Sorry – trying to change fonts has duplicated some areas…
It is become increasingly clear that so-called “somatization” “psychosomatic” diseases are associated with abnormal concentrations of mast cells – guardians of peripheral sensitization and also carriers of allergy reactions such as hives. Now Fibromyaglia has been found to be associated with excessive mast cell accumulations. One wonders if a skin biopsy could be used in the future to diagnose Fibromyalgia. There can be a problem finding mast cells because of a bad tendency to understain specimens.
Clin Rheumatol. 2010 Apr 30. [Epub ahead of print]
Abnormal overexpression of mastocytes in skin biopsies of fibromyalgia patients.
Blanco I, Béritze N, Argüelles M, Cárcaba V, Fernández F, Janciauskiene S, Oikonomopoulou K, de Serres FJ, Fernández-Bustillo E, Hollenberg MD. abstract here
- Biopsies found 5-15 mast cells per high powered field vs 0-1 in “normal” people – that is 5 -15 times the number of cells in the skin.
- Their conclusion – Fibromyalgia is a Mast Cell (MC) disease. This high body load of mast cells could degranulate at any time “releasing several proinflammatory products which are able to generate nervous peripheral stimuli causing CNS hypersensitivity, local, and systemic symptoms.”
Confirming that excessive skin mast cells are implicated in this disease comes from another skin mast cell disease – chronic hives – ie chronic uriticaria:
Acta Derm Venereol. 2009;89(4):389-92.
Chronic urticaria is usually associated with fibromyalgia syndrome.
Torresani C, Bellafiore S, De Panfilis G. abstract here free article here
- 70% – Yes, seventy percent – of these cases had Fibromyalgia.
- Their reason? – Neurogenic skin inflammation – “It is possible that dysfunctional cutaneous nerve fibres of patients with fibromyalgia syndrome may release neuropeptides, which, in turn, may induce dermal microvessel dilatation and plasma extravasation. Furthermore, some neuropeptides may favour mast cell degranulation, which stimulates nerve endings, thus providing positive feedback.” – chemicals released by allergy cells irritate the nerve (we know that because itch is a nerve C fiber type of pain) which sets up a peripheral sensitization which then triggers a central sensitization.
______________
Preliminary discussion:
Mast Cells do triple duty – allergy reaction, host defense, and initiate peripheral sensitization
- Mast cells are typical mediators of allergic reactions. Interestingly, they are attracted by damaged nerves and play a role in “peripheral sensitization” where nerve-damaged tissues are rendered inordinately painful, swollen and spastic . They are also important in certain “host defense:
- Curr Opin Immunol. 2007 Feb;19(1):31-8. Epub 2006 Nov 28.
New and emerging roles for mast cells in host defence.
Dawicki W, Marshall JS. abstract here
So call Somatization Disorders may well be Mast Cell Diseases
Somatization disease (diseases without known cause – previously thought more psychosomatic) have been found to have associations with mast cells:
INTERSTITAL CYSTITIS

- Interstitial cystitis – bladders in IC are crawling with mast cells:
- The Mast Cell in Interstitial Cystitis: Role in Pathophysiology and Pathogenesis
Grannum R. Sant, Duraisamy Kempuraj, James E. Marchand, and Theoharis C. Theoharides
UROLOGY 69 (Suppl 4A): 34–40, 2007 free article here -
mast cell counts >20 cells/mm2 in bladder muscle have an 88% diagnostic specificity and a 95% diagnostic sensitivity for IC. -and most of them are degranualated – “spent” from overactivity.
Drugs used for allergies have been found to help IC:
-
- Singulair 10 mg daily (though I have used it twice daily) – after 3 months – “urinary frequency had decreased from 17.4 to 12 voidings (p = 0.009), nocturia had decreased from 4.5 to 2.8 (p = 0.019) and pain had decreased from 46.8 to 19.6 mm”:
- IN: J Urol. 2010 Aug 17. [Epub ahead of print]
Interstitial Cystitis/Painful Bladder Syndrome and Associated Medical Conditions
With an Emphasis on Irritable Bowel Syndrome, Fibromyalgia and Chronic Fatigue
Syndrome.
Nickel JC, Tripp DA, Pontari M, Moldwin R, Mayer R, Carr LK, Doggweiler R, Yang
CC, Mishra N, Nordling J. abstract – here- Hydroxyzine: an antihistamine helps – start 25 mg hs 1st week, 50 mg hs second week, then 50 mg bed and 25 mg mid-day resulted in a 40% symptom reduction.
Urology Volume 49, Issue 5, Supplement 1, Pages 108-110 (May 1997)
Hydroxyzine therapy for interstitial cystitis
Theoharis C. Theoharides, Grannum R. Sant
- Hydroxyzine: an antihistamine helps – start 25 mg hs 1st week, 50 mg hs second week, then 50 mg bed and 25 mg mid-day resulted in a 40% symptom reduction.
Maybe chronic prostatitis too?? – there is some rodent evidence that this can occur but understaining in the human model may be underestimating this…
Migraines – mast cell activity helps initiate problems in migraines:
Mast cell degranulation activates a pain pathway underlying migraine headache
D Levy, R Burstein, V Kainz, M Jakubowski, AM
Pain. 2007 July; 130(1-2): 166–176. free article here
The role of mast cells in migraine pathophysiology
Theoharis C. Theoharides, , Jill Donelan, Kristiana Kandere-Grzybowska1 and Aphrodite Konstantinidou2
Brain Research Reviews 49(1), July 2005, Pages 65-76 abstract here
- Stress effects migraine levels – No big surprise – stress helps initiate the mast cell activation to degranulate:
Endocrinology. 1995 Dec;136(12):5745-50.
Stress-induced intracranial mast cell degranulation: a corticotropin-releasing hormone-mediated effect.
Theoharides TC, Spanos C, Pang X, Alferes L, Ligris K, Letourneau R, Rozniecki
JJ, Webster E, Chrousos GP. abstract here
Interestingly, part of the damage mast cells might inflict may be through the renin-angiotensin blood pressure system:
Mast Cells Activate the Renin Angiotensin System and Contribute to Migraine: A Hypothesis
Hisham Ba’albaki, MD; Alan Rapoport, MD
Headache 48 (10),2008 pp. 1499-1505
-
- which might explain why ACE (angiotension converting enzyme) inhibitor may help migraines:
lisinopril (10 mg first week, then 20 mg) – 20% reduction over placebo
BMJ. 2001 January 6; 322(7277): 1-4
Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study
Harald Schrader free article here
- And why ARB’s (angiotension receptor blockers) might help:
Candesartan (atacand)16 mg OD – 31% reduction headache hours over placebo
Tronvik E, Stovner LJ, Helde G, Sand T, Bovim G. Prophylactic treatment
of migraine with angiotensin II receptor blocker. JAMA 2003;289:
65-9. free article here
- And why ARB’s (angiotension receptor blockers) might help:
- which might explain why ACE (angiotension converting enzyme) inhibitor may help migraines:
Blockers of this system help migraines:
Ann Pharmacother. 2010 Feb;44(2):360-6. Epub 2010 Jan 19.
Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers for
the prevention of migraines.
Gales BJ, Bailey EK, Reed AN, Gales MA. abstract here
TMJ
- TMJ – increased mast cells have been implicated in this disorder:
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Oct;92(4):384-9.
Substance P and mast cells: preliminary histologic analysis of the human temporomandibular joint.
Henry CH, Wolford LM. abstract here
the association of mast cells and and substance P containing nerves gives it some credibility. -
A previous study had noted mast cells in TMJ discs of TMJ dysfunctional subjects:
Arch Oral Biol. 1995 Jun;40(6):549-57.
A microscopic and immunocytochemical study of structural changes in dysfunctional
human temporomandibular joint discs
Marchetti C, Piacentini C, Farina A, Bernasconi G, Calligaro A. abstract here
Cytokines are elevated in TMJ syndrome:
British Journal of Oral and Maxillofacial Surgery Volume 41, Issue 2, April 2003, Pages 95-101
Expression of interleukin 6 in synovial tissues in patients with internal derangement of the temporomandibular joint
- Irritable bowel syndrome: although there have been sporadic reports demonstrating increased mast cells in Irritable bowel for years, no one actually put two and two together until this landmark study was published in 2004:
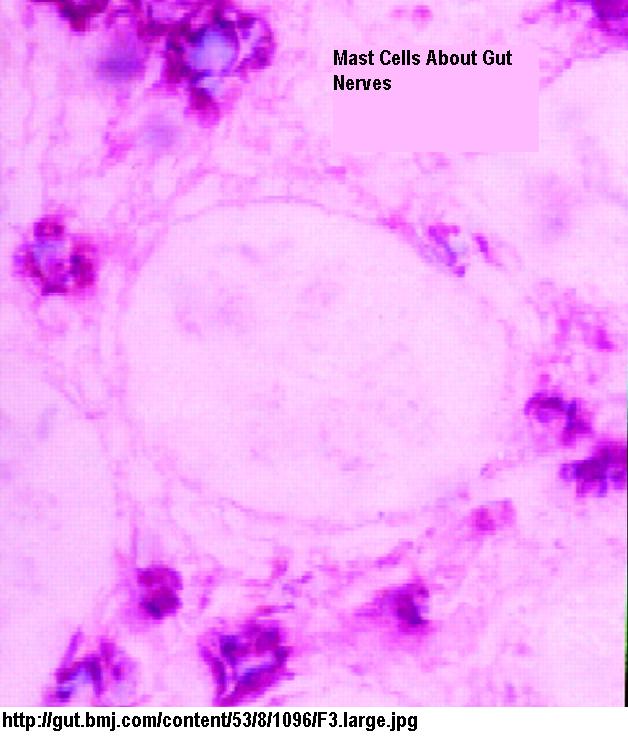
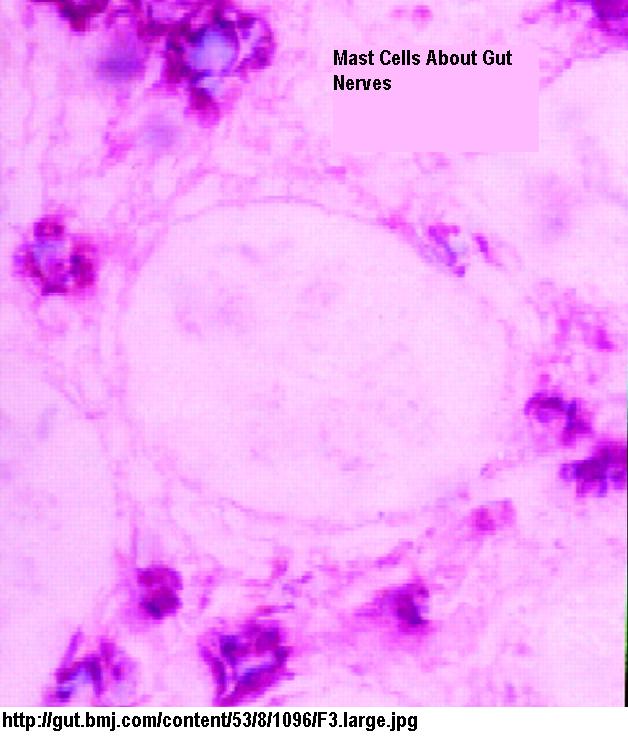
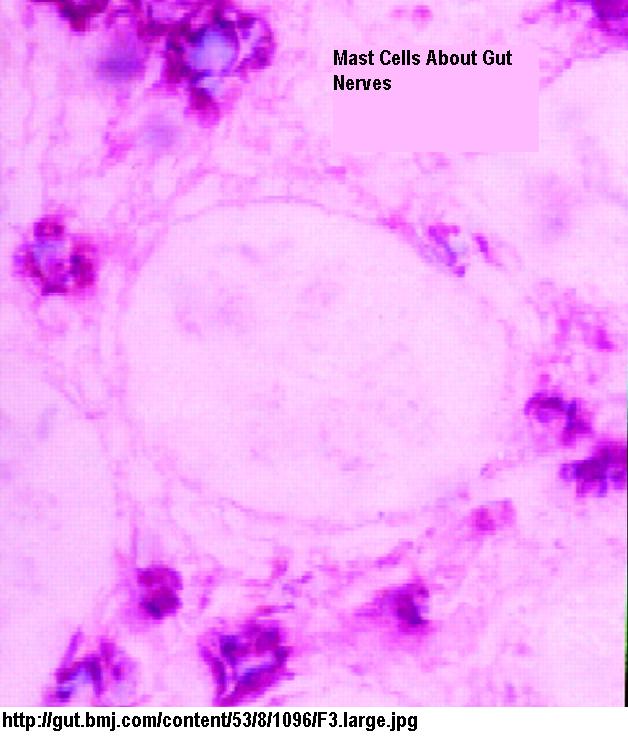
Activated Mast Cells in Proximity to Colonic Nerves Correlate With Abdominal Pain in Irritable Bowel Syndrome
GIOVANNI BARBARA,* VINCENZO STANGHELLINI,* ROBERTO DE GIORGIO,* CESARE CREMON,* GRAEME S. COTTRELL,‡ DONATELLA SANTINI,§ GIANANDREA PASQUINELLI,§
ANTONIO M. MORSELLI–LABATE,* EILEEN F. GRADY,‡ NIGEL W. BUNNETT,‡ STEPHEN M. COLLINS, and ROBERTO CORINALDESI*
GASTROENTEROLOGY 2004;126:693–702 free article her
- Prior gut trauma (previous infection), food allergy, and stress are key players in this mast cell contributing pain syndrome:
Mast cells: A possible link between psychological stress, food allergy,nd gut hypersensitivity in the Irritable Bowel syndrome
XIAN-YONG GUI
Journal of Gastroenterology and Hepatology Volume 13 Issue 10, Pages 980 – 989
abstract here- There is evidence of activation of the immune system in Irritable bowel, in part probably mediated by mast cells:
Immune Activation in Patients With Irritable Bowel Syndrome
TOBIAS LIEBREGTS,*,‡ BIRGIT ADAM,*,‡ CHRISTOPH BREDACK,*,‡ ALEXANDER RÖTH,§ SUSANNE HEINZEL,SUE LESTER, SARAH DOWNIE–DOYLE, ERIC SMITH, PAUL DREW,NICHOLAS J. TALLEY,#,** and GERALD HOLTMANN*,‡
GASTROENTEROLOGY 2007;132:913–920 free article hereThe plot thickens with finding this inflammation associated with a leaky gut that can spawn further
-
- reaction:
-
- see
Irritable Bowel (IBS) Involves Excessive Permeability of Gut MembranesPart of the visceral hypersensitivity in IBS might be mediated by the fact that mast cells can cause persistent activation of “C” nerve fibers – in skin these fibers are associated with burning pain peripheral sensitization
-
- .
Mast cell-mediated long-lasting increases in excitability of vagal C fibers in guinea pig esophagus
Shaoyong Yu,1 Marian Kollarik,2 Ann Ouyang,1 Allen C. Myers,2 and Bradley J. Undem2
Am J Physiol Gastrointest Liver Physiol 293: G850-G856, 2007 abstract hereThe visceral hypersensitivity level, particularly in the diarrhea dominant Irritable bowel
- , correlates well with mast cell counts in the in the terminal ileum, ascending colon and rectum:
Journal of Gastroenterology and Hepatology Volume 21 Issue 1, Pages 71 – 78
Mucosal mast cell counts correlate with visceral hypersensitivity in patients with diarrhea predominant irritable bowel syndrome
JUNG HO PARK, POONG-LYUL RHEE, HYUN SEO KIM, JUN HAENG LEE, YOUNG-HO KIM, JAE JUN KIM AND JONG CHUL RHEE abstract hereSo mast cells do double duty – help mediated peripheral sensitization and run allergic reactions.
Surveys have demonstrated people with IBS have intolerances to about 1/3 of foods. Dietary changes have an impact on IBS:
Is there a role of food allergy in irritable bowel syndrome and functional dyspepsia? A systematic review
M.I. Park & M. Camilleri
Neurogastroenterology & Motility Volume 18 Issue 8, Pages 595 – 607, 22 Dec 2005
abstract hereElimination diet is associated with improvement in 1/2 of cases (and if bacterial overgrowth
- had been dealt with, I bet that could have been even higher):
EPIDEMIOLOGIC ASSOCIATION OF ABOVE DISEASES:
The above mentioned diseases are all interconnected:Re Fibromyalgia – stats from:
J Clin Rheumatol. 2006 Jun;12(3):124-8.
The incidence of fibromyalgia and its associated comorbidities: a population-based retrospective cohort study based on International Classification of Diseases, 9th Revision codes.
Weir PT, Harlan GA, Nkoy FL, Jones SS, Hegmann KT, Gren LH, Lyon JL. abstract here
Food intolerance and the irritable bowel syndrome
R NANDA, R JAMES, H SMITH, C R K DUDLEY, AND D P JEWELL
Glut, 1989, 30, 1099-1104 free article here
- dairy and wheat products were highest on list (so much for eating bran – use psillium instead)
D Levy, R Burstein, V Kainz, M Jakubowski, AM
Pain. 2007 July; 130(1-2): 166–176. free article hereInterestingly, part of the damage mast cells might inflict may be through the renin-angiotensin blood pressure system:
Mast Cells Activate the Renin Angiotensin System and Contribute to Migraine: A Hypothesis
Hisham Ba’albaki, MD; Alan Rapoport, MD
Headache 48 (10),2008 pp. 1499-1505Blockers of this system help migraines:
Ann Pharmacother. 2010 Feb;44(2):360-6. Epub 2010 Jan 19.
Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers for
the prevention of migraines.
Gales BJ, Bailey EK, Reed AN, Gales MA. abstract here
- which might explain why ACE (angiotension converting enzyme) inhibitor may help migraines:
lisinopril (10 mg first week, then 20 mg) – 20% reduction over placebo- And why ARB’s (angiotension receptor blockers) might help:
Candesartan (atacand)16 mg OD – 31% reduction headache hours over placebo
- And why ARB’s (angiotension receptor blockers) might help:
BMJ. 2001 January 6; 322(7277): 1-4
Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study
Harald Schrader free article here
Tronvik E, Stovner LJ, Helde G, Sand T, Bovim G. Prophylactic treatment
of migraine with angiotensin II receptor blocker. JAMA 2003;289:
65-9. free article here
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Oct;92(4):384-9.
Substance P and mast cells: preliminary histologic analysis of the human temporomandibular joint.
Henry CH, Wolford LM. abstract herethe association of mast cells and and substance P containing nerves gives it some credibility.
A previous study had noted mast cells in TMJ discs of TMJ dysfunctional subjects:
Arch Oral Biol. 1995 Jun;40(6):549-57.
A microscopic and immunocytochemical study of structural changes in dysfunctional
human temporomandibular joint discs
Marchetti C, Piacentini C, Farina A, Bernasconi G, Calligaro A. abstract here -
- abstract here
Arch Oral Biol. 1995 Jun;40(6):549-57.
A microscopic and immunocytochemical study of structural changes in dysfunctional
human temporomandibular joint discs
Marchetti C, Piacentini C, Farina A, Bernasconi G, Calligaro A. abstract hereCytokines are elevated in TMJ syndrome:
British Journal of Oral and Maxillofacial Surgery Volume 41, Issue 2, April 2003, Pages 95-101
Expression of interleukin 6 in synovial tissues in patients with internal derangement of the temporomandibular jointPrior gut trauma (previous infection), food allergy, and stress are key players in this mast cell contributing
- pain syndrome:
Mast cells: A possible link between psychological stress, food allergy,nd gut hypersensitivity in the Irritable Bowel syndrome
XIAN-YONG GUI
Journal of Gastroenterology and Hepatology Volume 13 Issue 10, Pages 980 – 989
abstract here
Activated Mast Cells in Proximity to Colonic Nerves Correlate With Abdominal Pain in Irritable Bowel Syndrome
GIOVANNI BARBARA,* VINCENZO STANGHELLINI,* ROBERTO DE GIORGIO,* CESARE CREMON,* GRAEME S. COTTRELL,‡ DONATELLA SANTINI,§ GIANANDREA PASQUINELLI,§
ANTONIO M. MORSELLI–LABATE,* EILEEN F. GRADY,‡ NIGEL W. BUNNETT,‡ STEPHEN M. COLLINS, and ROBERTO CORINALDESI*
GASTROENTEROLOGY 2004;126:693–702 free article here- There is evidence of activation of the immune system in Irritable bowel, in part probably mediated by mast cells:
Immune Activation in Patients With Irritable Bowel Syndrome
TOBIAS LIEBREGTS,*,‡ BIRGIT ADAM,*,‡ CHRISTOPH BREDACK,*,‡ ALEXANDER RÖTH,§ SUSANNE HEINZEL,SUE LESTER, SARAH DOWNIE–DOYLE, ERIC SMITH, PAUL DREW,NICHOLAS J. TALLEY,#,** and GERALD HOLTMANN*,‡
GASTROENTEROLOGY 2007;132:913–920 free article hereThe plot thickens with finding this inflammation associated with a leaky gut that can spawn further
-
- reaction:
-
- see
Irritable Bowel (IBS) Involves Excessive Permeability of Gut MembranesPart of the visceral hypersensitivity in IBS might be mediated by the fact that mast cells can cause persistent activation of “C” nerve fibers – in skin these fibers are associated with burning pain peripheral sensitization
-
- .
Mast cell-mediated long-lasting increases in excitability of vagal C fibers in guinea pig esophagus
Shaoyong Yu,1 Marian Kollarik,2 Ann Ouyang,1 Allen C. Myers,2 and Bradley J. Undem2
Am J Physiol Gastrointest Liver Physiol 293: G850-G856, 2007 abstract hereThe visceral hypersensitivity level, particularly in the diarrhea dominant Irritable bowel
- , correlates well with mast cell counts in the in the terminal ileum, ascending colon and rectum:
Journal of Gastroenterology and Hepatology Volume 21 Issue 1, Pages 71 – 78
Mucosal mast cell counts correlate with visceral hypersensitivity in patients with diarrhea predominant irritable bowel syndrome
JUNG HO PARK, POONG-LYUL RHEE, HYUN SEO KIM, JUN HAENG LEE, YOUNG-HO KIM, JAE JUN KIM AND JONG CHUL RHEE abstract here
So mast cells do double duty – help mediated peripheral sensitization and run allergic reactions.
Surveys have demonstrated people with IBS have intolerances to about 1/3 of foods. Dietary changes have an impact on IBS:
Is there a role of food allergy in irritable bowel syndrome and functional dyspepsia? A systematic review
M.I. Park & M. Camilleri
Neurogastroenterology & Motility Volume 18 Issue 8, Pages 595 – 607, 22 Dec 2005
abstract hereElimination diet is associated with improvement in 1/2 of cases (and if bacterial overgrowth
- had been dealt with, I bet that could have been even higher):
- Migraines – mast cell activity helps initiate problems in migraines:
- Mast cell degranulation activates a pain pathway underlying migraine headache
- The role of mast cells in migraine pathophysiology
Theoharis C. Theoharides, , Jill Donelan, Kristiana Kandere-Grzybowska1 and Aphrodite Konstantinidou2
Brain Research Reviews 49(1), July 2005, Pages 65-76 abstract here
No big surprise – stress helps initiate the mast cell activation to degranulate:
Endocrinology. 1995 Dec;136(12):5745-50.
Stress-induced intracranial mast cell degranulation: a corticotropin-releasing hormone-mediated effect.
Theoharides TC, Spanos C, Pang X, Alferes L, Ligris K, Letourneau R, Rozniecki
JJ, Webster E, Chrousos GP. abstract here
- Mast cell degranulation activates a pain pathway underlying migraine headache
TMJ
- TMJ – increased mast cells have been implicated in this disorder:
IRRITABLE BOWEL SYNDROME
- Irritable bowel syndrome: although there have been sporadic reports demonstrating increased mast cells in Irritable bowel for years, no one actually put two and two together until this landmark study was published in 2004:
EPIDEMIOLOGIC ASSOCIATION OF ABOVE DISEASES:
The above mentioned diseases are all interconnected:Re Fibromyalgia – stats from:
J Clin Rheumatol. 2006 Jun;12(3):124-8.
The incidence of fibromyalgia and its associated comorbidities: a population-based retrospective cohort study based on International Classification of Diseases, 9th Revision codes.
Weir PT, Harlan GA, Nkoy FL, Jones SS, Hegmann KT, Gren LH, Lyon JL. abstract here
Food intolerance and the irritable bowel syndrome
R NANDA, R JAMES, H SMITH, C R K DUDLEY, AND D P JEWELL
Glut, 1989, 30, 1099-1104 free article here
- dairy and wheat products were highest on list (so much for eating bran – use psillium instead)
D Levy, R Burstein, V Kainz, M Jakubowski, AM
Pain. 2007 July; 130(1-2): 166–176. free article hereInterestingly, part of the damage mast cells might inflict may be through the renin-angiotensin blood pressure system:
Mast Cells Activate the Renin Angiotensin System and Contribute to Migraine: A Hypothesis
Hisham Ba’albaki, MD; Alan Rapoport, MD
Headache 48 (10),2008 pp. 1499-1505Blockers of this system help migraines:
Ann Pharmacother. 2010 Feb;44(2):360-6. Epub 2010 Jan 19.
Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers for
the prevention of migraines.
Gales BJ, Bailey EK, Reed AN, Gales MA. abstract here
- which might explain why ACE (angiotension converting enzyme) inhibitor may help migraines:
lisinopril (10 mg first week, then 20 mg) – 20% reduction over placebo- And why ARB’s (angiotension receptor blockers) might help:
Candesartan (atacand)16 mg OD – 31% reduction headache hours over placebo
- And why ARB’s (angiotension receptor blockers) might help:
BMJ. 2001 January 6; 322(7277): 1-4
Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study
Harald Schrader free article here
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Oct;92(4):384-9.
Substance P and mast cells: preliminary histologic analysis of the human temporomandibular joint.
Henry CH, Wolford LM. abstract here
Tronvik E, Stovner LJ, Helde G, Sand T, Bovim G. Prophylactic treatment
of migraine with angiotensin II receptor blocker. JAMA 2003;289:
65-9. free article herethe association of mast cells and and substance P containing nerves gives it some credibility.
A previous study had noted mast cells in TMJ discs of TMJ dysfunctional subjects:
Arch Oral Biol. 1995 Jun;40(6):549-57.
A microscopic and immunocytochemical study of structural changes in dysfunctional
human temporomandibular joint discs
Marchetti C, Piacentini C, Farina A, Bernasconi G, Calligaro A. abstract here -
-
British Journal of Oral and Maxillofacial Surgery Volume 41, Issue 2, April 2003, Pages 95-101
Expression of interleukin 6 in synovial tissues in patients with internal derangement of the temporomandibular joint
J. Sato DDS, PhD et al.Mast cells release, among other things, cytokines. An exciting newer treatment for TMJ involves irritation of the joint to flush these irritating compounds out: lack of success with irritigation corrleated with the cytokine levels in the washed out synovial fluid:
inflammatory cytokines correlated with clinical outcome of temporomandibular joint irrigation in patients with chronic closed lock
Yoshiki Hamada, Toshirou Kondoh, Anders B. Holmlund, Matsuo Yamamoto, Akihisa Horie, Tomoyuki Saito, Ko Ito, Kanichi Seto, Hideki Sekiya
Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology – November 2006 (Vol. 102, Issue 5, Pages 596-601 abstract here -
Mast cells release, among other things, cytokines. An exciting newer treatment for TMJ involves irritation of the joint to flush these irritating compounds out: lack of success with irritigation corrleated with the cytokine levels in the washed out synovial fluid:
inflammatory cytokines correlated with clinical outcome of temporomandibular joint irrigation in patients with chronic closed lock
Yoshiki Hamada, Toshirou Kondoh, Anders B. Holmlund, Matsuo Yamamoto, Akihisa Horie, Tomoyuki Saito, Ko Ito, Kanichi Seto, Hideki Sekiya
Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology – November 2006 (Vol. 102, Issue 5, Pages 596-601 abstract here-
- Mast cells release, among other things, cytokines. An exciting newer treatment for TMJ involves irritation of the joint to flush these irritating compounds out: lack of success with irritigation corrleated with the cytokine levels in the washed out synovial fluid:
-
- So in TMJ, there is a mast cell – cytokine link
Activated Mast Cells in Proximity to Colonic Nerves Correlate With Abdominal Pain in Irritable Bowel Syndrome
GIOVANNI BARBARA,* VINCENZO STANGHELLINI,* ROBERTO DE GIORGIO,* CESARE CREMON,* GRAEME S. COTTRELL,‡ DONATELLA SANTINI,§ GIANANDREA PASQUINELLI,§
ANTONIO M. MORSELLI–LABATE,* EILEEN F. GRADY,‡ NIGEL W. BUNNETT,‡ STEPHEN M. COLLINS, and ROBERTO CORINALDESI*
GASTROENTEROLOGY 2004;126:693–702 free article here- “There was a 150% increase in the number of degranulating mast cells” (P<.001)
- Only the cases that had more abdominal pain had “mast cells in close proximity
to nerves” (p=0.003)
Animal studies have confirmed the mast cell presence is a cause of the abdominal pain:
Gastroenterology. 2007 Jan;132(1):26-37.
Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome.
Barbara G, Wang B, Stanghellini V, de Giorgio R, Cremon C, Di Nardo G, Trevisani
M, Campi B, Geppetti P, Tonini M, Bunnett NW, Grundy D, Corinaldesi R.
abstract here free html here- Prior gut trauma (previous infection), food allergy, and stress are key players in this mast cell contributing pain syndrome:
Mast cells: A possible link between psychological stress, food allergy,and gut hypersensitivity in the Irritable Bowel syndrome
XIAN-YONG GUI
Journal of Gastroenterology and Hepatology Volume 13 Issue 10, Pages 980 – 989
abstract here- There is evidence of activation of the immune system in Irritable bowel, in part probably mediated by mast cells:
Immune Activation in Patients With Irritable Bowel Syndrome
TOBIAS LIEBREGTS,*,‡ BIRGIT ADAM,*,‡ CHRISTOPH BREDACK,*,‡ ALEXANDER RÖTH,§ SUSANNE HEINZEL,SUE LESTER, SARAH DOWNIE–DOYLE, ERIC SMITH, PAUL DREW,NICHOLAS J. TALLEY,#,** and GERALD HOLTMANN*,‡
GASTROENTEROLOGY 2007;132:913–920 free article here-
- The plot thickens with finding this inflammation associated with a leaky gut that can spawn further reaction:
-
- see
Irritable Bowel (IBS) Involves Excessive Permeability of Gut Membranes
-
- Part of the visceral hypersensitivity in IBS might be mediated by the fact that mast cells can cause persistent activation of “C” nerve fibers – in skin these fibers are associated with burning pain peripheral sensitization.
Mast cell-mediated long-lasting increases in excitability of vagal C fibers in guinea pig esophagus
Shaoyong Yu,1 Marian Kollarik,2 Ann Ouyang,1 Allen C. Myers,2 and Bradley J. Undem2
Am J Physiol Gastrointest Liver Physiol 293: G850-G856, 2007 abstract here- The visceral hypersensitivity level, particularly in the diarrhea dominant Irritable bowel, correlates well with mast cell counts in the in the terminal ileum, ascending colon and rectum:
Journal of Gastroenterology and Hepatology Volume 21 Issue 1, Pages 71 – 78
Mucosal mast cell counts correlate with visceral hypersensitivity in patients with diarrhea predominant irritable bowel syndrome
JUNG HO PARK, POONG-LYUL RHEE, HYUN SEO KIM, JUN HAENG LEE, YOUNG-HO KIM, JAE JUN KIM AND JONG CHUL RHEE abstract here
-
- So mast cells do double duty – help mediated peripheral sensitization and run allergic reactions.
- Surveys have demonstrated people with IBS have intolerances to about 1/3 of foods. Dietary changes have an impact on IBS:
Is there a role of food allergy in irritable bowel syndrome and functional dyspepsia? A systematic review
M.I. Park & M. Camilleri
Neurogastroenterology & Motility Volume 18 Issue 8, Pages 595 – 607, 22 Dec 2005
abstract here- Elimination diet is associated with improvement in 1/2 of cases (and if bacterial overgrowth had been dealt with, I bet that could have been even higher):
Food intolerance and the irritable bowel syndrome
R NANDA, R JAMES, H SMITH, C R K DUDLEY, AND D P JEWELL
Glut, 1989, 30, 1099-1104 free article here
- dairy and wheat products were highest on list (so much for eating bran – use psillium instead)
-
- People with fibromyalgia are 3.5 -5 times more likely to have irritable bowel; and are 3.5-4.3 times more likely to have migraines. Mast cell degranulation in interstitial cystitis causes a adrenaline-like hyper state that increases the incidence of panic attacks in that condition. In fibromylagia, the incidence of anxiety is 3 – 4.5 times more likely.
Re irritable bowel
-
- – stats from:
Prevalence of Fibromyalgia in patients with Irritable bowel Syndrome
Irritabl barsak et al
Turk J Gastoenterol 2001; 12(2) 141-4 article here-
- In irritable bowel, the incidence of FM varied with the study – 23.1, 28, and 31.6% while the incidence of FM in the general population is 6.88% – that’s 3.4 to 4.6 times more likely for someone with irritable bowel to have Fibromyalgia.
In interstitial cystitis
-
- according to:
COMORBIDITY OF INTERSTITIAL CYSTITIS WITH OTHER UNEXPLAINED CLINICAL CONDITIONS
C. A. TONY BUFFINGTON
THE JOURNAL OF UROLOGY Vol. 172, 1242–1248 free article here-
- the incidence of irritable bowel is 3.4 – 10.3 times as likelyComment – So the so-called “somatization diseases” appear to represent different manifestations of mast cell diseases. The mast cell presence may represent a form of peripheral sensitization as damaged nerves back spilling irritating neurotransmitters that attract mast cells. Fibromyalgia has a more generalized expression of mast cells. “FMS seems to be a papillary dermis disease associated with increased numbers of mastocytes”
Systemic mastocystosis and testing with serum tryptase testing
-
- :Systemic Mastocytosis is a disease with multiple “systemic symptoms” such as fatigue, headache, flushing, abdominal discomfort, nausea, hypotension, and tachycardia.
A potentially useful test is the serum tryptase – in this disease it is typically over 20 ng/ml.
Rev Med Suisse. 2009 Apr 15;5(199):837-42.
[Mastocytosis: when should it be considered?] [Article in French]
Comte-Perret S, Bart PA, Spertini F, Leimgruber A. abstract here
Eur J Gastroenterol Hepatol. 2009 Mar;21(3):273-7.
Mast cell tryptase in sera of patients with Crohn’s disease and mastocytosis.
de Rossi TM, Krauss N, Wilken V, Giera B, Konturek PC, Kressel J, Hahn EG, Raithel M.-
- They comparied serum tryptase levels in crohn’s disease and mastocytosis, they found
-
- controls – tryptase 2.4±1.0.crohn’s – 2.6±2.4mastocytosis – (21.19±18.55, P<0.0001) – I wonder if some of the cases that were not high had been treated with anti-cancer drugs because there is a malignant spectrum subtype; this treated group might not show the elevation. It does appear a level over 20 is confirmative.One study suggested if the tryptase levels were under 20, it probably meant they had only the skin disease variant:
The alpha form of human tryptase is the predominant type present in blood at baseline in normal subjects and is elevated in those with systemic mastocytosis.
Lawrence B. Schwartz,* Kentaro Sakai,* Timothy R. Bradford,* Shunlin Ren,* Burton Zweiman* Alexandra S. Worobec,§ and Dean D. Metcalfe
The Journal of Clinical Investigation Volume 96, December 1995, 2702-2710 free article here-
- Someone at our lab considers the only time to do a test is during an allergic reaction – that is a test for anaphylaxis and not what we are looking for here. Will have to talk with these people…BTW – if you have mastocytosis or suspect so – DO NOT have a general anesthetic done until an anesthetist has set up precautions otherwise the surgery may kill you…
Anaesthesist. 2009 Dec;58(12):1239-43.
[Mastocytosis. A challenge in anaesthesiology]
[Article in German]
Konrad FM, Unertl KE, Schroeder TH. english abstract here- The question now, is how does one get rid of these mast cells, and how can you stabilize them? Opioids cause histamine release from mast cells which might explain why subjects with Fibromyalgia do not respond well to these agents…I hope to have a new blog note on treatments for mast cell diseases if an interest is shown..
J. Sato DDS, PhD et al. abstract here
inflammatory cytokines correlated with clinical outcome of temporomandibular joint irrigation in patients with chronic closed lock
Yoshiki Hamada, Toshirou Kondoh, Anders B. Holmlund, Matsuo Yamamoto, Akihisa Horie, Tomoyuki Saito, Ko Ito, Kanichi Seto, Hideki Sekiya
Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology – November 2006 (Vol. 102, Issue 5, Pages 596-601 abstract hereSo in TMJ, there is a mast cell – cytokine linkIRRITABLE BOWEL SYNDROME
- Irritable bowel syndrome: although there have been sporadic reports demonstrating increased mast cells in Irritable bowel for years, no one actually put two and two together until this landmark study was published in 2004:
- “There was a 150% increase in the number of degranulating mast cells” (P<.001)
- Only the cases that had more abdominal pain had “mast cells in close proximity
to nerves” (p=0.003)
Animal studies have confirmed the mast cell presence is a cause of the abdominal pain:
Gastroenterology. 2007 Jan;132(1):26-37.
Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome.
Barbara G, Wang B, Stanghellini V, de Giorgio R, Cremon C, Di Nardo G, Trevisani
M, Campi B, Geppetti P, Tonini M, Bunnett NW, Grundy D, Corinaldesi R.
abstract here free html here24.4% of IC had irritable bowel vs 5.2 in control group
17.7% had Fibromyalgia vs. 2.6% in control group
9.5% had chronic fatigue vs 1.7% in control groupMast cell disease is so bad in this condition, a mast cell inhibitors, hydroxyzine (atarax) and Singulair (montelukast) form intregral parts of the treatment: -
-
British Journal of Oral and Maxillofacial Surgery Volume 41, Issue 2, April 2003, Pages 95-101
Expression of interleukin 6 in synovial tissues in patients with internal derangement of the temporomandibular joint
J. Sato DDS, PhD et al.Mast cells release, among other things, cytokines. An exciting newer treatment for TMJ involves irritation of the joint to flush these irritating compounds out: lack of success with irritigation corrleated with the cytokine levels in the washed out synovial fluid:
inflammatory cytokines correlated with clinical outcome of temporomandibular joint irrigation in patients with chronic closed lock
Yoshiki Hamada, Toshirou Kondoh, Anders B. Holmlund, Matsuo Yamamoto, Akihisa Horie, Tomoyuki Saito, Ko Ito, Kanichi Seto, Hideki Sekiya
Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology – November 2006 (Vol. 102, Issue 5, Pages 596-601 abstract here
inflammatory cytokines correlated with clinical outcome of temporomandibular joint irrigation in patients with chronic closed lock
Yoshiki Hamada, Toshirou Kondoh, Anders B. Holmlund, Matsuo Yamamoto, Akihisa Horie, Tomoyuki Saito, Ko Ito, Kanichi Seto, Hideki Sekiya
Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology – November 2006 (Vol. 102, Issue 5, Pages 596-601 abstract here

Great research. I have also linked degranulating mast cells to all of the conditions you have listed, with the exception of TMJ. I am very interested in your musings on stabilizing mast cells.
I am DXed with a condition called mast cell activation syndrome/disorder MCAS/MCAD by Dr. Marianna Castells at Brigham & Women’s.
I must take daily doses of H-1’s (zyrtec AM/atarax PM), H-2 (ranitidine), and singulair to prevent symptoms. With these meds, I am practically symptom free. Without them, I am incredibly ill including anaphylactoid episodes despite the fact that I have NO allergies.
Good Stuff. Keep researching!
Here are several other informative links on the subject:
1. http://mastcelldisorders.lefora.com/2010/08/08/interesting-blog-is-fibromyalgia-a-mast-cell-disea/
2. http://www.drlucas.de/assets/applets/Fibromyalgia__IJIP.pdf
3. http://www.therapath.com/Mast_Cell_Density.php
4. http://www.curetogether.com/mastocytosis/symptoms/
#4 is particularly interesting. Its a survey of patients diagnosed with mastocytosis. The symptoms have signficant overlap with fibromyalgia
You can actually order a skin biopsy test for mast cell density.
Here’s a link: http://www.therapath.com
Thanks for all the research. I would love it if you decided to post more along these lines. I was diagnosed with fibro in 1997 and now likely have MCAD. I’m not sure if I was misdiagnosed in ’97 or now have both.
Wow, I was diagnosed with fibromyalgia over 12 years ago. Back then, they thought I was nuts with the itching skin, ic, tmj, and esophagus and bladder spasms. Now it’s all starting to make sense.
I have read so many articles or reviews on the topic of the blogger lovers however
this piece of writing is genuinely a good article, keep it up.
I believe the problem with mast cells is related to “biome depletion,” i.e. the elimination of keynote species from the human gut ecology. http://sciences.surgery.duke.edu/research/institutes-and-labs/parker-lab
I also think the connection between mast cells and fibromyalgia may have to do with nutritional deficiencies linked to malabsorption. Malabsorption is a known problem in mast cell disorders. Thanks for a thoughtful site. I think you’re on to something.
http://www.ncbi.nlm.nih.gov/pubmed/24784142
http://www.ncbi.nlm.nih.gov/pubmed/20428906
http://www.ncbi.nlm.nih.gov/pubmed/10027670
http://www.ncbi.nlm.nih.gov/pubmed/22594347
http://www.ncbi.nlm.nih.gov/pubmed/22311432
http://www.ncbi.nlm.nih.gov/pubmed/21894355
http://www.ncbi.nlm.nih.gov/pubmed/15945613
http://www.ncbi.nlm.nih.gov/pubmed/22271372