- Erythromelalgia (EM) is a syndrome of burning pain in the feet often accompanied by redness and warmth,and often aggravated by heat and exercise. Cold water soaks are the mainstay of treatment. Painkillers are usually ineffective. IV lidocaine and mexelitine hold promise. Some cases are more complex then they seem.

Reviews Include:
Mayo clinic series:
Archives of Dermatology 136(3), March 2000,330-336
Natural History of Erythromelalgia: Presentation and Outcome in 168 PatientsZ
Davis, Mark D. P. MB, MRCPI; O’Fallon, W. Michael PhD; Rogers, Roy S. III MD; Rooke, Thom W. MDRecent review:
J Vasc Nurs. 2010 Jun;28(2):67-71.
Erythromelalgia: a rare microvascular disease.
Latessa V abstract here
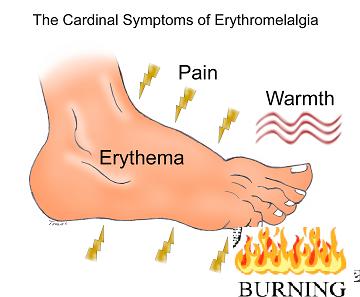
Symptoms include:
- redness- erythema
- Pain + burning – 1/2 felt it as hot and 2/3 as burning according to Mayo clinic study
- Warmth
- in response to warmth and exercise
Primary EM
- rare disorder in caucasians- most adult onset – 4.2% childhood
- Rarely (4.7% in Mayo clinic series) it can be autosomal dominant form is a disorder of pain neuron sodium 1.7 channels . Interesting, sodium channel blockers include most neuropathic used drugs:
- Amitriptyline and other Tricyclic drugs
- Anticonvulsants
- Most interestingly includes parenteral lidocaine and oral Mexiletine
Curr Pharm Des. 2005;11(23):3005-11.
Sodium channel blockers in neuropathic pain.
Kalso E. abstract here - This condition is distinct from another Na channel 1.7 disorder called Paroxysmal Extreme Pain Disorder (PEPD) – severe pain and skin flushing precipitated by perineal groin nerve activation and bowel movements:
Mol Pain. 2008 Sep 19;4:37.
Paroxysmal extreme pain disorder M1627K mutation in human Nav1.7 renders DRG
neurons hyperexcitable.
Dib-Hajj SD, Estacion M, Jarecki BW, Tyrrell L, Fischer TZ, Lawden M, Cummins TR,
Waxman SG. free article here - described as a cutaneous microvascular disorder – the opposite of raynaud’s phenonmenon – where there is vascular engorgement that results in actual decrease blood perfusion and hypoxia as consequence – with burning pain as result.
- small-fiber neuropathy has been found associated:
J Am Acad Dermatol. 2006 Sep;55(3):519-22.
Histopathologic findings in primary erythromelalgia are nonspecific: special studies show a decrease in small nerve fiber density.
Davis MD, Weenig RH, Genebriera J, Wendelschafer-Crabb G, Kennedy WR, Sandroni P. abstract
Secondary EM
occurs as a consequence of other diseases which includes:
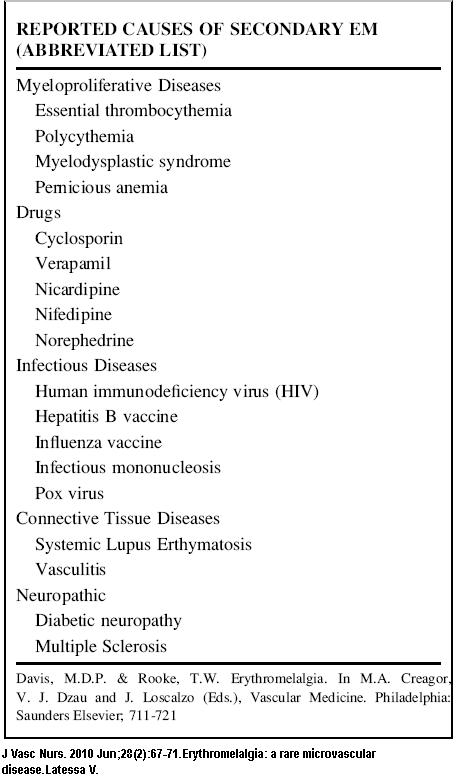
Also:
- gout
- Rheumatoid arthritis
- musculoskeletal disease such as sciatica
- mercury poisoning
- Fabry’s disease
- certain platelet disorders like thrombotic thrombocytopenic purpura
- HIV – AIDs
Differential Diagnosis
Considered more in the differential diagnosis (as per
J Vasc Nurs. 2010 Jun;28(2):67-71.Erythromelalgia: a rare microvascular disease.Latessa V.)
included:
- skin infections – Cellulitis, erysipelas
- skin rashes – Dermatitis
- Complex Regional Pain Syndrome – though I wonder if there is not some in EM
- Systemic Lupus Erythromatosis (SLE)
- Raynaud’s phenomenon – though the white finger/toe (s) should be a dead givaway
- Peripheral neuropathy
- Fabry disease
- Arterial or venous insufficiency – raising the leg should give it a pallor that turns red when then put down again. Need to check the pulses..
- Gout – and don’t forget allopurinol can cause peripheral neuropathy – have a case of such though no EM.
I had one case who developed EM after being started on Nifedipine. She was inconsiderable distress and it was a very scary situation. Besides stopping the drug, I started her on Prednisone 30 mg/day which mercifully remitted her condition. It makes one think it is similar to complex regional pain where steroids can be acutely used. Steroids were found helpful in an acute childhood EM situation:
Childhood steroid-responsive acute erythromelalgia with axonal neuropathy of large myelinated fibers: A dysimmune neuropathy?
Zoltan Pfund a, Jozsef Stankovics b, Tamas Decsi b, Zsolt Illes a,
Neuromuscular Disorders 19 (2009) 49–52 abstract here
They used ” methylprednisolone (MP) therapy was initiated (500 mg for 5 days in infusion, then oral MP slowly tapered for 3 months)…symptoms in the feet started to subside in the next two weeks.”
Triggers:
- Heat – dressing too warm. hot weather
- Night – especially if hot out and feet covered
- Prolonged standing
- exercise like brisk walking
- alcohol
- caffeine mentioned by one
- medications – one not mentioned but could be inadvertently given could be the niacin in vitamins. It can cause a flush and I wonder if it makes things worse.
- certain spices
- certain fruits – particularly melon seems to be mentioned
- large amounts of sugar mentioned in one article
Testing
Diagnosis is often clinical but testing would include:
If does not look good see in separate window Here
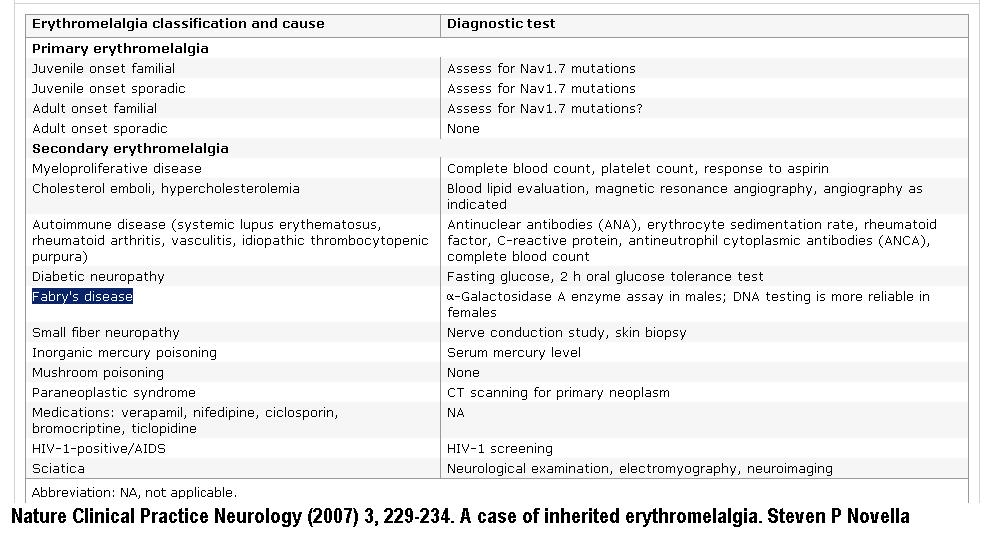 at: http://www.nature.com/nrneurol/journal/v3/n4/full/ncpneuro0425.html
at: http://www.nature.com/nrneurol/journal/v3/n4/full/ncpneuro0425.html
Elevated ESR and serum protein electrophoresis and be seen in 1/2 of Mayo clinic series
Watch out for increased WBC or platelet counts.
Mayo Clinic study facts
In a Mayo Clinic study (168 cases) the following associations were found:
- 3:1 female: male. All causacian.
- Average age 55.8 ± 18.9 years; range, 5 to 91 years. Three patients were 11 years old or young
- 97% had intermittent symptoms
- 88% feet; 25% hands
- 50% had a history of smoking
- 11.3% had a high cholesterol – I’m not sure a statin would be a wise idea in this disorder.
- 13.7% had hypertension – maybe avoid calcium channel blockers which cause vasodilation; – though it is also listed as a treatment in some cases…
- diabetes 2.4%
- myeloproliferative disease in 8.9%
- polycythemia rubra vera in 5.3% , essential thrombocythemia in 2.3% , and chronic granulocytic leukemia in 1%.
Prognosis:
“Over time, the symptoms can worsen, stay the same, improve, or resolve in approximately equal proportions.” as per Mayo clinic here
3 Catagories of EM
Back in the 1990’s it was suggested that there were 3 catagories of EM and each had different treatments:
BMJ. 1990 September 8; 301(6750): 454–455.
Three types of erythromelalgia.
J P Drenth and J J Michiels free article here
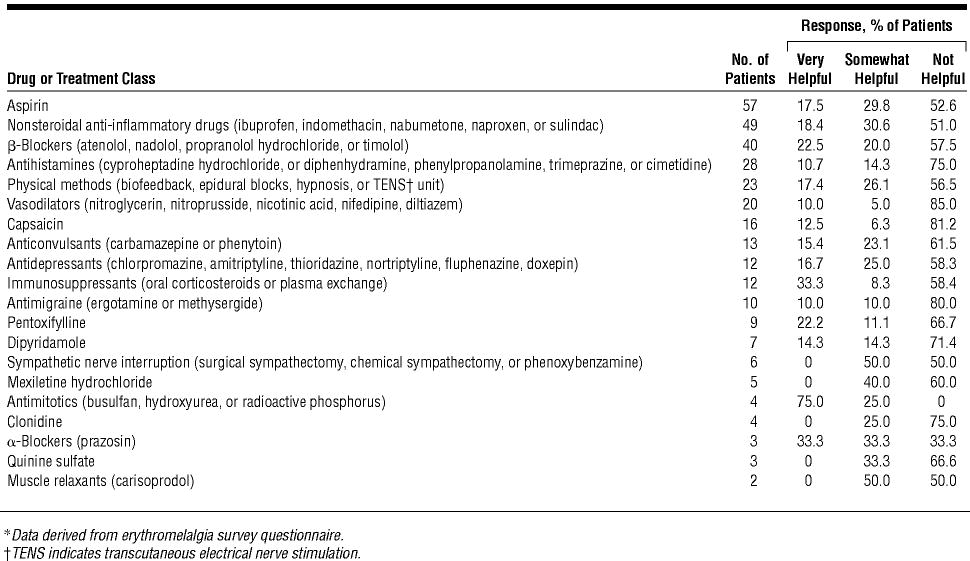
- associated with thrombocythaemia of platelets and a good response to aspirin or NSAID anti-inflammatory agents. – In Mayo clinic article 17.5% had excellent response to aspirin and 18.4% to NSAID’s. One free ASA article:
Krishnan S, Yesudian PD, Jayaraman M, Jan. Erythromelalgia responding to aspirin. Indian J Dermatol Venereol Leprol 1996;62:204-5 article here - Primary – given this is a sodium 1.7 channel disorder, all the agents for Na channel neuropathy could help – IV lidocaine and mexiletine stand out as recent artcile notations
- secondary EM – treat the underlying condition
Treatments
There is a proliferation of treatments that work in case studies, and some that are now becoming more popular:
- ice water; store shoe in freezer; walk in snow barefoot
- airconditioners or blow fans across their affected areas
- avoid prolonged standing
- Would sure what to know that patient’s B12 levels were normal..
- Aspirin –
- If you cannot see drug list below see in separate window here
Mexiletine
A couple recent article found Mexiletine in children helpful:
Ann Saudi Med. 2009 Jul-Aug;29(4):316-8.
Experience with oral mexiletine in primary erythromelalgia in children.
Iqbal J, Bhat MI, Charoo BA, Syed WA, Sheikh MA, Bhat IN
abstract here free article here
- 12 year old boy
- started on mexiletine 100 tid – increased to 200 tid (3 times a day)
- relief started after 2 weeks and continued to improve up to 6 weeks
Mexiletine-responsive erythromelalgia due to a new Nav1.7 mutation showing use-dependent current fall-off
Jin-Sung Choi a,b,c, Lili Zhang d, Sulayman D. Dib-Hajj a,b,c, Chongyang Han, Lynda Tyrrell ,
Zhimiao Lin d, Xiaoliang Wang , Yong Yang, Stephen G. Waxman
Experimental Neurology 216 (2009) 383–389
7 year old girl on Mexiletine 300 mg/day – improvement continued even after drug was stopped
In the pain world, IV lidocaine is often used prior to mexiletine-5 mg/kg given over 1 hour – a good response would suggest mexiletine might be worthwhile trying.
Comment – Although it is obvious, I would select out another group – Those with Complex Regional Pain symptoms. Treatments would include:
- sympathetic blocks
________________________________________________________________________ - Dealing with any peripheral factors – a common factor I see in many conditions. If I may digress, I would like to describe a case of “sciatica” that was left disabled
- gentleman in his late 50’s with several year history of medial ankle, leg, anterior thigh and buttock/back pain. Disabled and used a cane.
- Finally had nerve testing done which suggested a tarsal tunnel syndrome – for which there was a concern no surgeon would be know how to treat.
I have written about it in regard to diabetics:
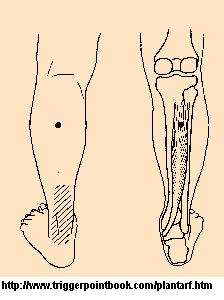
Surgery For Diabetic Peripheral Neuropathy – Another Option Not Available Here - Not only did he have tarsal tunnel with a tinel’s sign at ankle (see above link) but he had noted he had become more flat footed in past few years and was very tender over his tibilais posterior tendon nearby. – indicating he has torn his posterior tibialis tendon – something that occurs in not infrequently in older age groups
J Bone Joint Surg Am. 1999;81:1173-82.
GREGORY C. POMEROY, R. HOWARD PIKE, TIMOTHY C. BEALS and ARTHUR MANOLI
Current Concepts Review – Acquired Flatfoot in Adults Due to Dysfunction of the Posterior Tibial Tendon free article here - Knowing he had posterior tibialis tendonitis,I sought out the posterior tibialis muscle. About 1/3 way down the back of calf from knee and in deep in between the calf muslces can be realized a tenderness (maybe bit lower than this image in this case):
- I needled the posterior tibialis muscle going anteriorly and using an acupuncture needle threaded between the tibia-fibula (safer as nerves/blood vessels anteriorly). While needling I applied pressure posteriorly on the sore area. I used a pointer plus to pulse- needle area until it was no longer tender. This took significant pain away from ankle temporarily.
- Now getting to the sciatica part – he could bend forward and touch toes so I knew this had to be a more peripheral sciatic nerve entrapment and sure enough his piriformis was very tender.
- I stretch massaged the piriformis muslce using a technique in which you engage the muscle either from below or above and push tangentually It is described here:
How Should One Investigate Chronic Back Pain and What about the Back Muscles?
the procedure takes 10-20 minutes and I do knuckling back and forth over muscle over 120 times to get residual spasm released and then SI mobilize and lightly finger massage after. - There was some anterior quads tenderness but it massaged out easily
- Kenalog was injected parallel to tibialis posterior tendon where still sore.
- What was thought for years to be only sciatica turned out to have significant peripheral issues:
- piriformis syndrome – needs 2-3 months of twice weekly stretching – assuming cannot afford Botox.
- tibialis posterior triggers – can be very painful and respond amazingly to needling
- Tibialis posterior tendonitis and tearing
- Tarsal tunnel syndrome – anyone know a surgeon in Saskatchewan who does this?
- pes planus (flat feet) – had been given an arch support blank but it was not significantly tilted “posted” – I put adhesive moleskin to post it higher medially on heel.
OK – long story – now a EM case: – Piriformis contribution:
I have mild EM that only bothers me on hot summer days ( One good reason to be in cool Canada). I had had a piriformis problem after driving a long distance with a wallet in my back pocket (boy don’t do that anymore). During a hot period some years later, my EM started to bother me. One night not only were my feet hot, my right foot was painful as well, although it just seemed to be one pain. I thought about my piriformis and pressed over the area. It was tender and when I hit the right spot, I could feel the muscle vibrating under my pressing fingers. After a while the tenderness remitted, the pain in the leg disappeared and the hot feet were not particularly bothersome at all anymore – and I went to sleep.
I contend anyone with significant pain in the leg with EM will have significant peripheral elements – a piriformis, muscle leg knots that should be needled and massaged, tendonitis that may need injection, and perhaps a tarsal tunnel. It is noted that sciatica can cause EM and steroid epidurals/ Enbrel shots would be helpful there as well.
New solution was its response to transcranial magnetic stimulation:
Int J Dermatol. 2018 Mar 10.
doi: 10.1111/ijd.13963. [Epub ahead of print]
Erythromelalgia: improvement in pain with transcranial magnetic stimulation.
Tjahjono LA et al
https://www.ncbi.nlm.nih.gov/pubmed/29524220
Would be interested in comments
addendum:
In new onset cases, triggered by drugs, trauma, infection, there is a early phase where steroid could shut it down:
I will include abstract as it is not readily available
Pain Medicine 18(3) march 2017 abstract 160
160
Erythromelalgia: A Steroid-Responsive Subset
Gabriel Pagani-Estevez, MD, paganiestevez.gabriel@mayo.edu1; Paola Sandroni, MD PhD1; Mark Davis, MD1; James Watson, MD1; (1) Mayo Clinic, Rochester
Introduction:
Erythromelalgia is a rare pain disorder characterized by the clinical triad of severe, usually distal, extremity pain, redness, and elevated temperature that is highly disabling and often treatment-refractory. Corticosteroids (CS) may benefit certain erythromelalgia patients and this study was designed to determine clinical predictors of corticosteroid-responsive erythromelalgia.
Materials and Methods: Following IRB approval, Erythromelalgia patients who received CS were retrospectively identified and stratified into corticosteroid non-responders (NR), partial-corticosteroid responders (PSR), complete-corticosteroid responders (CSR) and corticosteroid responders (SR=PSR+CSR). In the study variable analysis, a p-value less than 0.05 was considered statistically significant.
Results: The median (interquartile range) age of the 31-patient cohort was 47 (26–57) and 22 (71%) were female. Fourteen (45%) were NR, 17 (55%) SR, 8 (26%) PSR and 9 (29%) CSR. A subacute temporal profile to disease zenith (<21 days) was described in 15 (48%) patients, of whom 13 (87%) were SR (p = 0.003; OR 0.069: CI 0.011–0.431). Six (67%) CSR reported a disease precipitant (surgery, trauma, infection) (p = 0.007; OR 12.667; CI 2–80.142). SR patients received CS sooner than NR at 3 (3-12) versus 24 (17-45) months (p = 0.003). A high-dose CS trial ( > = 200 mg prednisone cumulatively) was administered to 17(55%) patients, of whom 13(76%) were SR (p = 0.012; OR 8.125;CI 1.612–40.752).
Conclusions: An infectious, traumatic, or surgical precipitant and subacute presentation may portend steroid-responsive erythromelalgia. A transient “golden window” where corticosteroid intervention is useful may exist before irreversible nociceptive remodeling and central sensitization occurs.
References:
1) Laughlin RS, Dyck PJ, Watson JC, et al. Ipsilateral inflammatory neuropathy after hip surgery. Mayo Clin Proc. 2014;89(4):454-461.
2) Davis MD, O’Fallon WM, Rogers III RS, et al. Natural history of erythromelalgia: presentation and outcome in 168 patients. Arch Dermatol. 2000;136(3):330-336.
3) Oaklander AL, Klein MM. Evidence of small-fiber polyneuropathy in unexplained, juvenile-onset, widespread pain syndromes. Pediatr. 2013;131(4):e1091-1100.

Hi Everybody,
I thought you might be interested in this website about EM. You can check it out here: http://www.rarediseasestudy.org
I am a medical student!!! Your blog is very helpful for me….i get good information from your blog!!!!
Statin drugs cause this disorder! The public needs to be warned about this.
My 7 year old daughter has been diagnosed with EM in the genital area, we live in Australia and can’t seem to find any doctors who have knowledge in EM. She is currently on 600mg per day of Gabapentin and Tegretol 3 times a day.
————————
First question is whether she responded to 81 mg of aspirin/day
There was a recent Australian article where a child was even loosing his teeth from the erythmelalgia:
Pediatr Dent. 2012;34(5):422-6.
Erythromelalgia presenting with premature exfoliation of primary teeth: a diagnostic dilemma.
Prabhu N, Alexander S, Wong P, Cameron A. abstract here:
http://www.ncbi.nlm.nih.gov/pubmed/23211921
when the dust settled, “She was treated with low-grade aspirin therapy which led to a remarkable recovery”
Secondly is this a recent event?
Is so, it could respond to a pulse of steroids:
Childhood steroid-responsive acute erythromelalgia with axonal neuropathy of large myelinated fibers: A dysimmune neuropathy?
Zoltan Pfund a, Jozsef Stankovics b, Tamas Decsi b, Zsolt Illes a,
Neuromuscular Disorders 19 (2009) 49–52
http://www.ncbi.nlm.nih.gov/pubmed/19056270
Pulse steroid clinicians used to use IV methyprednisolone pulse therapy but found you can quickly run out of veins that way. In a conditions called ITP they found they could give the pulse therapy with oral dexamethasone 40 mg/day and get same results as IV:
PULSED HIGH-DOSE DEXAMETHASONE THERAPY IN CHILDREN WITH CHRONIC IDIOPATHIC THROMBOCYTOPENIC PURPURA
Pediatric Hematology-Oncology 2002, Vol. 19, No. 5 , Pages 329-335
Yasser A. Wali, Zakia Al Lamki, Wasifuddin Shah, Mathew Zacharia and Ahmed Hassan abstract here:
http://informahealthcare.com/doi/abs/10.1080/08880010290057345
Might be worth a try if not had too long.
From what I can tell, Genital Erythromelalgia is extremely rare and that diagnosis would be easier to make if there was Erythromelalgia in the family. The combination of carbamazepine and gabapentin has been used in some cases:
Clin Exp Dermatol. 2009 Dec;34(8):e640-2.
Treatment with carbamazepine and gabapentin of a patient with primary erythermalgia (erythromelalgia) identified to have a mutation in the SCN9A gene, encoding a voltage-gated sodium channel.
Natkunarajah J, Atherton D, Elmslie F, Mansour S, Mortimer P.
http://www.ncbi.nlm.nih.gov/pubmed/19549232
I did mention the use of mexilitine in children.
I did come across one case of genital erythermalgia:
Case Reports in Medicine Volume 2011 (2011), Article ID 374167, 3 pages
Erythema and Burning Pain in the Vulva: A Possible Phenotype of Erythromelalgia
Elisabeth Johnson, Priya Iyer, Alisa Eanes, and Denniz Zolnoun
free article here:
http://www.hindawi.com/crim/medicine/2011/374167/
They used a combination of clonazepam (a valium like drug) and a beta blocker blood pressure medication – check out the link
Another point that is quite important in her case, is whether there is any associatied arthritic joint pains and associated “connective tissue” complaints – dry mouth/eyes, swallow difficulties, rashes, and so on. This would suggest erythromelalgia is a secondary issue. Secondary erythromelalgia may respond to immunoglobulin infusions:
J Child Neurol 2012 27: 922 – 923
Secondary Erythromelalgia Successfully Treated With Intravenous Immunoglobulin
Shadé Moody, Susan Pacheco, Ian J. Butler and Mary Kay Koenig
http://jcn.sagepub.com/content/27/7/922.short
If you think your daughter has seconday Erythromelalgia let me know and I’ll send you the article.
Ganglion impar blocks have been used in vulvar conditons and in a child would be easy to reach if properly sedated. A dental needle injected through the sacrococcygeal joint would be all it would take.
They discuss ganglion impar blocks for vular conditions briefly here:
Journal of Sex & Marital Therapy, 30:125–139, 2004
Vulvar Vestibulitis Syndrome: A Clinical Approach
ALESSANDRA GRAZIOTTIN, LORI A. BROTTO
free article here:
http://www.obgyn.ubc.ca/SexualHealth/documents/Graziottin%20%26%20Brotto,%202004.pdf
The original protocol came from:
Graziottin A, Vincenti E. Anthalgic treatment of intractable pain due to vulvar vestibulitis syndrome: preliminary
results with oral gabapentin and anethetic block of ganglion impar (abstract). Proceedings of the Congress of the
international Society for the Study of Women’s Sexual Health (ISSWSH), Vancouver, october 10-14, pag 179, 2002
as reference here:
Graziottin A.
Dyspareunia: clinical approach in the perimenopause
in: Studd J. (Ed.), The management of the Menopause – Third Edition, The Parthenon Publishing Group, London, UK, 229-241, 2003
free article here:
http://www.fondazionegraziottin.org/ew/ew_articolo/1267%20-%20dyspareunia%20and%20perimenopause.pdf
More importantly, if ganglion impar block did give temporary relief, it is possible that longlasting relief could be achieved by botox injection to the ganglion impar. I have discussed this here:
New Treatment of Perineal / Pelvic Pain – Botox to Ganglion Impar
http://painmuse.org/?p=334
If your child’s pain is not well controlled, clinicians tend to go the extra mile to help them. There have been repeated instances of children been given 5-7 day regional or epidural block infusions with relative remission following:
Treatment of refractory primary erythromelalgia in a child using a continuous epidural infusion
Kaur Brar, Helen Baljit; El-Dabe, Sameh; Shehade, Suhail
The Pain Clinic, Volume 12, Number 1, 2000 , pp. 65-69(5)
abstract here:
http://www.ingentaconnect.com/content/maney/tpc/2000/00000012/00000001/art00011
The use of regional anaesthetic blockade in a child with recurrent erythromelalgia
C M Harrison, J M Goddard, C D Rittey
Arch Dis Child 2003;88:65–66
free article here:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1719300/pdf/v088p00065.pdf
This would require a good pediatric pain centre. There is a list of centres here:
http://www.apsoc.org.au/pdfs/fac_dir_paed_pain.pdf
Now, to get to someone who knows about erythromelalgia, you might what to contact the author of the Australian article – I know he’s a dentist but he must have got quite knowledgable about the condition and would know what pediatric specialist were helpful to him in his case.
Erythromelalgia presenting with premature exfoliation of primary teeth: a diagnostic dilemma.
Prabhu N, Alexander S, Wong P, Cameron A. abstract here:
http://www.ncbi.nlm.nih.gov/pubmed/23211921
the authors are here:
Department of Pediatric Dentistry, Westmead Hospital, Sydney, Australia.
and Dr. N. Prabhu’s email is given as:
neetaprabhu@hotmail.com
I will write him as well and ask advice.
I havew EM started a year ago, tried every drug get relief
My condition with EM is good, it has not gone away but has eased off
I wear thongs all the time, and do not walk very much.
My Dr, rang to tell me, I have abnormal blood, goung to see him today.
I hope it is going to be better news, than what is going thru my mind.
Hello, I have severe primary EM due to an SCN9a mutation. I applaud your efforts, but I’m begging you to remove the above mentions of cold water or ice water, ice, snow, etc., as these are all very dangerous for people with EM. It can cause nerve damage and can also cause the skin to break down, resulting in gangrene and amputation. A few other things:
1) While EM and PEPD are distinct, they can overlap. I suffer from both and have read a case study of another person with Primary EM who also has both.
2) Cipro and similar antibiotics have caused many cases of EM, and even in those with Primary EM, Cipro is often the trigger for the first attack.
3) Long-term Verapimil use has been reported as a cause of EM.
4) Please urge physicians to test for myeloproliferative diseases as soon as possible, and if none is found and no other cause can be found, continue to monitor for at least 2 years. EM can be a harbinger of impending myeloproliferative disease.
5) For those with severe EM like myself, the triggers can be much smaller than those listed. Some of us cannot stand up or even allow our legs to dangle without provoking a flare. Temperatures as low as 65 degrees can trigger flares. I could go on and on, but you get the idea.
6) Rather than being the opposite of Reynaud’s (although, descriptively that does make sense), EM has much in common with Reynaud’s in the sense of responding to temperatures in a dysfunctional way. This is important to point out because many EM sufferers also have Reynaud’s but have been told by doctors that they couldn’t possibly have both because they are opposite conditions. Not only is it possible to alternate between the two, it is possible to experience both at the same time, particularly because of our constant efforts to stay cool. This may manifest as one foot or hand having a Reynaud’s attack while the other has an EM flare, or it may manifest as a mosaic pattern. The EM patches will give off heat and right next to them, the Reynaud’s patches will feel frozen to an observer. This is exceptionally painful, in my experience.
7) Be careful not to conclude that a patient has Secondary EM solely because that patient also has a disease or syndrome that can cause EM. Those of is with Primary EM tend to have many other health problems as well, particularly rheumatological conditions. It is also clear that there are other genetic causes besides SCN9A mutations that are as yet unidentifed, because there are examples of familial EM in the absence of that mutation.
That’s all I can think of off the top of my head. Please feel free to contact me for further information, but be warned that it is difficult for me to respond in a timely manner! I am severely disabled by this condition and others.
I wish I could edit my above comment! I couldn’t read it as I was typing and now I see several things I’d like to correct. Oh well… I guess I can at least clarify one thing. In the beginning when I said, “It can cause nerve damage…,” of course I meant “They,” in reference to the preceding list, and also I should have said “over time.” EM patients can be desperate enough for relief to apply ice (or soak in ice water) for many hours every day. Many will do this even knowing the risks, sheerly out of desperation.
I skimmed the article again and I may have missed something, but I did not see any mention of topical treatments, so I’d like to mention that I am totally dependent on compounded topical medications, since nothing else has yet provided any relief. I currently use 15% Lidocaine ointment and Lidoderm patches. I have also used, with less success: 5x strength EMLA; Amitryptaline (can’t recall concentration); Ketamine; and Baclofen. (Baclofen did nothing.)
I also noticed aspirin was mentioned in the chart from the survey of treatment success. Aspirin generally provides relief only to those with myeloproliferative diseases, and the relief is generally marked. It usually helps those cases quite quickly, even within hours in some cases. Others take days before it begins to help.
Last thing: In the chart of tests recommended, it said no genetic testing was recommended for sporadic adult-onset cases. I am a sporadic adult-onset case with an SCN9A mutation and I know of one other. I’m certain we’ll find others if people like me were more able to access testing.
———
Thanks
admin
I would like to thank you for the efforts you’ve put in writing
this blog. I’m hoping to see the same high-grade blog posts
from you in the future as well. In truth, your creative writing abilities has motivated me to get my very own site now ;)