If you take cases of cervical radiculitis – if imaging shows possible reason for it, they give a history of having had shingles at about 18.4%. In cases with normal imaging, the prior incidence jumps to 81.6% (p<0.01) – most of them not within the last 24 months. This leaves one to wonder if the virus had some input into this disease or whether abnormal autoantibodies contributes to some autoimmune syndrome.
Int Orthop. 2017 Aug 10. doi: 10.1007/s00264-017-3593-0. [Epub ahead of print]
Shoulder pain due to cervical radiculopathy: an underestimated long-term
complication of herpes zoster virus reactivation?
Gumina S et al
https://www.ncbi.nlm.nih.gov/pubmed/28798978
- 110 cases aged 40-73 (average 46.5) M 52; F 58
Symptoms – Symptoms in 2 studies:
- paraesthesias in 89.7 – 91%
- sensory loss in 24% – 33%
- symptoms of weakness in 15.3 – 34%
- signs of weakness in 64.2 – 70%
- hypoactive tendon reflex – 72% – 84.1%,
- C7 is the most affected , followed by C6, C5, C4 and C8
18.4%; in mri positive group history shingles
81.6% in mri negative group history shingles – mostly over 2 years ago
Comment – question of whether course of anti-virals should be tried in cervical radiculitis of unknown cause. There is a syndrome of Parsonage–Turner Syndrome:
Feinberg, Joseph H., David A. Doward, and Alita Gonsalves.
Cervical radiculopathy vs Parsonage–Turner syndrome: a case report.
HSS Journal 3.1 (2007): 106-111.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2504088/
their summation verbatim:
- Patients present with sudden and severe shoulder girdle pain. Pain can also involve the trapezius ridge, arm, forearm, and hand [5]. The symptoms often appear to be radicular-like but many of its hallmark features are atypical for a cervical radiculopathy.
- Pain is rarely positional, Spurling’s maneuver is usually negative, and sensory changes are not in a dermatomal fashion.
- Pain lasts from hours to weeks and then gradually subsides but it is not always the predominating feature [29, 34, 38].
- Rapid and severe atrophy follows weakness approximately 3–4 weeks after the initial onset of symptoms. As the pain subsides, 75% of patients are left with severe weakness in muscles innervated by the upper trunk of the brachial plexus [29, 38].
- There is full motor recovery in approximately 36% of patients at 1 year, 75% of patients at 2 years, and in 89% of patients at 3 years [38].
- Sensory changes are often not a significant complaint or finding [43] but sensory deficits were observed in 66% of patients in one study [6] and in a minority of patients in another [43].
- Parsonage–Turner syndrome primarily affects the upper trunk of the brachial plexus or one of the shoulder girdle’s peripheral nerves, although rare involvement of the middle and lower trunks has also been reported [38].
- The suprascapular, long thoracic, and axillary nerves are the most commonly involved peripheral nerves [21, 27, 30, 38]. The musculocutaneous, anterior interosseous, ulnar, median, and phrenic nerves were also reported [6, 19, 23, 28].
- There are also reports of lumbosacral plexus involvement but most of these patients have complicated medical histories, suggesting there may be other contributing factors [4, 12, 23, 33]. Because the paraspinal muscles are usually spared, root level involvement is felt to be rare [23].
- Gender differences exist in Parsonage–Turner syndrome. There is a higher incidence in men than women. Magee and DeJong [21] reported a male to female ratio of 11.5 to 1, Tsaires et al. [38] a ratio of 2 to 1, and Parsonage and Turner [29] a ratio of 2 to 1. But Martin and Kraft [24] found a much closer ratio of 11 to 9.
- Etiology of the disorder is disputed, with 25% occurring after viral infection and 15% after immunization [14].
- Other risk factors include patients who have had injury at a remote area, at postexercise, and at postsurgical [14, 24, 43].
- Thirty-three percent of cases have bilateral involvement, but one side may be subclinical and only detected by evidence of axonal degeneration on EMG.
- The clinical course is usually self-limiting, and strength gradually returns, but this may be incomplete [35].
- Treatment is symptomatic with nonsteroidal anti-inflammatory drugs, narcotics, anticonvalescents, and physical therapy [22, 27]. Steroids and antiviral medication were used but there is no consensus whether these medications are indicated [24]. The early use of steroids when they are given has a more favorable prognosis. Other causes of brachial plexopathy should be considered, such as stretch injury, cancer, postradiation, and idiopathy. There is also a hereditary form of brachial neuritis [37].
Comment – saw a case of Parsonage–Turner syndrome in which pain over triceps area was severe. Neck movements would not precipitate it. Frequent B12 injections were a help as per:
Chronic Back Pain Help – Forgotten B12 Injections and What Else Good For…
http://painmuse.org/?p=1543
addendum:
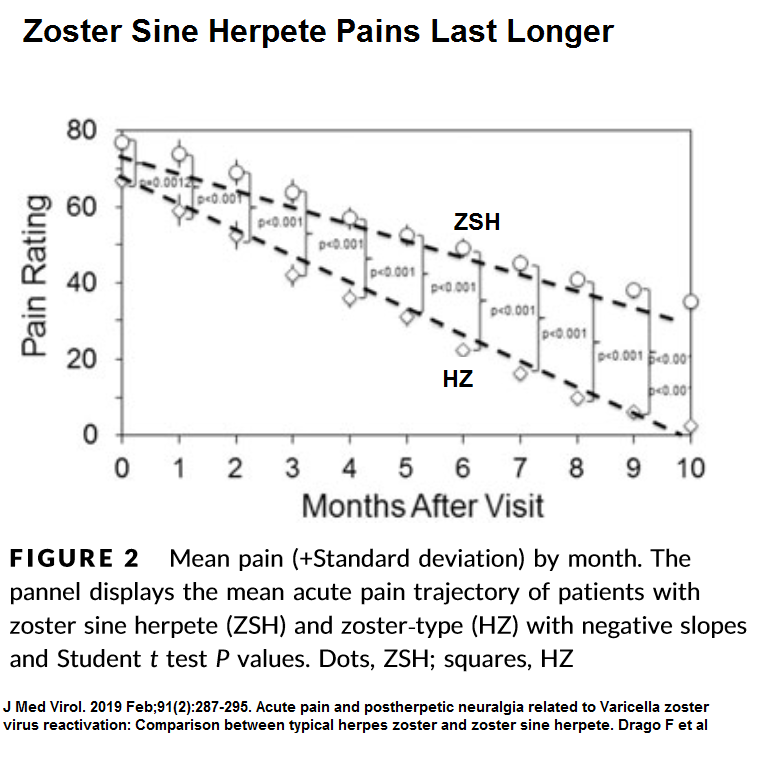
what is not known, is that zoster sine herpete (shingles without rash) is more painful and lasts longer that that with rash
J Med Virol. 2019 Feb;91(2):287-295. doi: 10.1002/jmv.25304.
Acute pain and postherpetic neuralgia related to Varicella zoster virus
reactivation: Comparison between typical herpes zoster and zoster sine herpete.
Drago F et al
- confirmed by Serum samples – initial visit and 1 and 2 months later.
- “VZV DNA persisted statistically higher in ZSH sera than HZ sera 1 month after onset (P = 0.0007)”
- pain was higher VAS – 76.88/100 vs. 66.88 ( P = 0.0012)
I give steroid injections into zoster rash areas but not sure what to do if no rash. I also give nerve blocks to tenderized areas – not sure what to do with the no rash as well.
Just one tip re injecting tenderized areas in herpes zoster – there is a whole zone near the midline of the back from the back dorsal nerve roots. -higher up levels have the roots come out near the spinous process and can be hit there – otherwise further out.
Comment – I have 3 cases of neck and arm pain radiculitis without injury that I have treated successfully with Valcyclovir 1000 mg tid x7 days with surprisingly good results – all caught within days of it getting bad – some advantage to doing GP work