Finding Mast Cell accumulations up to 15 times normal in the skin of Fibromyalgia (FM) subjects has raised the question whether FM is a skin condition causing a tenderness there. This has sparked my interest in dermatological treatments. A trial of UV treatments didn’t show much.
The concept of FM being a mast cell disease was discussed here:
Is Fibromyalgia a Mast Cell Disease – like some “somatization diseases” such as migraine, TMJ, irritable bowel, and interstitial cystitis
Re Suntanning:
g and FM:J Altern Complement Med. 2009 Jan;15(1):15-23.
Pilot study of the effect of ultraviolet light on pain and mood in fibromyalgia syndrome.
Taylor SL, Kaur M, LoSicco K, Willard J, Camacho F, O’Rourke KS, Feldman SR. abstract here
- Blinded, controlled trial using both UV tanning and non-UV tanning beds
- White women ages 29-58
- Some exclusions:
- Fitzpatrick skin type 1 (“never tan, always burn”);
- past or present skin cancer;
- On sun sensitizing drugs – I would think that would lessen the dose of sun exposure needed
- pregnant, planning to become pregnant, or breast feeding – I would think that would make it a more natural treatment
- photosensitive disease, positive antinuclear antibody, positive anti-Smith antibody test, or positive anti-ds-DNA test
- UVB irradiance of 0.40 mW/cm2 and UVA irradiance of 13.73 mW/cm2
- looks like 8 weeks of monday, wednesday and friday – 24 total sessions
- UV exposure was increased from 3 min to 9 min over the first 6 visits. Then 10 min. – a session thereafter
- Results on pain levels:
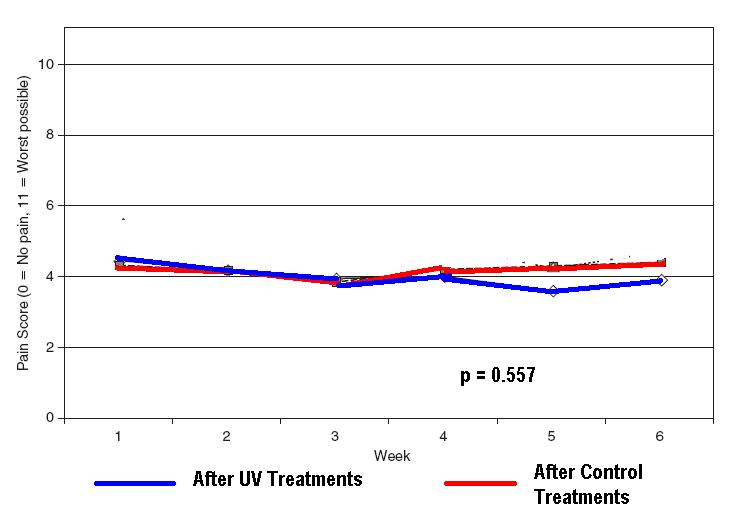
Pain level differences between the two were neither statistically nor clinically (need a drop of 2) significant.
- The hope in this study was that endophins (bodies natural morphine) would be stimulated by UV treatment.
- A recent article found UV skin stimulation promoted the production not only of Vitamin D3 but also interleukin-10, which suppresses inflammation:
J Exp Med. 2010 Mar 15;207(3):455-63. Epub 2010 Mar 1.
Evidence that vitamin D(3) promotes mast cell-dependent reduction of chronic UVB-induced skin pathology in mice.
Biggs L, Yu C, Fedoric B, Lopez AF, Galli SJ, Grimbaldeston MA. abstract here
“Our findings suggest that 1alpha,25(OH)(2)D(3)/VDR-dependent induction of IL-10 production by cutaneous mast cells can contribute to the mast cell’s ability to suppress inflammation and skin pathology at sites of chronic UVB irradiation.” - One wonders if UV treatments would only be successful preventatively. It has been recently found that high vitamin D levels might prevent the later induction of MS.
JAMA. 2006 Dec 20;296(23):2832-8.
Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis.
Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. free article here
“Only the OR for the highest quintile, corresponding to 25-hydroxyvitamin D levels higher than 99.1 nmol/L, was significantly different from 1.00 (OR, 0.38; 95% confidence interval, 0.19-0.75; P = .006).”
Now in the animal model it has been found that UV exposure itself lower risk of the animal model of MS above its vitamin D effects:
Proc Natl Acad Sci U S A. 2010 Apr 6;107(14):6418-23. Epub 2010 Mar 22.
UV radiation suppresses experimental autoimmune encephalomyelitis independent of vitamin D production.
Becklund BR, Severson KS, Vang SV, DeLuca HF. abstract here
Comments – This is a big disappointment and would suggest FM is much more than just a skin disease. Study is however fraught with “subgroup” problems:
It has been suggested that there are 3 group of FM patients – those with tender spots, those with tender muscle triggers, and those with a combination of the two:
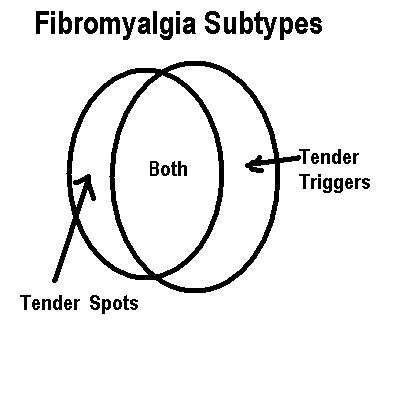
I would think it unlikely that the tender triggers would respond to suntanning as the muscles are not skin deep. However, the subtype with just tender spots might be more a skin issue and more likely to respond.
Having said that, it seems unlikely that UV irradiation in itself would show benefit. It may be that it would only be valuable in combination with other treatments that would alter mast cell expression and deal with the central sensitization and peripheral muscle sensitization seen in FM.
I would be interested in any other perspectives.
