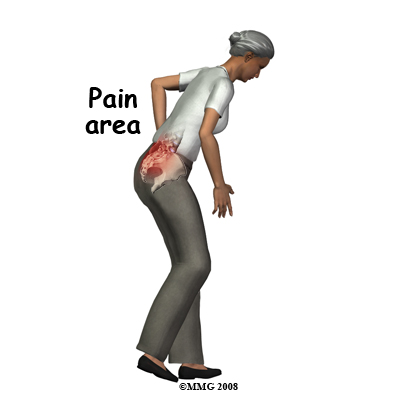
One elderly lady, I recently saw, fell and multiple fractured her left humerus. Was seen, put in a sling, kept briefly in hospital and discharged. Because she could not walk, she was reassessed and found to have a pubic ramus fracture – kept in hospital briefly by hospitalist and sent home. Recently I saw her and found serious tenderness over the sacrum – very much suggesting a sacral fracture. Regular xrays are often useless because this area is covered with gas. In certain elderly osteoporotic cases, the sacrum can fracture in what is called a sacral insufficiency fracture without even any trauma. This can cause longstanding pain without being diagnosed because doctors have excessive faith in xrays
American Journal of Emergency Medicine (2010) in press
Sacral insufficiency fractures: an easily overlooked cause of back pain in the ED
John G. Galbraith, Joseph S. Butler, Simon P. Blake, Gemma Kellehe abstract here
- Co- existent pubic bone fractures and “parasymphyseal region”, occur in up to 88% cases (like my lady above)
- In absence of injury, can present with intractable back pain over age 50 with normal xrays (except for osteoporosis) and normal lab work
- Osteoporosis and prior radiotherapy are risk factors
- sacral tenderness
Test I tried on sacarum is a balottment technique devised by Dr. K. Lewitt:- Patient, lying down facing you, with hips drawn up to 90 degrees
- Put patient’s knees on the your abdomen
- put your hands on sacrum
- push knees back with your abdomen while pushing forward with hands on sacrum. Pain will be elicited – and by moving your hands can be quite specific – can ballot the low thoracic/lumbar levels as well for vertebral fracture.
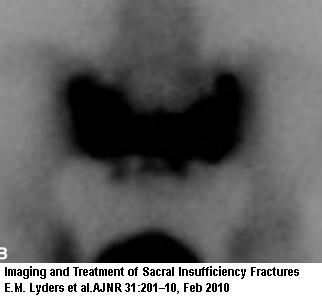
- Bone scan is 96% sensitive and 92% specific – but cannot differentiate cancers
- CT scan is considered gold standard
TREATMENT
- Usual treatment involves “bed rest with gradual mobilization” and a walker. – symptoms can take 6-15 months to resolve. The debility and embolic complications can lead to a 14.3% overall mortality
- Newer techniques involves polymethylmethacrylate cement injection into the fracture site:good discussion is here:
Imaging and Treatment of Sacral Insufficiency Fractures
E.M. Lyders, C.T. Whitlow, M.D. Baker, P.P. Morris
AJNR Am J Neuroradiol 31:201–10, Feb 2010 free article here Sacroplasty – is the specific sacral injection procedure. One prospective trial found:
prospective 50% reduction in the pain level by 2 days, 80% by 2 weeks, and 90% at 1
year:
Frey ME, DePalma MJ, Cifu DX, et al. Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J 2008;8:367–73. Epub 2007 Jul 20 - Good review of sacroplasty here:
European Spine Journal Volume 18, Number 9, 1266-1271, 2009
Clinical outcomes of sacroplasty in sacral insufficiency fractures: a review of the literature
Edward Bayley, Shreya Srinivas and Bronek M. Boszczyk abstract here - Screw placement is another technique used
Addendum:
IASP Poster Presentation Number: PW 401, Montreal 2010
PERCUTANEOUS SACROPLASTY (PS) CT-SCAN GUIDED FOR THE TREATMENT OF SACRAL INSUFFICIENCY FRACTURES (SIFS)
R. H. Wortley1,2, S. Pilheu1, C. Stinga1, V. D’Acunha1, L. C. Daldovo1, M. Romano3
- 11 cases
- pains 9/10
- minimally invasive – done under local! – discharged within 12-24 hours
- complete pain relief 52%; Moderate pain relief (VAS 3-5) in 35%; poor pain control (6-8) 4.25%
- Not effective in 2 patients with lumbar arthrodesis and associated pubis fractures.
- No one worse – one had asymptomatic cement leak into S1 foramen
Comment – I have used 3 day – 30 mg/day Pamidronate in one case with rather good relief of pain (was a postlaminectomy case as well – so hard to tell). Sacroplasty seems very easy and very effective.
It does seem the only way to diagnose this condition is to be aware of it ahead of time and to look for it…
We need to teach our medical student well…
A good overall discussion of this condition is available here
any comments?
