Sometimes chronic perineal pain comes out of the blue and one could certainly use a secret weapon. Botox to ganglion impar reduced one case of perianal and genital pain from 8/10 to 2-4/10 for months.
Korean J Pain Vol. 23, No. 1, 2010
Ganglion Impar Block With Botulinum Toxin Type A
for Chronic Perineal Pain
Su Jin Lim, MD, Hue Jung Park, MD, Sang Hoon Lee, MD, and Dong Eon Moon, MD
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2884216/
- 40 year old man
- 8/10 pain – perianal, perineal, and genital. – couldn’t sit > 5 min
- Investigations negative
- medical treatments, epidural blocks – no help though analgesic impar blocks helped temporarily
- Block technique: “A subcutaneous infiltration was performed in the superior area of the anococcygeal ligament. This area was chosen as a puncture point. Using a C-shaped image intensifier, a 22 G, 10 cm block needle in which the terminal part was bent at an angle of 30 degrees was advanced to a distance of 6 cm. Thus, attempts were made at the sacrococcygeal junction to reach the anterior surface.”
- Repeated blocks of 80-100 units Botox were used every 2-3 months
- Pain was brought to 2-4/10 with treatments.
Comments: Hitting the ganglion impar is confusing because its location is. One article suggests injecting through the sacrococcygeal joint but that assumes the ganglion is at that level. An autopsy study found the following locations:
Anesthesiology:July 2004 101[1]249-250
Clinical Implications of Topographic Anatomy on the Ganglion Impar;
Oh,Chang-Seok et al free article here
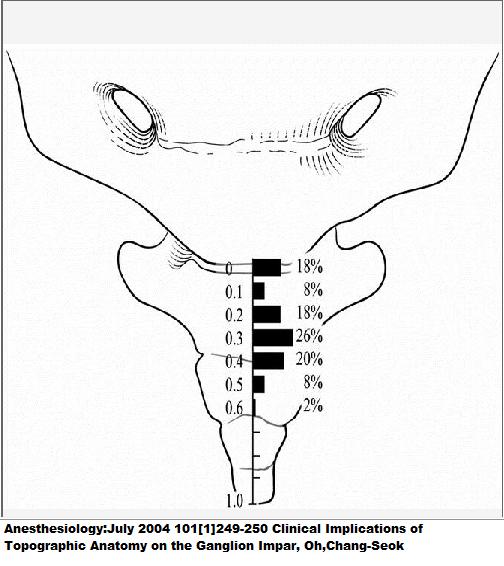
As you can see, the ganglion is more likely to be lower down. They used 0.5% bupivacaine 1 ml with the Botox which I am not sure is too good an idea as it cuts down nerve activity and botox absorption. It is a welcome addition to treatments.

Pingback: New Treatments For Coccygodynia (sore Coccyx) | Pain Medical Musing
New Treatment of Perineal / Pelvic Pain – Botox to Ganglion Impar
Regarding the news above, I’m actually the exact person who was the patient to Botox injection. I have pain right on impar and since then I’m receiving Botox every 5 month.
Without botox, no idea how to control the pain, might commit suicide, too painful to endure.
I also received radiofrequency ablation there one time, but it did not help, so I’m on Botox now for 3 years. And it has steadily reduced the pain so that I work as a fulltime researcher in oceanography.
My questions are
1) why ablation did not work for me? worth trying another round because of #2
Dr. Moon said it may not work for patients who have pain right on the impar. Is that so?
2) I received botox a few days ago, but the doctor pushed too much and pork the nerve, damaging the nerve. Following I’m having more pain with chills. ANd have to wait some time (weeks hope or months) until the pain comes down as botox fights the pain. WHat shall I do?
3) regarding your comment on the procedure, can you explain more in detail why do you think that way? “As you can see, the ganglion is more likely to be lower down. They used 0.5% bupivacaine 1 ml with the Botox which I am not sure is too good an idea as it cuts down nerve activity and botox absorption. It is a welcome addition to treatments”
—————
It sounds like you are in considerable pain and I would like to help but it is pretty unclear what exactly you have:
– Is there lower abdominal pain associated? If so, I find injecting the pyramidalis muscle makes a difference see article
http://www.stacommunications.com/journals/pdfs/cme/CMEfebruary2003/pelvicpain.pdf#search=%22Magali%20Robert%20calgary%20pelvic%20pain%22
– Are there pelvic muscle spasms?;
If so having them massaged by a proper therapist would help.
Initial article finding it helped in urinary frequency syndromes was here:
Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome
JM Weiss et al
Journal of Urology,Vol 166, Dec. 2001.p2226-31 fee article here with illustations of how to do it:
http://www.jmweissmd.com/pdf/JMW_Pelvic_Floor_Myofascial_Trigger_Points.pdf
Physiotherapy approach for men was furthered in
THE JOURNAL OF UROLOGY July, 2005, p. 155-160
INTEGRATION OF MYOFASCIAL TRIGGER POINT RELEASE AND PARADOXICAL RELAXATION TRAINING TREATMENT OF CHRONIC PELVIC PAIN IN MEN
RODNEY U. ANDERSON, DAVID WISE, TIMOTHY SAWYER, AND CHRISTINE CHAN
From the Department of Urology (RUA, CC), Stanford University School of Medicine, Stanford, Sebastopol, (DW) and Los Gatos (TS)
free article here:
http://www.prostatitis.hostei.com/docs/stanford2005.pdf
The success of this line of treatment was confirmed by a randomized multicenter control group trial:
J Urol. 2013 Jan;189(1 Suppl):S75-85. doi: 10.1016/j.juro.2012.11.018.
Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes.
Fitzgerald MP, Anderson RU, Potts J, Payne CK, Peters KM, Clemens JQ, Kotarinos R, Fraser L, Cosby A, Fortman C, Neville C, Badillo S, Odabachian L, Sanfield A, O’Dougherty B, Halle-Podell R, Cen L, Chuai S, Landis JR, Mickelberg K, Barrell T, Kusek JW, Nyberg LM
abstract here:
http://www.sciencedirect.com/science/article/pii/S0022534712002595
This program was honed down to a 6 day program:
J Urol. 2011 Apr;185(4):1294-9.
6-day intensive treatment protocol for refractory chronic prostatitis/chronic pelvic pain syndrome using myofascial release and paradoxical relaxation training.
Anderson RU, Wise D, Sawyer T, Glowe P, Orenberg EK.
abstract here:
http://www.ncbi.nlm.nih.gov/pubmed/21334027
There are studies demonstrating self massage makes a real difference as well: This one is with mostly male patients:
Clin J Pain. 2011 Nov-Dec;27(9):764-8.
Safety and effectiveness of an internal pelvic myofascial trigger point wand for urologic chronic pelvic pain syndrome.
Anderson R, Wise D, Sawyer T, Nathanson BH.
Free article here:
http://www.multibriefs.com/briefs/aaoorg/MFTriggerpointpelvicpain.pdf
The only commercially available product I could find was something called the Crystal wand – one site selling it here:
http://www.cmtmedical.com/index.php?main_page=product_info&products_id=420
Without the full curve though, you will not be able to reach triggers in obturator internus anteriorly:
http://www.scielo.br/img/revistas/ibju/v35n3/3a10f01.jpg
Is the back a player?
If so, work on back, sacroliac and piriformis areas might make a differernce.
Does it hurt badly to sit down?
This is a condition called pudental neuropathy
This is a big topic. Here is a good power point discussion:
http://www.canadianpainsociety.ca/congres/calgary2010/Presentations/Session302_StanleyAntolak.pdf
For women does the pain vary with menstrual cycle? –
if so, depo provera shots to inhibit cycle supplemented with daily estrogen to prevent osteoporosis would help (or just on one of the continuous birth control pills)
Is the bladder affected (having to pee often)? – if so, in women treating interstitial cystitis would help. In men, injecting botox into the prostate might help.
I have a whole section on IC: – even the food you eat could have some effect
http://painmuse.org/?cat=5
Above pelvic floor technique work for bladder as well.
Is the tailbone affected?
This is a tougher issue and steroid injection only work in recent cases. I have discussed this issue before including not bad results from tailbone removal.
New Treatments For Coccygodynia (sore Coccyx)
http://painmuse.org/?p=2073
Is the perineal skin sore?
I have a list of measures for women with vulvar area problems:
Vulvodynia Therapy Patient Resource
http://painmuse.org/?p=187
It is becoming increasingly recognized that the blood vessel and accompanying sympathetic nerve are seriously damaged in severe pain. One recent study of severe forearm pain went to the extent to remove the fatty tissue and blood vessels under the skin in the sore area:
Journal of Trauma and Acute Care Surgery: June 2012 – Volume 72 – Issue 6 – p 1647–1653
Surgical treatment of complex regional pain syndrome type II with regional subcutaneous venous sympathectomy
Happak, Wolfgang MD; Sator-Katzenschlager, Sabine MD; Kriechbaumer, Lukas K. MD
abstract here:
http://journals.lww.com/jtrauma/Abstract/2012/06000/Surgical_treatment_of_complex_regional_pain.33.aspx
I suppose this explains why in women remove of the painful Vulvar skin by surgery is so effective for vulvodynia:
Eur J Obstet Gynecol Reprod Biol. 2005 May 1;120(1):91-5.
Modified vulvar vestibulectomy: simple and effective surgery for the treatment of vulvar vestibulitis.
Lavy Y, Lev-Sagie A, Hamani Y, Zacut D, Ben-Chetrit A.
abstract here:
http://www.ncbi.nlm.nih.gov/pubmed/15866093
There are those that do not think surgery works:
Focal vulvitis: a psychosexual problem for which surgery is not the answer.
Journal of Psychosomatic Obstetrics & Gynecology 1995, Vol. 16, No. 2 , Pages 85-91.
M.J. deJong1†, R. H. W. van Lumen2, E. A. Robertson3, L. N. E. Stam2 and F. B. Lammes
abstract here:
http://informahealthcare.com/doi/abs/10.3109/01674829509042783
Several topical on skin cream agents can be used for skin level pains: –
gabapentin:
New Treatment For Vulvodynia – 6% Gabapentin in Lipoderm
http://painmuse.org/?cat=5
ketamine-amitriptyline for genital pains:
Pain Physician. 2012 Nov;15(6):485-8.
Topical amitriptyline-ketamine for treatment of rectal, genital, and perineal pain and discomfort.
Poterucha TJ, Murphy SL, Rho RH, Sandroni P, Warndahl RA, Weiss WT, Davis MD
free article here:
http://www.painphysicianjournal.com/2012/december/2012;15;485-488.pdf
Topical lidocaine for even tail bone pains:
Topical Lidocaine for Coccydynia
http://painmuse.org/?p=1342
The superficial sore skin can be injected with just plain 5% dextrose in a technique coined neuroprolotherapy. You can also inject strong local anesthetic – 5% lidocaine with perhaps some numbing effects (would be painful for few days though) – a technique devised by a doctor Choi:
Reg Anesth Pain Med. 1998 Jan-Feb;23(1):96-100.
The use of 5% lidocaine for prolonged analgesia in chronic pain patients: a new technique.
Choi YK, Liu J.
abstract here:
http://www.ncbi.nlm.nih.gov/pubmed/9552786
I have found botox shots only partially effective in neuropathic pain though have not done ganglion injections. For occipital neuralgia and trigeminal neuralgia I found I had to supplement injections with several weekly deep (in your case ganglion) injections of 5% lidocaine by Dr. Choi’s technique.
Now, to answer your questions:
Ablation might be useful if local anesthetic block could repeatedly give relief. It is possible the ablation missed because as I mentioned, some people have the ganglion impar lower down:
http://painmuse.org/?p=334
and
http://painmuse.org/?p=1351
If you had chills after the last injection maybe your rectum was penetrated. I do not feel tihis is a big issue as people having prostate biopsies have 12 penetrations done. However, you might consider asking to go on Cipro antibiotics before and for a couple days after a shot if concerned.
If you are not better, I would move on to recommendations above including 5% lidocaine injection into ganglion impar.
A recent study did not find local reduced effect of Botox:
Adding Lidocaine to Botox Might Not Affect Potency
http://painmuse.org/?p=1794
You stated you did not understand something about the procedure but were not specific.
I would never expect one process to treat chronic pain. Your pain sounds very neuropathic. I would wonder if gabapentin would help, particularly if augmented with frequent B12 shots (the combo works better in the animal model with even oral meds)
Proc West Pharmacol Soc. 2004;47:76-9.
Oral administration of B vitamins increases the antiallodynic effect of gabapentin in the rat.
Reyes-García G, Caram-Salas NL, Medina-Santillán R, Granados-Soto V
abstract here:
http://www.ncbi.nlm.nih.gov/pubmed/15633618
http://painmuse.org/?p=1420
If the pain is so bad it can make you suicidal, then you need a good painkiller – methadone is probably the best for severe pain as it affects both mu receptors and NMDA receptors.
I have found regular ketamine shots work well for severe pains with prominent mood issues but it is not a treatment for people with bladder issues:
Simplest Ketamine Technique Ever for CRPS – Low Dose 10 mg Ketamine Subcut Weekly at:
http://painmuse.org/?p=695
and
Depression is a Form of Pain and Ketamine May be a Cure if One Can Make It Last
http://painmuse.org/?p=1420
Interestingly, my use of ketamine was initiated by Dr. Antolak who was using it in the pudental neuralgia /can’t sit patients.
At a recent Canadian Pain Society meeting, people with conditions like yourself are often very depressed. Depression turns up the volume on pains and NEEDS TO BE TREATED; Suicidality can happen and makes it time to consider sacral nerve stimulation – a rather simple procedure for perineal pain where you have electrical stimulation done through your sacral level:
International Urogynecology Journal August 2000, Volume 11, Issue 4, pp 231-236
Patient Satisfaction and Complications Following Sacral Nerve Stimulation for Urinary Retention, Urge Incontinence and Perineal Pain: a Multicenter Evaluation
K. Everaert, D. De Ridder, L. Baert, W. Oosterlinck, J. J. Wyndaele
abstract here:
http://link.springer.com/article/10.1007%2Fs001920070031?LI=true
I’m sure there are physicians more specialized in this area then I; and I would be interested in their comments.
thank you so much for detailed replies.
My problem is the pain is shooting up from ganglion impar, the pain referred in all over the body. Most difficult is abdominal neuropathic pain, and no medication will work.
I feel ablation would be the best if the ganglion is exactly located. Last time I had internal sun burn pain following the procedure that lasted a couple of weeks, quite a difficult pain to endure and that is what I’m afraid of. It is more likely for high temperature ablation than done at low T.
I don’t think the needle puncture the rectum, but the nerve itself. The nerve has become very sensatized, sending pain signal upward.
—————————–
If you are getting abdominal pains, this is no longer just a ganglion impar issue.
– You may have an irritable bowel and issues that go with that. Dietary changes, amitriptyline, exercise, and hypnosis/yoga/meditation are good initial treatments for that.
– very likely there are abdominal wall triggers – one that gives neuropathic level pain is where the iliolumbar nerve penetrates subskin layers:
http://img.medscape.com/pi/emed/ckb/clinical_procedures/79926-81306-82983-1508747tn.jpg
If you lie down and lift your head up while pressing on the spot, you can see how tender it is.
– one would wonder if the joint where the pubic bones meet is sore:
http://painmuse.org/?p=291
– I have a couple of ladies with neuropathic level abdominal pains at times that both had inguinal hernias missed for years:
http://painmuse.org/?p=1086
I cannot believe you would have ganglion impar issues, and abdominal pains without having considerable pelvic floor muscle issues – I have expanded in original note on that.
When I deal with issues such as yours, I usually end up with a list of 5-10 problems – all of which need dealing with – dealing with abdominal wall issues and pelvic floor issues would be a start but each of the issues mentioned in this and prior note would need attention. I’m afraid I feel overwhelmed by possiblities and you need to see a doctor who knows how to deal with the pelvis – maybe check if there is a pelvic pain society in your country and see if you can find someone locally from their membership. good luck
I went through two Botox injections today and last monday, the only difference being the previous one done through transacrosscoyxial (a junior doctor) and today by following the way as originally performed by Plankarte (by a professor). He noted that Botox may not reach as down if done trans- way. I’ll let you know how I feel in a few days.
I was in depression these days, especially today as it seemed botox is not potent enough to block the pain. We are pretty much sure that the pain is of neuropathic along the ganglion impar. I talked to the prof about RF, but he said he is not willing to as the pain source may be wider than to be covered by RF. He showed when asked about by me the RF picture done a couple of years ago. He said it was correctly located.
Now as you suggest if botox is not working (yes it works, but it takes fairly long to suppress if the nerve damage is severe, as was for me), I’ll ask for lidocaine (5%) for neurolysis.
The questions for you are
1) what is the advantage of blending lidocaine with botox than just botox?
2) what are the advantages of using lidocaine over alcohol or phenol or any other known agent are with respect to safety and destruction of other parts around the impar?
———————————–
1) Concentrated lidocaine is quite acidic (ph around 4) and I think its acidity is part of its neurolytic power. That might denature the botox and make it worthless.
2) Phenol can cause painful numb dysesthesias “anesthesia dolorosa” – this varies for 0-23% according to
Pharmacology of Phenol Injections
in J Frangiamore, C O’Brien – Dystonia: Etiology, Clinical Features, and Treatment 2004
http://books.google.ca/books?hl=en&lr=&id=bMKypn_B0tIC&oi=fnd&pg=PA113&dq=phenol+nerve+dysesthesias+rate&ots=NRGuLsIXyM&sig=RsIJwygxPBe2Ch5NETlpOUfhp_Y#v=onepage&q&f=false
Some studies have either not found any cases:
Journal of Neurosurgery May 1999 / Vol. 90 / No. 5 / Pages 828-832
Trigeminal nerve peripheral branch phenol/glycerol injections for tic douloureux
Harold A. Wilkinson, M.D., Ph.
http://thejns.org/doi/abs/10.3171/jns.1999.90.5.0828
or found them low:
American Journal of Physical Medicine & Rehabilitation: July 2008 – Volume 87 – Issue 7 – pp 556-566
Safety Profile of Multilevel Chemical Denervation Procedures Using Phenol or Botulinum Toxin or Both in a Pediatric Population
Kolaski, Kat MD; Ajizian, Samuel J. MD; Passmore, Leah MS; Pasutharnchat, Nath MD; Koman, L Andrew MD; Smith, Beth P. PhD
http://journals.lww.com/ajpmr/Abstract/2008/07000/Safety_Profile_of_Multilevel_Chemical_Denervation.5.aspx
The dysesthesias according to first reference “most will resolve within 3 months”. Have seen one case and indeed it did resolve; it however made me fearful of phenol.
Alcohol injections are perhaps safer but do wear off over time.
Quite by accident, today I came across a review of ganglion impar block in a Jan 2013 issue:
Ganglion Impar Blockade: A Review
Julian Trevor Scott-Warren, Victoria Hill, Anand Rajasekaran
Curr Pain Headache Rep (2013) 17:306
They made the following point:
“Oh et al [1] note in their anatomical study of the ganglion impar that branches from the ventral ramus of the sacral nerve run close to the ganglion in 3 of their 50 samples. They suggest therefore that the amount of neurolytic agents used be minimized to avoid possible injury of the sacral nerve branch. ”
5% lidocaine is a gentler agent and I call it the sticky note of neurolytic agents – it may not take unless given several times but does not have the destructive power to hurt you. Spinal lidocaine 5% is used and it has 7.5% dextrose in with it.
Having said that, alcohol through the first inter-coccygeal joint does sound tempting as long as you could just use 0.5 ml – and found that anesthetic block confirmed that was the source of your problem.
The second botox injection was more effective, strongly reacting to nerve pain and significantly reducing the pain.
A problem is that the nerve is so damaged (it’s like a pin) sending off sharp pain signal (although less after botox injected) especially after sitting on chair as sitting presses the nerve.
alcohol will also denature botox too, right?
Will such neurotic pain go away with alcohol?
———————————–
I use botox to treat occipital neuralgia which has sharp pain “zingers”. It helps some but does not take them away. A couple shots of 5% lidocaine after the botox helps there. I wonder whether the sacral nerve branch was hit in one of the injections and that is where these zingers are coming from. One whould think alcohol should too if prior local anesthetic block gave temporary relief.
I think the pain travels along the sympathetic chain from the impar. I had a hard time for bowel today, contracting the rectum many times. And now it sends pain signal along the sympathetic chain again with mild chills and cramping (they were stronger a few days ago when I sit for couple of hours).
My options are
1) waiting and enduring the pain until botox has sufficiently reduce the inflammation on the nerve ( for how long?, and I have to work a new job next week)
2) ask my doctor to inject alcohol (not sure he will do because he has seen side effects), but the target must specific not to hurt other nerves. And if not affective for reasons when injected, I need to be assured that botox would still work for the pain as a backup.
A related question is how serious the side effects of alcohol injection are, if it happens?
Can doctor locate the area of the nerve of pain by putting his finger through my rectum? As ganglion impar can be located variably individually.
——————————
You can reach the sacro-coccygeal joint rectally and the first ganglion impar block I did trans sacro-coccygeal joint, I gauged the depth of the needle by a rectal finger feeling the needle coming through the other end (fortunately without penetrating rectum).
-admin
I met my pain doctor today about alcohol neurolysis on ganglion impar. He said he is concerned about neuritis following denervation with alcohol, and I may end up with more pain. And he suggested to wait for unknown time (basically endure with the pain until next week at least or much longer when botox is fully effective- I think its effect is already in full strength as it’s been a week) .
A couple of days ago I emailed with another doctor at another university with extensive experience on alcohol injection, and he said it could be very beneficial.
I was going to see this doctor this Friday to receive alcohol injection.
I know this is not good to see two doctors, but my doctor seems to underestimate my pain. And I simply can’t sit on chair as it press the nerve, causing almost unbearable pain.
How serious the neuritis would be? Even if there is some, I’m willing to take it.
_________________________
Neuritis could be bad. It would be much safer to start with a semi-neurolytic agent that would not cause neuritis – to start with: that would include
Lidocaine 5 – 10%; the 5% is available as spinal injectable if that is still used in your country.
or 10% tetracaine – it comes in a vial as a powder and can be made 10% usually but cutting fluid mix to 0.5 ml
Here are 4 articles where they have been used – maybe ask that one of these be tried first.
The Use of 5% Lidocaine for Prolonged Analgesia in Chronic Pain Patients: A New Technique
Young K. Choi, M.D., F.A.C.RM., and Joseph Liu, M.D.
Regional Anesthesia and Pain Medicine 23(1): 96-100, 1998
Efficacy and safety of high concentration lidocaine for trigeminal nerve block in patients with trigeminal
neuralgia
Int J Clin Pract, February 2008, 62, 2, 248–254
K. R. Han, C. Kim, Y. J. Chae, D. W. Kim
Pain Clinic, Department of Anesthesia and Pain Medicine, Ajou University Hospital, Suwon, Korea
Correspondence to:
Chan Kim, MD,
Department of Anesthesia and Pain Medicine, Ajou University Hospital,
San 5 Won-Cheon Dong Pal-Dal Gu, Suwon 442-721, Korea
Tel.: + 31 219 5896
Fax: + 31 219 5579
Email: kimchan@ajou.ac.kr
Intercostal Nerve Block With 5% Tetracaine for Chronic Pain Syndromes
Katsushi Doi, MD,* Tetsuro Nikai, MD,† Shinichi Sakura, MD,‡ Yoji Saito, MD§ Japan
Journal of Clinical Anesthesia 14:39–41, 2002
The long lasting effects of peripheral nerve blocks for trigeminal neuralgia using a high concentration of tetracaine dissolved in bupivacaine
Fumio Gotoa,*, Keiji Ishizakia, Daisuke Yoshikawaa, Hideaki Obataa, Hidehiro Ariib, Masamitsu Teradab
Pain 79 (1999) 101–103
Might be an idea to talk to the Korean article contact – it is only 5 years old.
I made an appointment with Dr. Kim Chan Friday morning to discuss their findings. In their paper, they say “Trigeminal nerve block with high concentration lidocaine (10%) is capable of achieving an intermediate period of pain relief, particularly in patients with lower pain intensity and shorter pain duration prior to the procedure.”
They say it works for lower pain intensity.
My concern is whether it would be strong enough to further down the pain for prolonged period, given strong lidocaine may denature botox as you said.
————-
5-10% strong lidocaine would denature botox if same syringe at time injected not regular lidocaine though
One professor said yesterday that he has extensive use of lidocaine , and its effect is limited and short-lived (1-4 weeks only).
He mentioned the lidocaine papers were initiated because the authors were concerned with repeated use of alcohol.
He suggested not to use alcohol (only for cancer patients) and endure pain until it calms down with botox (for how long I don’t know until I can comfortably sit, and I have to work now).
Will there be a treatment if neuritis happens with alcohol?
Another doctor who has extensive use of alcohol and I will meet him Friday also mentioned that for some patients alcohol will increase the pain, so he diagnoses first with anethestic.
——————————–
Is longer lasting after Botox but requires up to 3 weekly injections sometimes to get a good take. If you got a good temporary response to concentrated lidocaine, then I would try alcohol.
admin
Pingback: Ama Botox | Common Botox Effects
Pingback: Botox Clinic Potts Point | Botox Effects