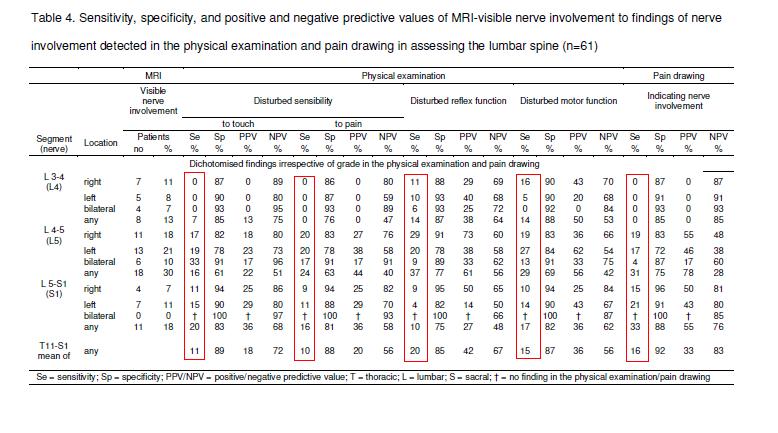
Radiculopathy (sciatica) cases were categorized by their pain diagrams and physical findings. Only 16- 37% of cases showed MRI findings. If there is an MRI-visible issues – only 22-78 % cases have symptoms (positive predictive values of MRI-visible nerve involvement). I can’t help but say it – Frankly, MRI’s suck in chronic radiculopathy. – The test that would be king – but fails badly. –
BMC Musculoskelet Disord. 2010 Sep 10;11(1):202.
Assessment of nerve involvement in the lumbar spine: agreement between magnetic resonance imaging, physical examination and pain drawing findings.
Bertilson BC, Brosjo E, Billing H, Strender LE. free article here
- 61 cases
- MRI studies for nerve root involvement
- Pain/numbness referral drawings
- numbness /weakness/reflex changes cataloged
As you can see from table, sensitivities related to various symptoms poor. they state with some astonishment that ” This means that at best 1 out of 5 and at worst 1 out of 10
patients with a physical examination finding indicating nerve involvement originating in the lumbar spine were considered as MRI-visible nerve involvement.”
- To compound this problem is the great faith put in MRI’s but some clinicians: “This means that for most patients, nerve involvement detected in a physical examination and/or pain drawing may go undetected if the clinician believes the MRI assessment of nerve involvement. This observation contrasts with the views of experts who suggest that the (greater) sensitivity of MRI in detecting spinal disorders can lead to potentially harmful clinical measures, for example surgery [6]. Roland et al. even suggest that a radiological report should include a caution to the effect that the clinician, and in the end the patient, should not worry about abnormalities seen on the MRI [17].”
Part of this is due to the natural history of chronic radiculopathy:
Spine (Phila Pa 1976). 2006 Jun 15;31(14):1605-12; discussion 1613.
Natural course of disc morphology in patients with sciatica: an MRI study using a standardized qualitative classification system.
Jensen TS, Albert HB, Soerensen JS, Manniche C, Leboeuf-Yde C. abstract here
J Manipulative Physiol Ther. 2007 Feb;30(2):98-108.
Magnetic resonance imaging findings as predictors of clinical outcome in patients with sciatica receiving active conservative treatment.
Jensen TS, Albert HB, Sorensen JS, Manniche C, Leboeuf-Yde C. abstract here
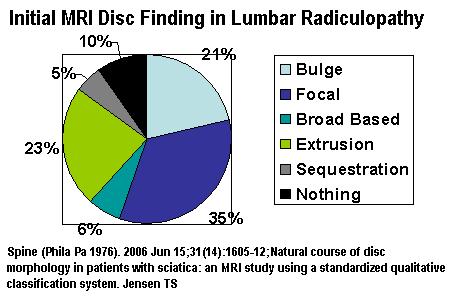
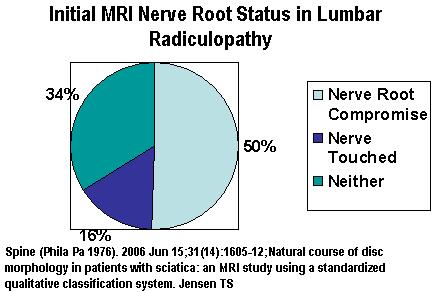
- 154 cases of lumbar radiculoppathy MRI followed for 14 months
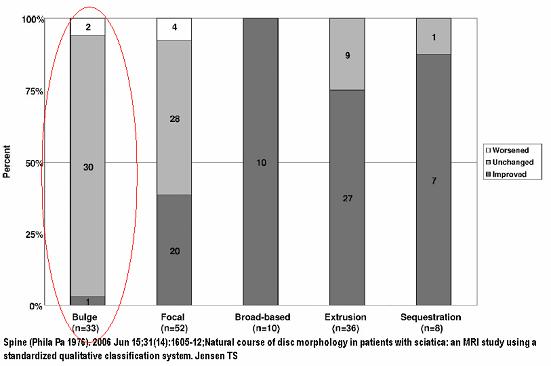
- Initially, 1/5 of radiculpathy shows only disc bulges:
- Initially, 1/3 of cases will show no touching, compression or displacement of nerve root:
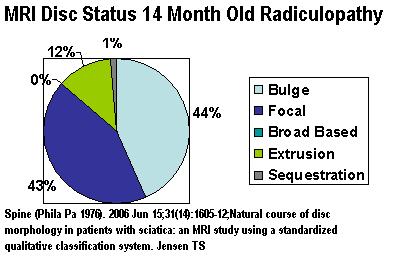
- 14 months later, 90% still symptomatic – though 52% improved. Of those worse or not improved – 1/2 will be disc bulges only:
- Disc bulge radiculopathy rarely gets better (1/33 better only)
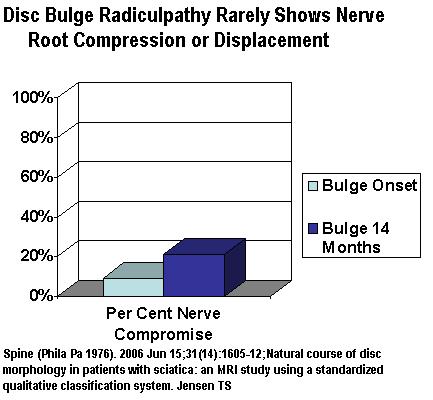
- Unusual for Bulging discs to show compression or displacement of nerve root so may not be able to be differentiated from the 78% of bulging discs that are asymptomatic
- Hence ultimate curse – have a bulging disc sciatica – unlikely to show nerve root involvement so will not be believed but also unlikely to get better. Women are more likely to get bulging disc sciaticas.
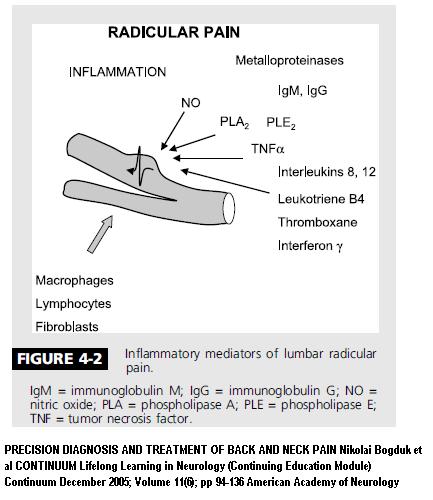
- Even worse was the 10% of chronic sciatica cases that shows no disc or nerve abnormalities at all. It is now understood that internal disc disruptions will cause heavy production of inflammatory chemicals that can cause typical sciatica –
- These chemical by themselves can cause radiating pain, numbness, muscle strength changes and reflex changes with Normal MRI – It was named “Chemical Radiculopathy”
Pain Physician, Volume 5, Number 3, pp 260-265
Clinical Evidence of Chemical Radiculopathy
Curtis W. Slipman, MD*, Zacharia Isaac, MD**, David A. Lenrow, MD#, Larry H. Chou,
Russel V. Gilchrist, DO♦ and Edward J. Vresilovic, MD, PhD♣ free article here
Joint Bone Spine. 2006 Mar;73(2):151-8. Epub 2005 Jun 22.
Pathophysiology of disk-related sciatica. I.–Evidence supporting a chemical component.
Mulleman D, Mammou S, Griffoul I, Watier H, Goupille P. abstract here
This issue got a boost from the 2006 article presenting 42 cases of chemical radiculitis. The found an internal “annular tear” might be the source of the inflammation, and the side of the disc torn corresponded to the side the sciatica was on:
Pain. 2007 Jan;127(1-2):11-6. Epub 2006 Sep 8.
Chemical radiculitis.
Peng B, Wu W, Li Z, Guo J, Wang X. abstract here
Abstract: The theory of chemical radiculitis had been put forward about 30 years ago, but
as yet it has not been proved by clinical studies. The aim of the current studies
was to determine whether the annular tear of a painful disc proved by discography
is the cause of radiating leg pain (radiculopathy) in patients with discogenic
low back pain. Forty-two patients with discogenic low back pain at single disc
level with concomitant radiating leg pain were studied in order to analyse the
relationship between site of annular tear and side of radiating leg pain.
Electromyogram and motor nerve conduction velocity were monitored to examine nerve root injury. The current studies found that there was a significant positive correlation between the site of annular tear and the side of radiation pain. Abnormalities of electromyogram and reduction of motor nerve conduction velocity were found on the side of radiating leg pain. The studies indicated that leakage of chemical mediators or inflammatory cytokines, which are produced in the painful disc, into epidural space through annular tear could lead to injury to adjacent nerve roots, and it might constitute the primary pathophysiologic mechanism of radiating leg pain in patients with discogenic low back pain but with no disc herniation.”
The BMC Musculoskelet Disord top study presents a plea for sufferers:
“many patients with “MRI-invisible” lumbar symptoms need treatment aimed at nerve involvement”
My plea would be that they are believed despite only a bulge or despite nothing because MRI are frankly just not any good.
To make the situation worse is the neck:
- First of all, the text-book radiation patterns of neck radiculitis are bogus. A Key point make in Bogduk’s educational article for neurologists is this:
“KEY POINT: A Cervical radicular pain does not follow dermatomes. Its pattern may be difficult to distinguish from somatic referred pain.”
Secondly, Findings on MRI do not correspond to the disability pain or recovery of the whiplash injured (excluding fractures and dislocations):
Eur Spine J. 2008 Aug;17(8):996-1005. Epub 2008 May 30.
Are early MRI findings correlated with long-lasting symptoms following whiplash
injury? A prospective trial with 1-year follow-up.
Kongsted A, Sorensen JS, Andersen H, Keseler B, Jensen TS, Bendix T. free article here
“Trauma-related MRI findings are rare in a whiplash population screened for serious injuries in the emergency unit and not related to a specific symptomatology. Also,
pre-existing degeneration is not associated with prognosis.”
In:
Arch Phys Med Rehabil 2007; 88: E64
Correlation of Clinical Findings, Electrodiagnosis, and Magnetic Resonance Imaging Study in Cervical Roots Lesion.
Seyedmansoor Rayegani, MD
- For neck – clinical and MRI correlation was only 52% (Flip a coin).
- Specific neck nerve root electrodiagnostic correlation with MRI was only 45% (worse than the coin flip). – oh brother.
- felt C6 most affected and best muscles to test were: deltoid (C5), pronator teres (C6), triceps brachii (C7), and abductor pollicis brevis (APB) (C8) muscles
In the top BMC Musculoskelet Disord article they comment on how pathetic it is for patients to put their faith in MRI’s:
“Such suggestions may explain why patients with back pain generally have very high expectations of the diagnostic value of MRI, at least believing that it will not fail to find the explanation for their discomfort, and therefore desire to have a scan. In our patient sample, 100% believed the MRI would (finally) provide the explanation for their discomfort, which for the median patient had started 14 years earlier and had plagued them to the extent that 85% desired back surgery after having been through years of conservative treatment.”
They also point out how these poor chronic radiculopathy cases are labelled “nuts” and treated accordingly:
[In chronic radiculopathy] “about half of these patients – and the referring clinicians – in the end received radiological reports that showed no visible nerve involvement. In accordance with clinical practice, this usually means that the patient’s discomfort is labelled “non-specific” and therefore continues to receive conservative treatment and/or is referred for psychosocial treatment strategies.”
I have heard of cases successfully treated with steroid epidural blocks told, because their recent MRI only showed a bulging disc, they could no longer benefit from the shots…
This is a sad, sick, world brought on by the arrogance of a medical profession in their “MRI GOD”
I hope the next generation of doctors are taught better…
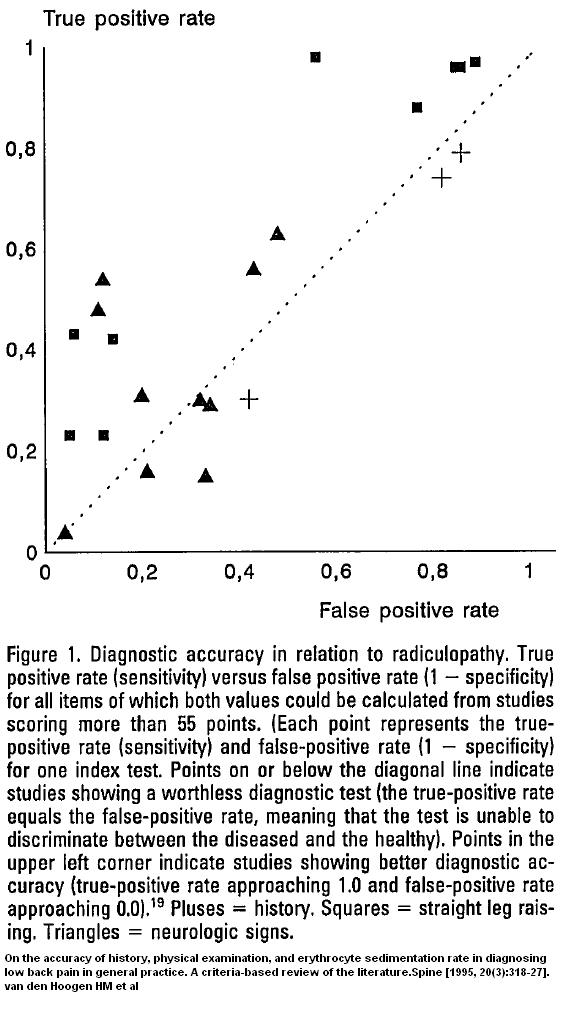
Addendum – even more damning is a review of how history and physical findings may not be much better than chance at determining ALL radiculopathy in general:
On the accuracy of history, physical examination, and erythrocyte sedimentation rate in diagnosing low back pain in general practice. A criteria-based review of the literature.
Spine [1995, 20(3):318-27].
van den Hoogen HM et al abstract here
Dotted line shows where test no better than chance –
– certainly history (the “+”) – no help;
– neurologic signs (Triangles) – some few studies not bad – most no help;
– straight leg raises (Squares) – better than nothing but can miss alot
From the looks of this top article, if MRI’s were included, “could miss alot” would be the result in chronic radiculopathy.
This article could use comments please.

I have this very problem and the doctors rely on the MRI to treat me, so far my pain has gotten worse and nothing works. Thanks for this info.
Have recently been diagnosed with chemical radiculopathy. Surgery 2/2010 L5S1. Large piece of disc broke off this large disc. No relief since injury. This info is helpful and know now am not nuts. Positive emg findings. Third MRI shows bulges, tears and rerupture. Pain increasing. Any treatment helpful for this condition other than pain meds?
Great assessment of this study. I find many patients with minimal or no MRI correlation often are the most difficult to treat. I’d suggest looking into the use of super pulsed laser therapy for those looking to an alternative solution to their pain.