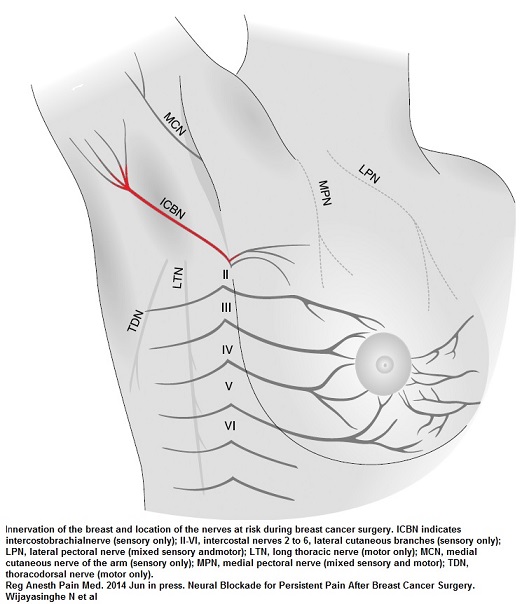
Injury to the Intercostobrachial nerve following breast cancer surgery helps trigger the persistent neuropathic pains after. Why don’t we hear much about it? Here is some info on it.
Following breast cancer surgery, pain is very common. One article divided the causes into:
Intercostobrachial neuralgia 33%
Scar neuroma 39%
Post amputation Phantom pains 22%
as mentioned in
Effet de la kétamine dans la prévention des douleurs chroniques post-mastectomies. Étude pilote
M. Crousier, V. Cognet, M. Khaled, P.-Y. Gueugniaud, V. Piriou
Annales françaises d’anesthésie et de réanimation 27(12) 987-993 – December 2008 abstract here
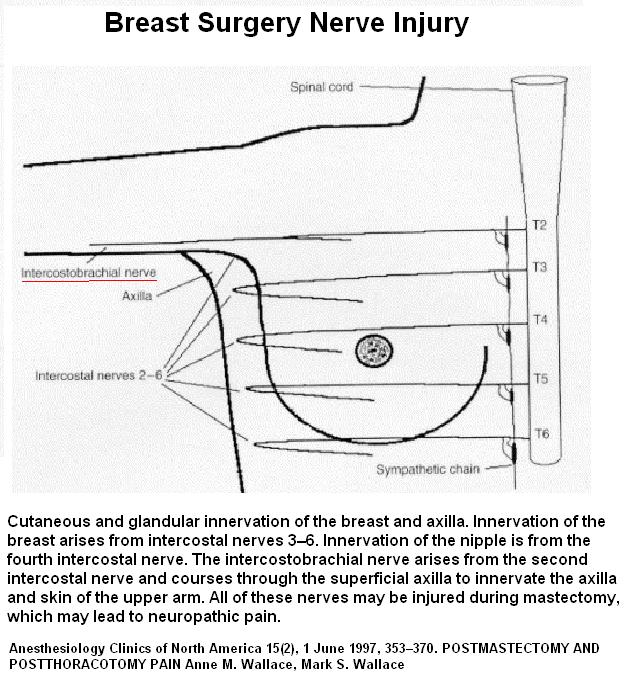
It has been written that between 80-100% of time the intercostobrachial nerve is damaged by breast cancer surgery – and those who had a lumpectomy – let us not forget the axillary node dissection. (as written in:
Anesthesiology Clinics of North America 15(2), 1 June 1997, 353–370.
POSTMASTECTOMY AND POSTTHORACOTOMY PAIN
Anne M. Wallace, Mark S. Wallace brief writeup here )
Along with this it has been written that “Post-mastectomy pain syndrome (PMPS) is experienced by 20–65% of patients who undergo breast surgery for cancer.”
Pain Volume 108, Issue 3, April 2004, Pages 294–296
Some cases of severe post-mastectomy pain syndrome may be caused by an axillary haematoma
Cornelia Blunta, Angelika Schmiedel abstract here:
A 2009 article stated “Chronic neuropathic pain affects between 20% and 50% of women after their breast cancer treatment.”
Chronic Neuropathic Pain in Women After Breast Cancer Treatment
Fozia Bokhari, Jo-Ann V. Sawatzky
Pain Management Nursing Volume 10, Issue 4, December 2009, Pages 197–205
http://www.sciencedirect.com/science/article/pii/S152490420800088X
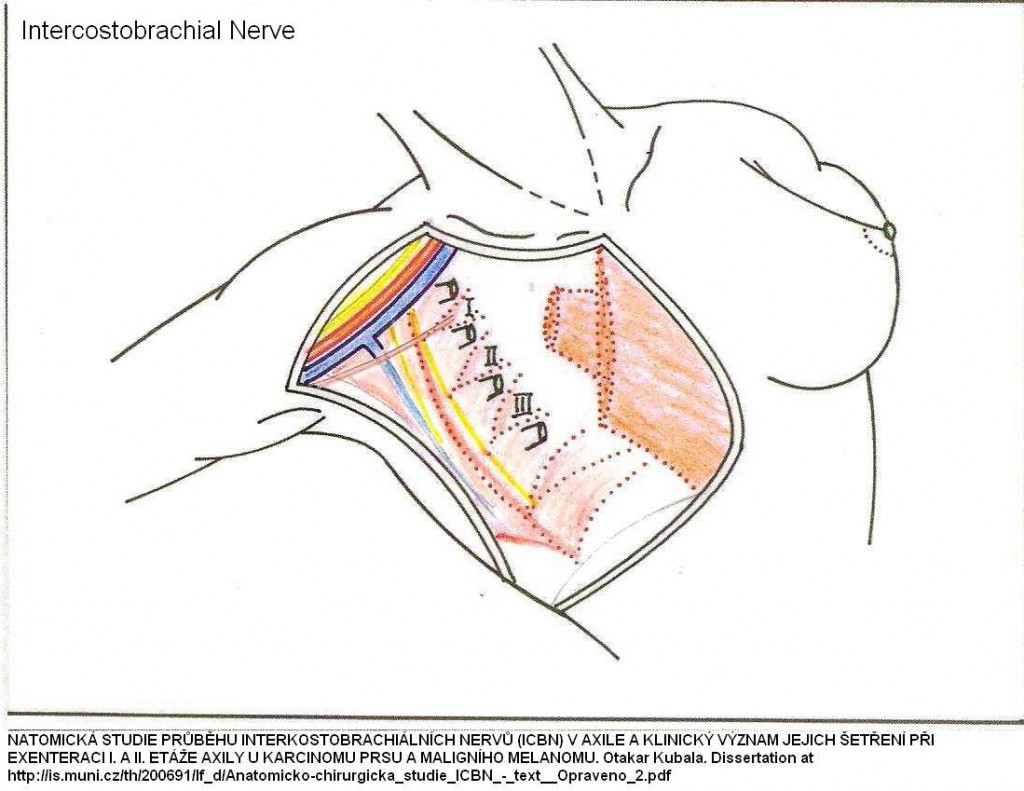
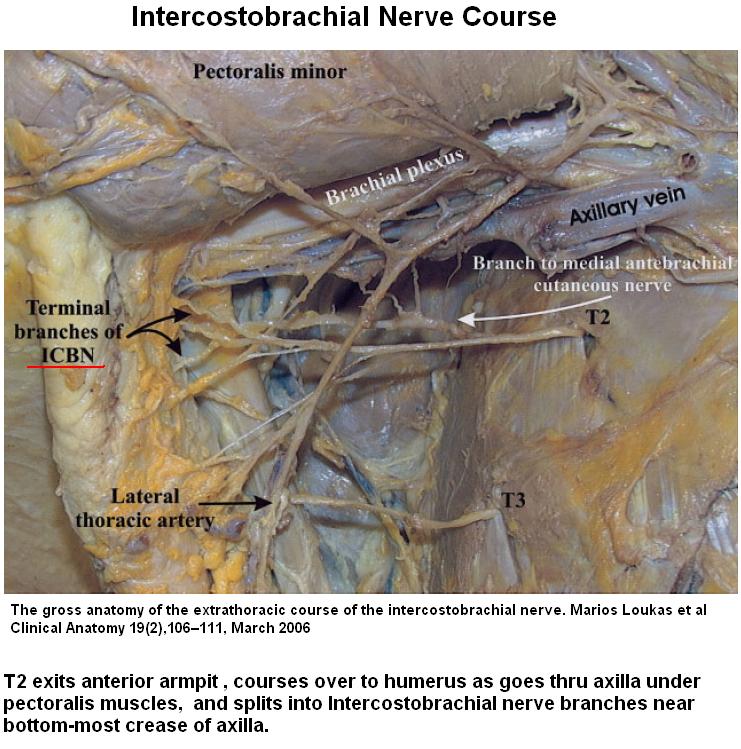
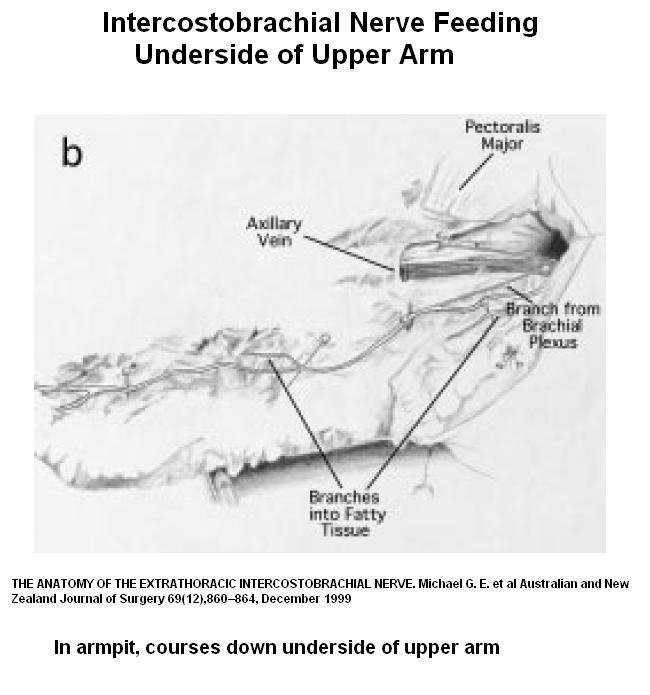
Anatomy of Intercostobrachial Nerve.
It comes out at T2 intercostal space in anterior axillary lline – look for tenderness there:
It comes out the 2nd rib intercostal space at anterior axillary line:
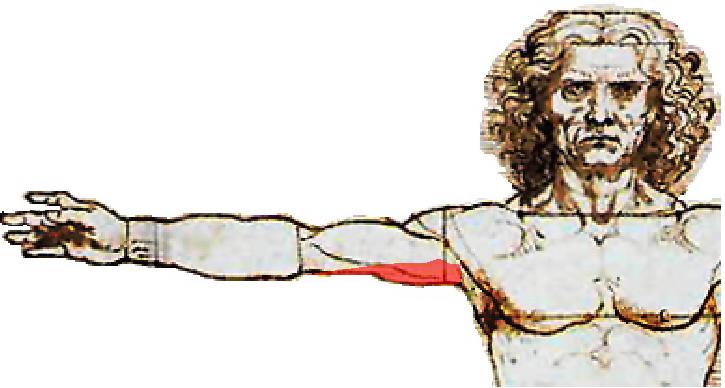
A branch course down inner aspect upper arm innervating this strip:
As seen here:
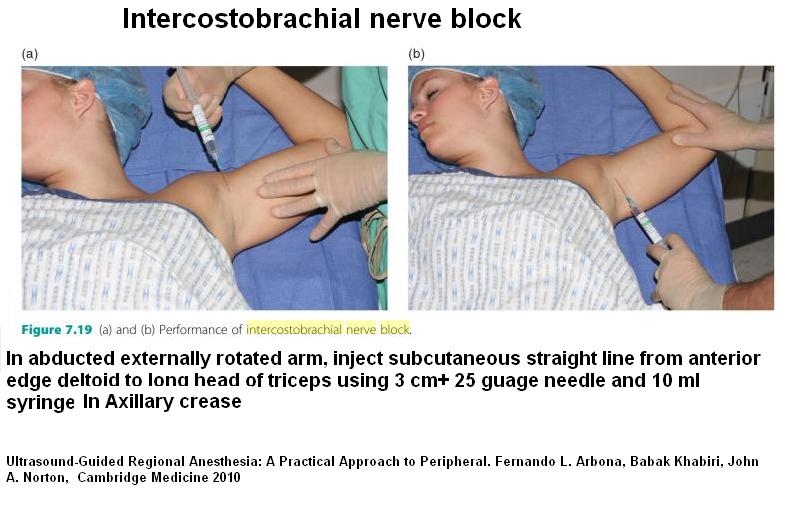
Blocking Nerve
Not a discrete block as multiple branches – instead injecting a subcutaneous strip front to back at bottom-most axilla:
- Evidence it has been sectioned can be confirmed by the paresthesia (funny feelings) and numbness in the proximal half posterointernal face of the upper arm.
- Studies have demonstrated that preserving this nerve during surgery might help prevent problems but authors are quick to add even in thier own cases this is not necessarily possible.
- Bruise formation in armpit “hematoma” can contribute to development post-mastectomy pains:
Pain Volume 108, Issue 3, April 2004, Pages 294–296
Some cases of severe post-mastectomy pain syndrome may be caused by an axillary haematoma
Cornelia Blunta, Angelika Schmiedel abstract here: - There seems little doubt that nerve damage “neuropathic pain” is involved in post breast cancer surgery pains:
Sensory function and pain in a population of patients treated for breast cancer
O. J. VILHOLM, S. COLDActa Anaesthesiologica Scandinavica Volume 53, Issue 6, pages 800–806, July 2009 abstract here
Syndrome of ICBN entrapment has been described:
- Severe pain involving in arm, shoulder, and chest
- “aching, or burning with intermittent flashes of bright, stabbing pain”
- Constant and more severe with arm movement
- pain radiates to the medial and posterior arm.
- excessive tenderness 2nd interspace anterior axillary line
- as described by
Atypical Chest Pain: Evidence of Intercostobrachial Nerve Sensitization in Complex Regional Pain Syndrome
Pain Physician 2009; 12:E329-E334 • ISSN 2150-1149
Jennifer W. Rasmussen, John R. Grothusen, Andrea L. Rosso, Robert J. Schwartzman free article here - Damage to this nerve has widely different expressions and it has been considererd that “Pain cannot be explained only by injury of the intercostobrachial nerve . An anatomical study of the extra-thoracic path of the intercostal nerve by Loukas et al. detected that the ICBN receives different contributions from the 1st, 2nd, 3rd, and 4th intercostal nerves. Based on those variations, the authors identified eight types of participation of those nerves in the formation of the intercostobrachial nerve . Perhaps those variations might explain the different complaints of pain by patients.”
as described in:
Post-Mastectomy Pain Syndrome. The Magnitude of the Problem
Tania Cursino de Menezes Couceiro, Telma Cursino de Menezes, Marcelo Moraes Valênça
Rev Bras Anestesiol 2009; 59: 3: 358-365 free article here
Neuromas:
- Neuromas are ascertained by
– very painful spot in scar
-tinel shooting numbness/pain when spot pressed on
– response to diagnostic injection - Neuromas are thought to be surgically treatable by surgical resection:
Annals of Plastic Surgery: May 2001 – Volume 46 – Issue 5 – pp 481-484
Intercostal Neuromas: A Treatable Cause of Postoperative Breast Surgery Pain
Wong, Lesley MD abstract here - At intercostal level, neuroma can be removed, nerves can be teased out of rib and planted in latissimus dorsi muscle:
Neurectomy for treatment of intercostal neuralgia.
Williams EH, et al
The Annals of Thoracic Surgery [2008, 85(5):1766-1770] abstract here
brought pain from 7-9/10 to 3.4/10 - Various injections are used on neuromas as well
For the intercostobrachial nerve damage cases various measures have been documented:
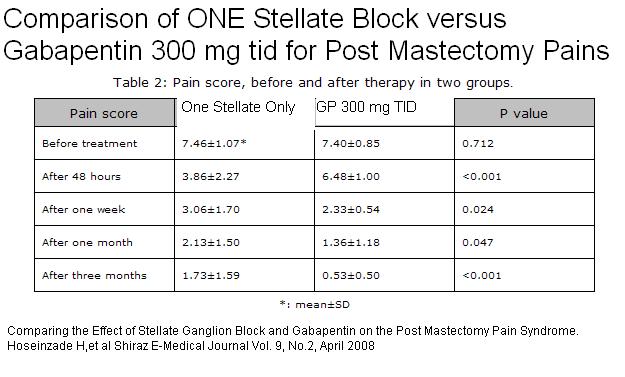
Comparing the Effect of Stellate Ganglion Block and Gabapentin on the Post Mastectomy Pain Syndrome.
Hoseinzade H, Mahmoodpoor A, Agamohammadi D, Sanaie S
Shiraz E-Medical Journal Vol. 9, No.2, April 2008 free article here
They mention:
1 Medications – antidepressants(18), NSAIDS (19), antiepileptics (20), opioids (21), NMDA receptor antagonists (22-23), lidocaine(24), magnesium (25), adenosine (26), ….)
Amitriptyline has been used for post mastectomy pains:
Kalso E, Tasmuth T, Neuvonen PJ.
Amitriptyline effectively relieves neuropathic pain following treatment of breast cancer.
Pain 1996;64:293–302
Gabapentin at 300 mg tid was found helpful in this article:
Comparing the Effect of Stellate Ganglion Block and Gabapentin on the Post Mastectomy Pain Syndrome.
Hoseinzade H, Mahmoodpoor A, Agamohammadi D, Sanaie S
Shiraz E-Medical Journal Vol. 9, No.2, April 2008 free article here
Results:
Gabapentin has been combined with Mexilitine for post mastectomy pains:
Fassoulaki A, Patrisk, Sarantopoulos C, Hogan Q.
The analgesic effect of gabapantine and mexiletine after breast surgery for cancer .
Anesth Analg 2002;95:985-91
2- Nerve blocks (28-30) –
stellate was used in this article:
Fluoroscopic Stellate Ganglion Block for Postmastectomy Pain: A Comparison of the Classic Anterior Approach and the Oblique Approach
Nabil Abbas, Dina MD; Abd el Ghafar, Ekramy M. MD; Ibrahim, Wael A. MD; Omran, Azza F. MD
Clinical Journal of Pain: March/April 2011 – Volume 27 – Issue 3 – p 207–213 abstract here
They did FOUR block and got good results
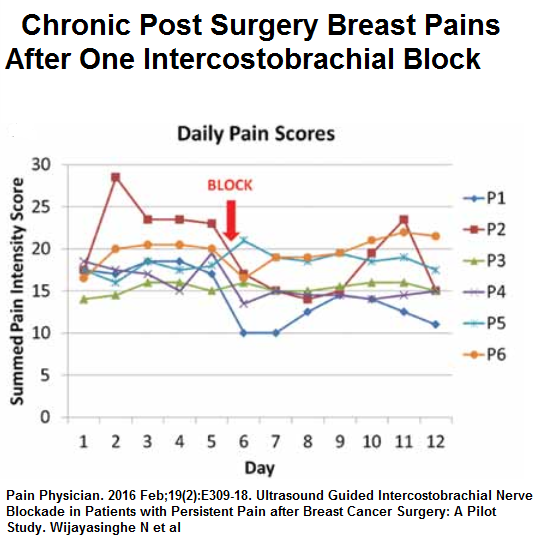
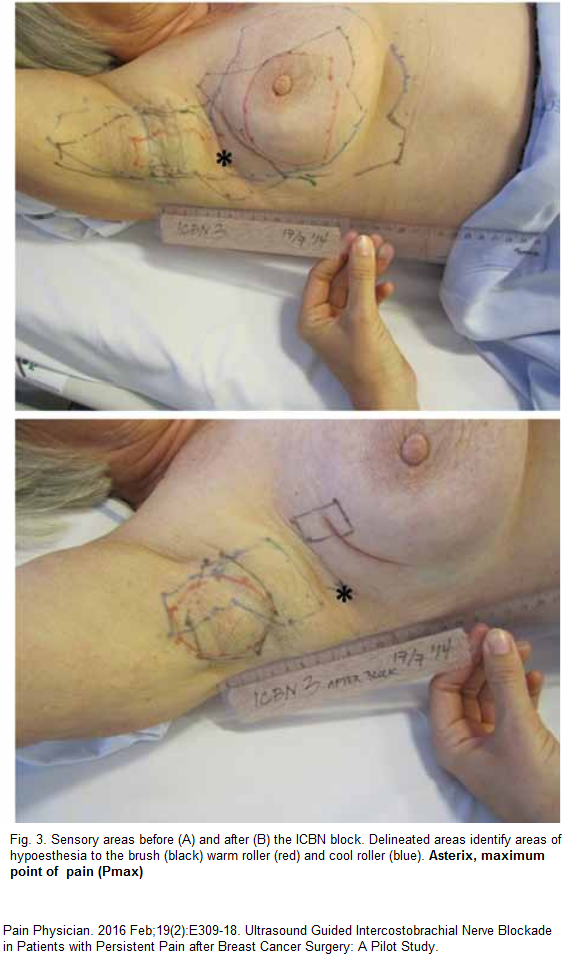
Recently an Ultrasound guided block of ICB nerve got some benefits though like other pains issues, repeated blocks are required to get much permanent results.
Pain Physician. 2016 Feb;19(2):E309-18.
Ultrasound Guided Intercostobrachial Nerve Blockade in Patients with Persistent
Pain after Breast Cancer Surgery: A Pilot Study.
Wijayasinghe N et al
http://www.painphysicianjournal.com/current/pdf?article=MjUyMg%3D%3D&journal=94
used Ten mL 0.5% bupivacaine given with 22 gauge block needle
persistent results were not well demonstrated “One week after the block was administered 2 patients demonstrated an improvement in their functional impairment scores (-17 and -29). However, 3 patients experienced a slight increase (13, 4, and 6) and one patient had no change.”
I use 5% lidocaine which has semi-neurolytic (mild nerve killing) properties – I gave a lady recently 0.5 mils into 2nd intercostal interspace laterally, 0.5 mls into point maximal tenderness, and rest into areas unaffected. She was much better week later and needed injection into posterior deltoid areas only.
Point maximal tenderness is:
3- peripheral nerve stimulation and spinal cord stimulation (27)
Why don’t surgeons deal with it?
- The don’t do nerve blocks;
- they don’t implant peripheral nerve stimulators;
- they have no training in physiotherapy techniques like myofascial release.
- Transferring groin lymph nodes to axilla helps some but unlike done here any time soon:
Post-mastectomy Neuropathic Pain Cure – Lymph Node Transplants - – The don’t implant neuroma nerves (suspect plastic surgeons can)
- – They don’t like treating chronic pain or using narcotics – heck, I’ve had patients with hip replacement sent home on Ibuprofen!
- They had very little training in chronic pain
I will try to expand on treatments sometimes
If you have good or bad experiences, I’d like to hear.
God help those who have mastectomies…
addendum:
Over 5-7 years after breast cancer surgery over 1/3 of women have persistent pain:
Evid Based Nurs. 2013 Aug 12. doi: 10.1136/eb-2013-101418. [Epub ahead of print]
Five to seven years after breast cancer treatment, over a third of women (37%) report persistent pain.
Knobf T.
no abstract
Comments – I use nerve damaging blocks of lidocaine 5% which like for shingles have to be given repeatedly: Scar injections might be needed to.
http://painmuse.org/?p=724
Addendum:
Part of the problem can result from fibrous cords that can develop in armpit that can occur particularly when axillary dissection or sentinel biopsying is done:
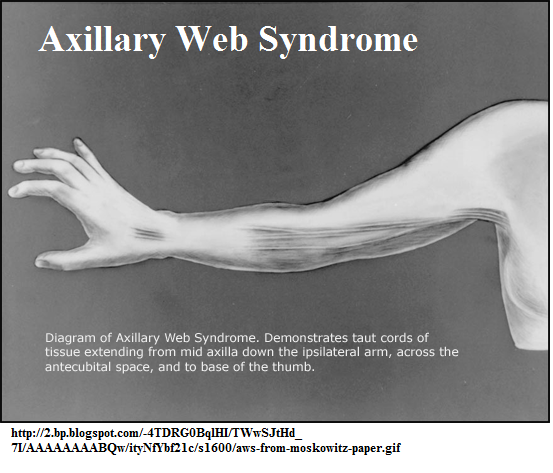
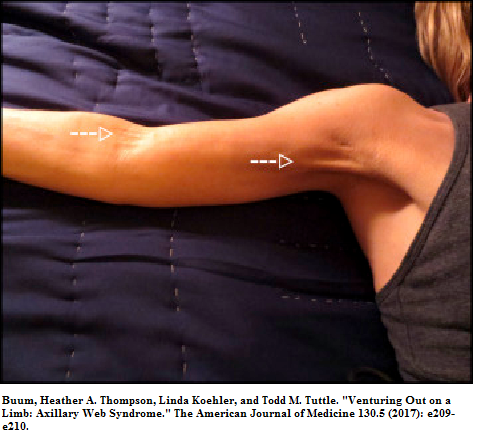
Recent article:
Buum, Heather A. Thompson, Linda Koehler, and Todd M. Tuttle.
Venturing Out on a Limb: Axillary Web Syndrome.
The American Journal of Medicine 130.5 (2017): e209-e210.
http://www.amjmed.com/article/S0002-9343(17)30006-2/pdf
- at 18 months suggested 50% incidence
- with axillary lymph node dissection 72%-75%
- with sentinel node biopsy 20%-41%
- syndrome is thought to be of lymphatic origin
- they suggest early aggressive physiotherapy
However a recent article suggested “cording” in 13.3%
Rev Bras Ginecol Obstet. 2017 Jul 12. doi: 10.1055/s-0037-1604181. [Epub ahead of
print]
Management of Axillary Web Syndrome after Breast Cancer: Evidence-Based Practice.
Luz CMD et al
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-72032017000300115&lng=pt&nrm=iso
- they found 1/2 resolved on own and 1/2 needed treatment but did not go into what exactly that entailed

OK….Upon doing google search about this Nerve Block my Plastic Surgeon suggest I came across this article that explained so VERY clear as to what I needed to know! THANK YOU!
Being 33 had a right masectomy for cancer in May 2013, reconstruction with removal of left breast June 2013, about 2 weeks after 2nd surgery the EXTREME burning, sharp shooting pain started under right breast. Ultrasounds done to make sure no infection, fluid build up anything. After any trips to dr and all I became very tired with my DR and ready to call quits with him BUT after reading this I am wondering if he may be right!?! He kept telling me we needed to “wait it out” and better pain mangement is needed. Being through chemo and all and so many hospital stays one gets tired of pain meds and dealing with depression after surgery I have learned they DO IN FACT contribute to my depression!!
The right breast I was very satisfied with after implant placed and all. Problems all started one day as I turned to walk out of bathroom door. All sudden EXTREME burning sharp shooting pain literally sent me to the floor! The shape of the breast changed and immed became swollen! Now this is the breast I had originally MX on and removal of lymph nodes. But why 2 weeks after surgery and all sudden? And pain and burning seems to get worse since it happened.
I am consulting the new DR for the nerve block in morning but have NOT agreed to doing it. Reading this article and few other things seems like might be a helpful thing!!!
—————-
Sounds like you have an implant shift complication – see article on breast reconstruction complications:
http://www.swancenteratlanta.com/wp-content/uploads/PlastReconSurg_2002_1097.pdf
The shift must have traumatized one of the intercostal or intercostobrachial nerves. Could also take a couple weeks to form a neuroma. You sure did not need this. A spot that triggers pain and any referred numbness would be nice… Working on an article about treatments for intercostal nerve pains mostly for post herpetic neuralgia but good for other things.
Good luck
admin
I am having intercostal brachial pain and I had my left breast removed 21 years ago. What to do . No one believes this.
————-
I would try massage first – and if there is arms swelling – get something called lymphedema massage. Pectoral, serratus and back shoulder muscles can play a part
Hi, Massages can be great therapy, helping to keep you stiffening up and adding to the chronic pain. Finding a specialist that not only believes you but has an understanding not only of what this pain is, but offering you options. I searched a very long time before I found a dr that has given me the Intercostal Nerve Block option. The benefits were nearly immediate! While I’m not positive this will be your answer,1st thing- don’t allow anyone to judge ur pain. Obviously, they don’t know what they’re talking about. Its not only real, its absolutely a COMMON problem! Hang in there, my survivor sister!!! B thinking of you and hoping u get some relief SOON! Please keep us posted!
Hi there, after putting up with axillary/anterior shoulder pain 2 years post mastectomy, I’ve now discovered why…and I know my body!! OK, I’m convinced I have PMPS and damaged nerves. No lymph nodes removed except for axillary clearance. Question; what is the Intercostal Nerve Block you mention? My doctor thinks I’m nuts saying my pain is from my surgery 2 years ago. Thanks for your article!!
I also have ths problem, and was told the PM ofc I have been to does not deal with Mast. Pain therapy because they do not understand it….i have dealt with it for 12 yrs…But recently confirmed that the pain near my sacrum is coming from a problem with the breast cavity and implants…..i emailed a dr via internet and this term was given as a possibility…i googled it and yes….it is
For those of us who are suffering with problems…is it allowable that others who have found drs who treat this, be able to mention their name?? It might help to have this info to get our own treatments going.
But to be honest…i have tried it all in 12 yrs for the secondary problems it brought on..nothing helps…I had some wonderful promise before with PT to only find myself even more alone then before searching for help…..my marriage has fallen apart, my children grown and I have nothing left….
I had surgery for strong family history because the drs played on my fear …The worst thing I ever did……i should have taken my chances…
Hi. I had fibro adenomas and my breast were removed. I had a lot of pain before and after the mastectomy. My Dr put silicone immediately in after the mastectomy. Nobody believe me about the pain I had in my right breast after the mastectomy. My right arm was constantly burning and have stitching pains. Could!d not use my arm. My GP called it awkward pains. Nobody could!d help me. They send me to a cosmetic surgeon and even him could not understand the pain I have. After 3years he decided to remove the silicon and all breast tissue and complete mastectomy. I need to get expanders afterwards to stretch the skin. Pain was still unbearable. The surgeon could not believe it. After my reconstruction the pain was still unbearable. They send me to a pain clinic. The 1st time a Dr understood the pain I have with the mastectomies the injured my nerves along the side of my breast under the armpit. They implanted a spinal cord stimulator and thank God my pain is better. I hope this will help you and others with same problems. Good luck
Hello,
I had my Mastectomy July 2013 where they also removed 3 nodes. I have always had some tenderness but the last few months it has gotten from tenderness to pain with lots of tingling and weakness. My Oncologist says I need to talk to my GP. Made an appt with my GP he wants a Nerve stimulation test and an MRI come to find out I have to wait til July of this year to even get seen. Guess I have to live with this pain til then.
To top things off since I had Chemo I have had more health issues then ever before, such as teeth just falling disintegrating, severe cellulitis where I was kept in the hospital for a week then there are the headaches, the list goes on and on but the Drs just tell me remember we are not getting any younger, take an ibuprofen that should help. Just love that remark.
Thank you for your article, was wondering do I need to get permission to print it so that I may hand it to my Dr?
—————
Delores,
I’m glad you found it useful. I made these blog notes so you could have something to take to your Doctor. Maybe make sure your B12 is normal (maybe have him check) and remember to take vitamin C 500 mg 2x/day – helps prevent CRPS pains and helps immunity.
Don’t forget vit D helps pain at 4000u/day
http://painmuse.org/?p=4168
and helps prevent breast cancer recurrence:
http://health.ucsd.edu/news/releases/Pages/2014-03-06-vitamin-D-and-breast-cancer-survival.aspx
and melatonin helps reduce breast cancer recurrence and augments tamoxifen:
http://www.sciencedaily.com/releases/2014/01/140128103117.htm
http://www.sciencedaily.com/releases/2014/07/140725080408.htm
Good luck
admin
Pingback: Any Neurologists here on BBC?
Pingback: PMPS: Post Mastectomy Pain Syndrome | AlteaYoga
Not a day goes by that I don’t have pain my double mastectomy was on 5/5/14 my PS removed my spacer and implant in August 2014 those sharp stabbing pain had a MRI nothing was found only scar tissue. Thank u for your article. Will copy show to my PCP
I had a mastectomy 2010. Have been taking morphine and oxy since abojt 6 months post op for pain. Had 29 lymphnodes removed, major pectoal muscle, and a lot of tissue. Skin was down to rib cage. I have tried Lyrica, Gagapentin, to no avail. I also suffer from lyphadema if I am not careful. I have had cellulitis three times. Last year I was told by a plastic surgeon if i had reconstruction done with a dorsi flap this could potentially help my chronic pain. It did not. Just added to it. Since my cancer and chronic pain I have developed depression and srruggle with bipolar. I am on disability and struggle with self. We just recently moved to another state and now my pain meds have been taken away cold turkey. Doctors here don’t understand… I am having to take withdrawal medication. Makes me feel worse and insurance only wants to cover it a short while. Guess my question is what pain block meds are working and how ften because I am still in pain… Thank you…
I have been having chronic and severe itching from the radiation on my chest wall (under breast) from 2009. Went to radiologist yesterday & he said it was probably nerve damage from the radiation. I also have 3 fractured ribs from it that he said will never heal b/c the ribs are damaged now from radiation. Has anyone else experienced any of this?
————————-
Nerve damage can cause itch and there is a syndrome of itch between shoulder blades caused by nerve damage there – called Noctalgia paresthetica. I wrote about it:
http://painmuse.org/?p=335
Treatments would be same:
– injections
– Capsaicin (red pepper) topically (like Zostrix) 3-4 times daily – best if lidocaine is added because application burns and a cortisone cream used regularly to keep down the irritation it can cause.
– Botox injections subcut along tender itch nerves
I knock out pain of damaged ribs with injections of semineuolytic local anesthetic just below ribs – 5% lidocaine (2 mls max each injection) or 4% pontocaine/tetracaine. I described its use in post herpetic neuralgia here:
described below but it can numb rib fracture pain from several days to several weeks+ at a time – with more prolonged results with a series of three.
Alternate Approaches to Post-Herpetic Neuralgia (PHN) .
http://painmuse.org/?p=346
admin
I wonder if you can send me some doctors names in the DC MD VA area that might understand more about the protocols you mention here. I have pretty much textbook pain from BC treatments. PMPS. But I have also had tingling and burning in my chest when I overuse my arm – and I begin to cough which is just a reactive cough.I have had this for 2 years. This symptom seems to throw everyone off. I went to a pain doc I really like who says I have complex regional pain syndrome – wants to do ganglion block. I am leery of getting this and really would like the more focused approaches in this article. I need to send this article to him but also wanted to know if you knew any pain docs in my region that I may not have to “educate” about this. I realize the injections may not help and perhaps a ganglion block can – but I do not like the side effects of that block and would like to try a more focused approach first. Thanks for this great article – I know this has helped many people find relief. Thank you- Anne S
Thanks, this website is extremely helpful
Wonderful information and images
I send you this link about it (longtime outcome with gabapentin)
https://www.ncbi.nlm.nih.gov/pubmed/26961424?dopt=Abstract
Thank you
I appreciated your graphics and would like to use one with permission. I am an IBCLC and am creating a course for nurses re: breastfeeding.
http://painmuse.org/wp-content/uploads/icbn1.jpg
Thank you
————————-
none of the graphics are mine; at bottom I do credit the real author
– admin
Right after double mastectomies ,I had severe pain. My surgeon said he never heard of the type of pain I was experiencing. It was like a steel band was squeezing my chest. I was later diagnosed with nerve damage and given Lyrica. It helped pain somewhat but side effects ex memory loss were too severe. I had them lower dose so I am still on Lyrica but low dose. Pain now 3 years post surgery is manageable but still there. Wish I could send that surgeon your notes but I have moved on.
If I am having large scar tissue massaged by lymphodema specialist can the spreading scar tissue (have a lot of scar tissue) affect the nerves or bump into them? I have started having sharp shooting pains since starting the therapy. I don’t recall them happening before they started working on it.
Pingback: Post Breast Surgery Pain – Clearer Reason It’s Bad – High Prevalence of Neuropathic Pain | Pain Medical Musing
I had a double mastectomy in 2006. The sloppy surgeon cut the intercoastal brachial nerve and I had screaming pain for 4 months. I tried everything from nerve blocks to heavy drugs and nothing helped. My husband (a podiatrist) came up with1/2 tramadol and 100 mg gabapenten. I can nowfunction through life.