram but none of them show why I am still having pain. I appreciate any guidance or help you can provide. Thank you.
—————-
Probably one of the more well known pain clinics would be the Messana clinic in Maryland.
http://www.mensanaclinic.com/
20 years ago they published an article on how 2/3 of chronic pain sufferers that were told there was nothing the matter with them – actually had well definable lesions.
http://www.sciencedirect.com/science/article/pii/S003331829371823X
A foot problems with neuralgic level pain could include a dropped cuboid:
http://www.biblio.physiotek.com/sites/biblio.physiotek.com/files/October1994-CS-Mooney.pdf
http://www.alliance-rehabilitation.com/wp-content/themes/alliance/files/ankle/Cuboid-Syndrome-Ankle-Sprains.pdf
And ankle impingement:(one type I discussed below)
http://painmuse.org/?p=1575
and lots others less easily treatable..
Good luck
Thank you very much for your reply. I really appreciate it.
Thank you very much for your comments and information. I really appreciate your inputs.
Hello
I am a resident of Montreal, with CRPS of the elbow at 4 months post-trauma.
I have read the 2013 Verenna article, and it looks very promising (even too good…).
Instead of wasting time (and worsening the prognosis) with ineffective nerve block or other treatment, I would like to find a physician (rheumatologist/neurologist/anaesthesiest…) who would be prepared to administer the Verenna protocol, with the alternative biphosphonate, since pamidronate is not available in Canada. Any suggestions on how to find such a courageous soul?
————————
Sorry – been unable to find Verenna article – please advise. I have had luck with:
1) Ketamine 10 mg every 15 minutes X2 repeatedly twice weekly – this was derived from article I discussed:: Simplest Ketamine Technique Ever for CRPS – Low Dose 10 mg Ketamine Subcut Weekly – http://painmuse.org/?p=695
It improves both pain and mood but needs repeated use.
2) Repeated blocks – probably easiest done by axillary block:
http://upload.wikimedia.org/wikipedia/commons/a/ab/Axillary_block.jpg
you don’t need a great block so just injecting some local in front and on either side of axillary artery is sufficient.. One has to be patient – repeated blocks work like was what necessary for post herpetic neuralgia:
Post Herpes Zoster – Repeated Nerve Blocks within 100 days Works
http://painmuse.org/?p=724
Anyone got better idea?
3) Local therapy depends on what issues are locally
– is there any evidence of entrapment that release might help?,
– how tender are skin nerves that D5W could be injected over top?
– Are there steroid responsive joint or tendonitis issues?
– are there muscles that can be helped by brutal transverse massage?
4) IV pamidronate is indeed available in Canada and considerably cheaper now that it has gone generic – hospitals with cancer clinics use it quite regularly for spinal cancer pains. People who use pamidronate have to have good teeth (rarely causes osteonecrosis jaw) and have to be willing to put up with feeling unwell with flu/aches after first shot especially for maybe a week. Last article I read suggested 4 shots might work best…
Confirmed Again – Biphosphanates Work In Complex Regional Pain
http://painmuse.org/?p=2339
How much is related to neck is important and Intramuscular stimulation (IMS) helped deal with that and some local triggers – you can find a practitioner through the Istop site – Canada is fortunate as Dr. Gunn is from Vancouver so Canadian practitioners are common:
http://www.istop.org/
Really desperate cases can respond to continuous IV lidocaine given in New York or IV ketamine given in Chicago but those would be expensive.
Any other suggestions out there? I liked the IV lidocaine/ketamine given by Dr. Ellen Thompson in Ottawa (might be worth the travel):
http://painmuse.org/wp-content/uploads/IV-with-lidocaine2.jpg
A team approach with anesthesia and physio etc works best but I know how long it takes to get to see a pain clinic – good luck there..
I am an interventional pain management specialist, and I appreciate some of your comments and observation. In my soon-t-be-published text book of peripheral nerve entrapments, I have even included the dorsal scapular nerve that you mentioned in another blog. However, since it is my image of the knee dissection that you are using in this posting (I had a press pass to take images of the Bodies, The Exhibition and then modified the images myself), I would have appreciated at least an attempt at asking permission to use the image (which I would have been glad to provide).
Andrea Trescot, MD
——————
Sorry, that was just rude of me.
admin
Awesome! Its actually awesome post, I have got much clear idea on the topic of from this post.
Pingback: Mulople Sclerosis (MS) Pain Treatment Options | Pain Medical Musing
Pingback: Post Breast Surgery Pain – Clearer Reason It’s Bad – High Prevalence of Neuropathic Pain | Pain Medical Musing
Pingback: Want Do You Do For Desperate Neuropathy? – Implantable Pain Pump | Pain Medical Musing