Radiofrequency to coccyx interdisc, pulsed radiofrequency to ganglion impar, and coccyx removal are all being used in recalcitrant cases.
I have had letters of unsatisfactory coccyx pain case and have included some more advanced measures:
Though prior studies have failed to find much MRI features, a recent study found significant findings:
Eur Spine J. 2012 Feb 22. [in press]
Magnetic resonance imaging findings in the painful adult coccyx.
Maigne JY, Pigeau I, Roger B abstract here
- 172 cases severe chronic coccydynia
- 70 cases (40%) disc abnormalities – intradisc fluid (17), Modic 1 end plate changes (38), or uncetain changes (15)
- Tip of coccyx abnormalities – 41 (24%) – 13 soft tissue inflammation, 18 venous dilatations, ambigious 13
- vertebral bone edema 5;
- benign tumor 1
- rigid coccyx cases were more likely to show coccyx tip abnormalities while mobile coccyx cases more likely a disc lesion:
“the 105 cases with a mobile coccyx mainly presented abnormal features mainly in a disc (63 cases vs. 4 cases for the tip), whereas
the 67 patients with a rigid coccyx mainly showed abnormal features at the tip (37 cases vs. 7 for the joints, p < 0.001)”.
Hence ascertaining whether coccyx mobile or not is useful.
In a disc case, they found radiofrequency ablation of the intradiscal joint followed by injection 20 mg methylprednisolone was helpful:
Pain Pract. 2011 May-Jun;11(3):278-81.
Radiofrequency ablation within the first intercoccygeal disk for coccygodynia: a case report.
Scemama P, Shaparin N, Kaufman A, Dua S. abstract here
- 44 year oold lady with 1 year history of a fall
- Confirmations included:
– localization of her pain at the disk between the 1st and 2nd coccygeal vertebrae.
– provocation with needle puncture or area
– local injection of 40 mg of methylprednisolone gave 3 weeks relief - Radio frequency ablation (RFA) was then carried out at 70°C for 80 seconds, followed by injection of 20 mg of methylprednisolone.
- 70% relief for 6 months (initially 9/10 Pains to 3/10 after)
For a case of uncertain origin of the pain, pulsed radiofrequency to ganglion impar offered relief:
J Pain Symptom Manage. 2010 Jun;39(6):e1-2.
Fluoroscopically guided ganglion impar block by pulsed radiofrequency for relieving coccydynia.
Usta B, Gozdemir M, Sert H, Muslu B, Demircioglu RI.
- 54 years old with 5 year coccyx pain unrelieved by usual measures
- did do trial block with 3 ml 1% lidocaine through transsacrococcygeal disc and I presume it helped temporarily though they did not say.
- “SMK-10 needle (NeuroTherm 22G, UK) with an active tip of 5 mm was inserted through the sacrococcygeal disc to the anterior surface of the coccygeal disc, with the guidance
of anteroposterior and lateral fluoroscopy” - 42 degrees centigrade for 240 seconds.
- pain initially 8/10; was 0/10 initially , the 1-2/10 thereafter
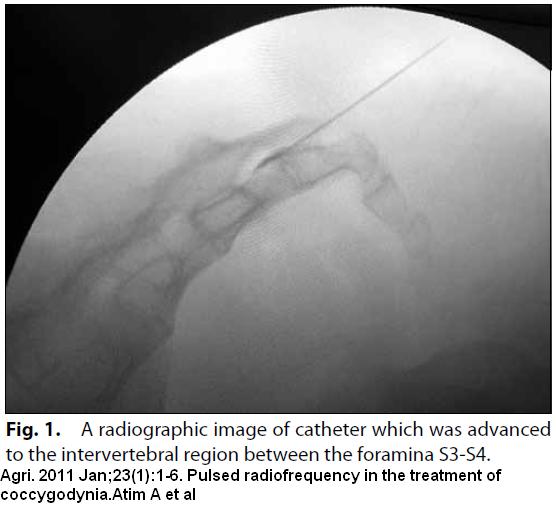
>Agri. 2011 Jan;23(1):1-6.
Pulsed radiofrequency in the treatment of coccygodynia.
Atim A, Ergin A, Bilgiç S, Deniz S, Kurt E. free article here
- 21 cases average age 40 – five times more likely in women
- pain during sitting or standing up from a chair
- sedation by 0.02 mg/kg midazolam (1.4- 2 mg)
- coccyx is innervated by anterior branches of S4 and S5 spinal nerves and anterior branch of coccygeal spinal nerve
- local to skin
- Cannula was advanced to the intervertebral region between the foramina S3-S4 with anteroposterior fluoroscopic imaging.
- Pulse radiofrequency – 180 seconds avoiding temperatures above 42°C. – in caudal space
- In the 16 cases without surgery, pain level was initially 9/10 and dropped to 1.5/10 at 3 weeks and 6 months.
- In the 5 cases with prior sugery, pain dropped from 9/10 initially to 4 /10 at 3 weeks and 5/10 at 6 months
- All together, 81% was considered successful at 6 months.
For those unresponsive to any other therapy , coccygectomy (tailbone removal) is still done:
Chin J Traumatol. 2011 Feb 1;14(1):25-8.
Coccygectomy for stubborn coccydynia.
Cheng SW, Chen QY, Lin ZQ, Wang W, Zhang W, Kou DQ, Shen Y, Ying XZ, Cheng XJ, Lü CZ, Peng L. abstract here
- followed up for 1 to 6 years (mean 3.3 years)
- 31 cases
- excellent in 20 patients (64.5%), good in 7 patients (22.6%), moderate in 3 patients (9.7%) and poor in 1 patient (3.2%)
- Getting an overall good-excellent rate of 87.1%, they felt procedure was worthwhile
- couple superficial wound infections
Given that results are generally good from surgery, particularly for prior trauma, it was suggested people not wait so much:
Injury. 2007 Oct;38(10):1183-8. Epub 2007 Apr 6.
Coccygectomy for coccygodynia: do we really have to wait?
Cebesoy O, Guclu B, Kose KC, Basarir K, Guner D, Us AK. abstract here
“coccygectomy is a reliable method of treatment with a high satisfaction and a low complication rate.”
Comment – There are a variety of treatments available:
- Good sites to look at would be :
http://www.coccyx.org/
and of course Dr. Maigne in France:
http://www.sofmmoo.com/english_section/7_coccyx/coccyx_photos/accueil_coccyx.htm
- I find the tip of tailbone is often tender (apparently more in rigid coccyx cases) and steroid to area could help –
- Where intradiscal pains are present, steroid inject into disc area, followed by rhizotomy (if temporary relief) could be valid.
- Overall, Ganglion impar injections could be useful and I have discussed this elsewhere:
Ganglion Impar Injection For Tailbone Coccydynia - Botox injections to the ganglion may give more lasting relief:
New Treatment of Perineal / Pelvic Pain – Botox to Ganglion Impar
- Now it looks like simple pulse radiofrequency to ganglion thru sacro-coccygeal joint may work as well.
- What I can’t ignore, is how a coccygectomy (tailbone removal) could work as well…
Any comments welcome…

Good Luck trying to get a HELP if workers compensation is involved after suffering “Tailbone Injury” their WCB medical consultant states, fractured tailbone usually does not require any treatment, it heals on its own, without any treatment.
There seems to be a consensus here in Saskatchewan with ortho surgeons, neurosurgeons, and especially WCB, the pain is all in your head, and your just a malingering faker out to abuse the system for free money;
At the website; Kemper Tailbone Foundation; “VIDEO” on the top right; video link below; Dr. Kemper has coined the phrase, saccrococcygeal syndrome;
http://www.ktif.info/
”Dr. Kemper, (or I should say, the narrator) describes the pain ”
from sacrococcygeal syndrome as a ; ”PINCHED NERVE OR WORSE”
I can personally verify, if you have this problem, start looking for a gun
because suicide will become an everyday thought; I left S’toon and within 20 minutes of sitting I was begging my wife to let me, end this fkin nightmare;
That’s How Bad The Pain Is; It’s no JOKE;
Other video on Y-tube by Erik Dalton, ends with, ”Then there is a problem.”
http://erikdalton.com/coccyx-seat-of-soul/
FYI:In BC Canada, Injured truck driver, had coccyx injury. Even though he had numerous, radiological investigation, MRI, CT scan’s, X-Rays, Bone scans, Dynamic sit-stand x-rays, etc.
Only surgery was able to properly diagnosis the severity and extent of injury;
At surgery, the ortho surgeon FOUND;The tailbone was Grossly Hypermobile, and had fractured through, well read it yourself;
(In his October 17, 2001 report Dr. S noted the worker’s advice that his pain was actually worsening. He advised the worker that he did not meet the criteria to warrant excision of the coccyx. He commented the worker was well aware of the problems with regard to surgery as well as the higher rate of infection and difficulty in eradicating pain when the coccyx was not grossly mobile and the pain source could not been localised. Dr. S indicated the worker’s recovery had plateaued. He considered the worker was not likely to improve any further and was likely to live with the chronic disability caused by ongoing constant coccydynia.)
In his January 9, 2002 report Dr. P2, an orthopaedic surgeon, noted that the worker came to see him regarding the advisability of removing his coccyx. He noted the worker’s belief that there was “luxation of the coccyx between the 1st and 2nd coccygeal segment.” Dr. P2 indicated that it would not be in the worker’s best interest to have the coccyx removed, as the surgical trauma was likely to increase his chronic pain syndrome.
In a September 11, 2002 claim log entry the case manager (workers comp) noted that she had advised the worker coccyx surgery would not be approved as the worker’s previous specialists did not expect he would benefit from surgery.
In his September 18, 2002 report Dr. P3 indicated that the worker had exhausted non‑operative management and had ongoing pain and clicking. He thought a coccygectomy was reasonable.
In his operative report documenting the worker’s October 23, 2002 surgery Dr. P3 indicated that the most distal coccyx segment was grossly mobile. He also noted a section of the coccyx had fractured “through the cartilage joining the next segment.”
Dr. H indicated in his April 14, 2003 letter that the worker’s recovery had not progressed as well as expected and he remained unable to return to work. He considered the worker continued to suffer from severe protracted chronic daily pain. He noted the worker was unable to sit and required daily use of regular potent chronic medication which might affect his alertness and impair his ability to drive safely and work at other occupations. He urged a reconsideration of the worker’s eligibility for disability benefits.
WCAT-2003-04102 (Re), 2003 CanLII 70455 (BC WCAT)
and again;
WCAT-2008-02021 (Re), 2008 CanLII 50181 (BC WCAT)