I have published on the use of ketamine to treat pain/depression/suicidality. Now a weak painkiller / partial painkiller blocker has been shown to help depression, not with one study, but with findings from twelve studies.
Stanciu, Cornel N., Oliver M. Glass, and Thomas M. Penders.
Use of buprenorphine in treatment of refractory depression—a review of current literature.
Asian journal of psychiatry 26 (2017): 94
https://www.ncbi.nlm.nih.gov/pubmed/28483102
- being only a partial stimulator, it has a ceiling effect – maxing out so taking more does no good and hence avoiding much misuse.-despite being 30 to 40 times more potent than morphine
- because it blocks Kappa receptors, there is “marked and less delayed withdrawal effects.”
Blocking kappa receptors has been found to bring back motivation in pain:
Blunting pain’s emotional component https://source.wustl.edu/2019/03/blunting-pains-emotional-component/
I will comment on the studies but not with opioid addicted subjects:
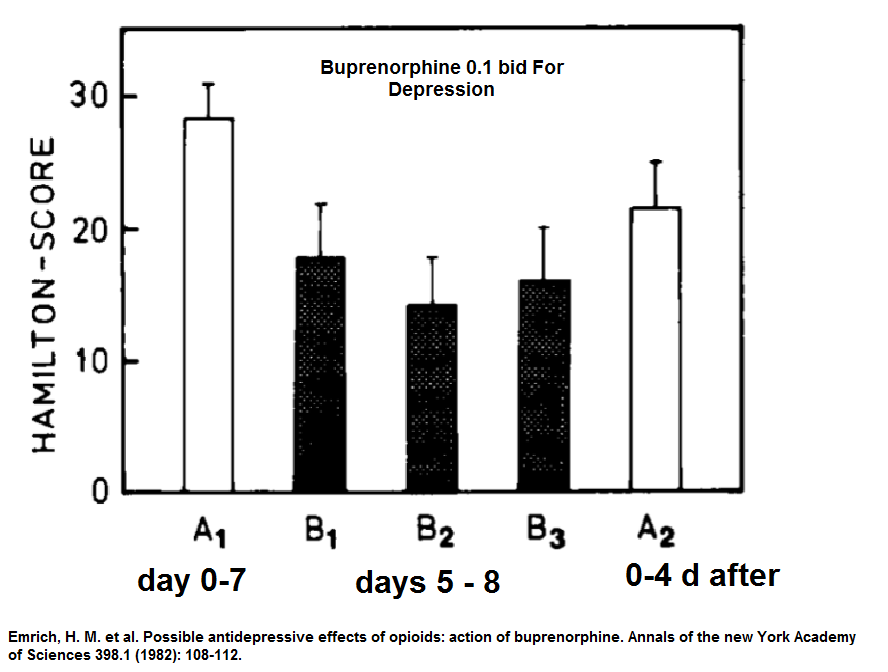
first study 1982
Emrich, H. M., P. Vogt, and A. Herz.
Possible antidepressive effects of opioids: action of buprenorphine.
Annals of the new York Academy of Sciences 398.1 (1982): 108-112.
https://nyaspubs.onlinelibrary.wiley.com/doi/full/10.1111/j.1749-6632.1982.tb39483.x
- 13 cases treated for 5-8 days
- BUP 0.1 mg twice daily
- depressed cases not on any other meds
- 50% responded very strongly while other half were non-responders
- slight nausea, dizziness, sedation
in 1995:
Buprenorphine Treatment of Refractory Depression
J. Alexander Bodkin, MD, Gwen L. Zornberg, MD, Scott E. Lukas, PhD,
and Jonathan O. Cole, MD.
Journal of Clinical Psychopharmacology, 1995,15,pp.49-‐57
https://www.researchgate.net/profile/J_Bodkin/publication/15485413_Buprenorphine_Treatment_of_Refractory_Depression/links/5746ef7d08ae9f741b452433.pdf
- 10 cases unipolar depression for 4-6 weeks
- treatment refractory cases
used average of 1.3 mg/day though in opioid abusers was 2-18 mg/day
noted rapid onset – most within 1 week
did not feel intoxicated or euphoric – just “more normal”
1/3 felt it was unpleasant and stopped taking it, while another 1/3 stopped at 4 weeks despite fact it helped
responders got “marked response” suggested tho them some abnormality of endogenous opioid system
referenced a study finding ninefold increase in opioid receptors in suicide victims.
“This finding may suggest that opioid receptor up-‐regulation may be occurring in this very treatment refractory population because of a deficit of endogenous opioid neurotransmitter availability”.
Gross-‐Isseroff R, Dillon KA, Israli M, Biegon A. Regionally selective increases in opioid receptor density in the brains of suicide victims. Brain Res 1990;530:312-‐6.
A commentary a year later
Biological Psychiatry 15 June 1996, 39(12), 989-1096
Buprenorphine for depression: The un-adoptable orphan
Enoch Callaway
bemoans the fact no one has run with the fact that the agent can quickly remit depression “most patients… within hours”. They had 5 cases that were followed for several years with maintained good results. They found any lethargy from the pill responded to methylphenidate or dexedrine.
No one picked up on it and it remained an orphan…
Most interesting, was a letter, using it in ECT refractory cases:
Nyhuis, Peter W. et al (from Germany)
Opiate treatment in depression refractory to antidepressants and electroconvulsive therapy.
Journal of clinical psychopharmacology 28.5 (2008): 593-595.
https://www.ncbi.nlm.nih.gov/pubmed/18794671
(letter – no abstract)
- States ECT works 50-75% of cases.
- “this leaves a percentage of 10%-20% of patients who are unresponsive to medication and ECT treatment”
- 4 women, 2 men with nonpsychotic major depressive episode
- Everything tried including inpatient and 11-14 ECT treatments
- began buprenorphine with 0.4 mg/day – increased every 1-2 days until 0.8-2.0 mg/day
Results are literally amazing:
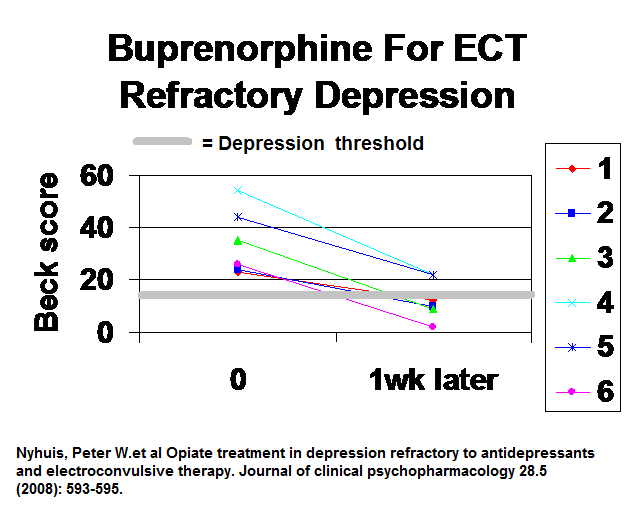 Within 1 week, 4/6 were below depression threshold
Within 1 week, 4/6 were below depression threshold
side effects included nausea, constipation, sedation, dizziness and sweating but not bad enough for any to stop treatment. – they felt they were mild, dose dependent and transient.
Given that doses used for pain went up to 16 mg, that the dose was trivial.
suggested that “a specific role of the endogenous opioid system” in a subgroup of patients.
They called it ,with tongue in cheek I suspect, “the Bopium cure”
In the last few years some real studies have been done:
Karp, Jordan F., et al.
Safety, tolerability, and clinical effect of low-dose buprenorphine for treatment-resistant depression in mid-life and older adults.
The Journal of clinical psychiatry 75.8 (2014): e785.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4157317/pdf/nihms609147.pdf
- age 60 and older
- 15 subjects over 8 weeks
- Temgesic (0.2 mg sublingual tablets)0.2 mg-1.6 mg/day. ( again a very small dose)
-
“For the first week, subjects took 0.2 mg/day, usually in the morning.”
- increases of 0.2 mg at a time depending on side effects
- at 8 weeks drug was stopped by “decreasing the dose about 20% every 2–3 days”
- average dose was 0.4/day and max 1.6/day
Results: using Montgomery Asberg Depression Rating Scale (MADRS)
(<7 no; 7-19 mild; 20-34 moderate)
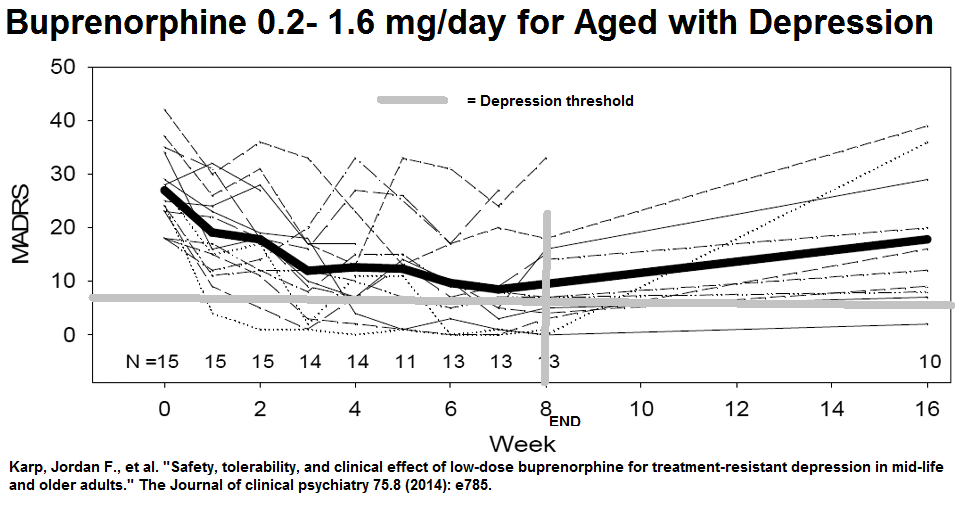 So started out with moderate and ended with mild but evidence of rebound some once off meds. They felt “the antidepressant benefits of low-dose buprenorphine may require long-term dosing to be sustained.”
So started out with moderate and ended with mild but evidence of rebound some once off meds. They felt “the antidepressant benefits of low-dose buprenorphine may require long-term dosing to be sustained.”
- mental functioning was not affected “buprenorphine has been shown to have a neutral effect on cognition “
- safe, well tolerated; no weight gain during
- Constipation and nausea were side effects but not bad
- dependence issue was not “clinically significant”
Recently:
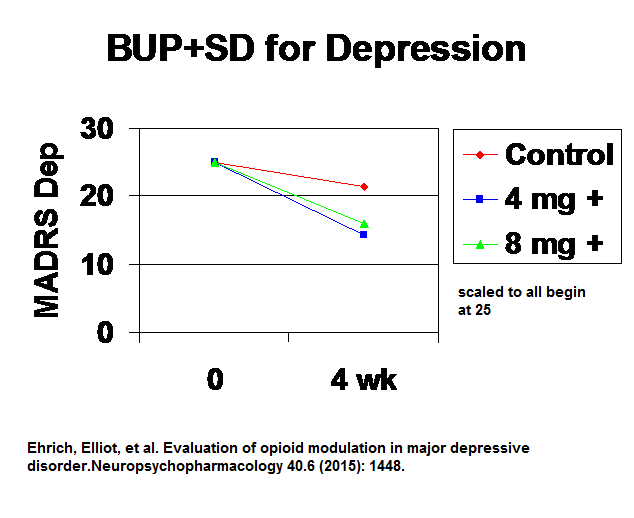
Ehrich, Elliot, et al.
Evaluation of opioid modulation in major depressive disorder.
Neuropsychopharmacology 40.6 (2015): 1448.
https://www.nature.com/articles/npp2014330.pdf
- This study went to major efforts to avoid opioid “high” physiological effects by adding an opioid antagonist that is absorbed easily through the skin called samidorphan (SAM)
- they had groups: – but only 1 week study
– control (first one!)
– 4 mg
– 8 mg
Results:
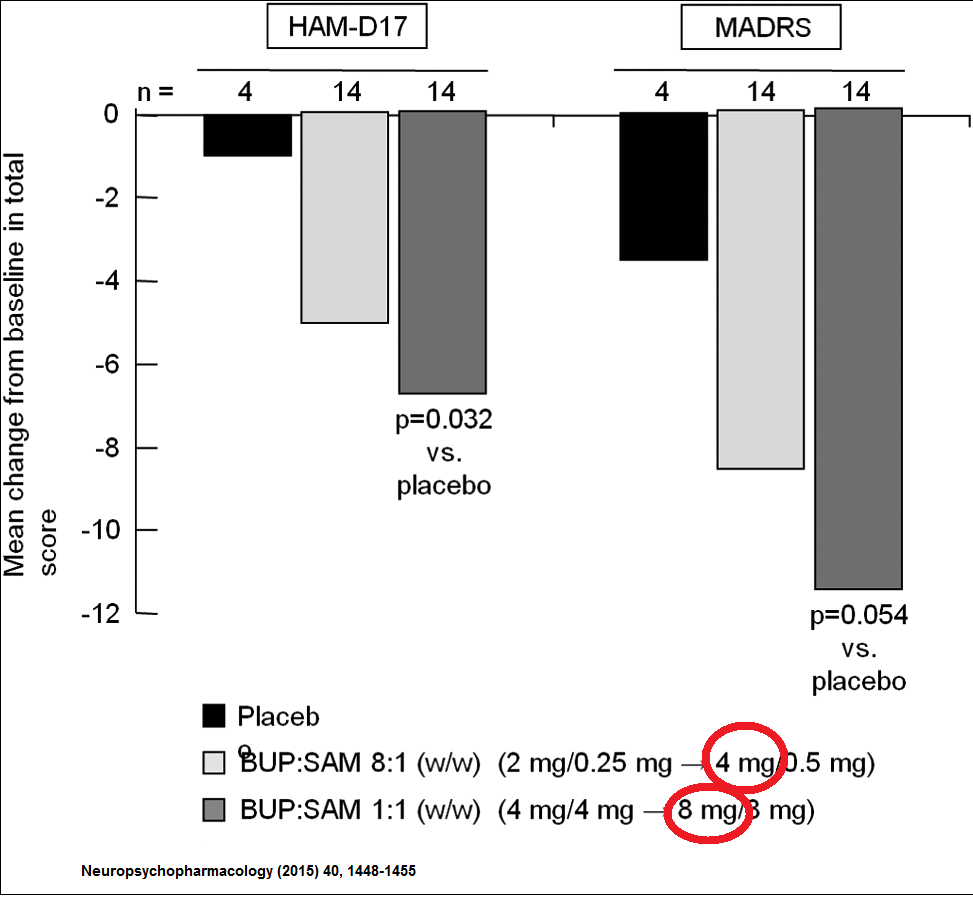 However if you proportion results at 25 and scale them down % wise for each it looks different. – They both dropped the same percent – the 8 mg was more down because they started out bit more depressed. So not convinced 4 mg+ was better than 8 mg+.
However if you proportion results at 25 and scale them down % wise for each it looks different. – They both dropped the same percent – the 8 mg was more down because they started out bit more depressed. So not convinced 4 mg+ was better than 8 mg+.
 If you look at previous study using MADRS depression scale, you see pain scale continued down to 10 by week 7 – just 3 above 7 = no depression
If you look at previous study using MADRS depression scale, you see pain scale continued down to 10 by week 7 – just 3 above 7 = no depression
Fava, Maurizio, et al.
Opioid modulation with buprenorphine/samidorphan as adjunctive treatment for inadequate response to antidepressants: a randomized double-blind placebo-controlled trial.
American Journal of Psychiatry 173.5 (2016): 499-508.
https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2015.15070921
- “Imaging studies have revealed alterations in opioid transmission associated with induced sadness, social rejection, and depression in key brain emotional regulatory centers, including the nucleus accumbens, ventral pallidum, amygdala, anterior cingulate cortex, and posterior thalamus.
- They’ve know for some time that there is an endophin deficiency state in suicidal patients
- the opioid antagonist samidorphan has no effect on depression so results in combo would be from buprenorphine. This I believe was a mistake and blunted to opioid effects.
- “Endogenous opioid dysregulation” as a factor in chronic depression
- Used 2 or 8 mg plus samidorphan
Did a fancy technique to remove placebo responders and came out with this using MADRS depression scale (<7 no depression; 7-19 mild; 20-34 moderate)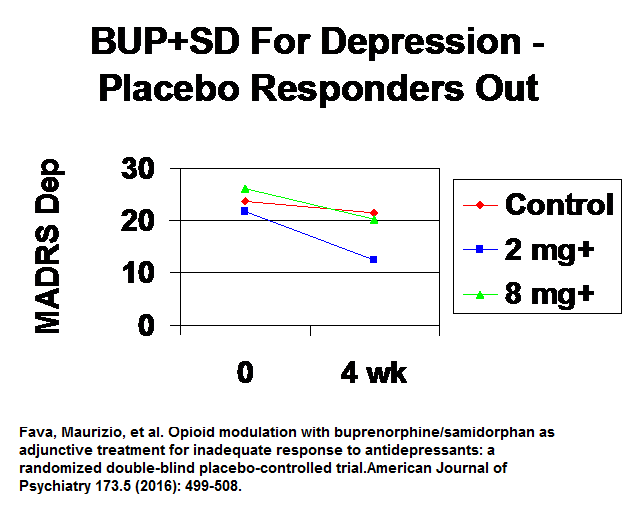 This suggested the lower dose was better – started out moderate and ended up mild.
This suggested the lower dose was better – started out moderate and ended up mild.
They found ” this compares favorably with results from a meta-analysis of 14 studies with atypical antipsychotics as adjunctive therapy for major depression”. – a viable treatment option then.
side effects were nausea, vomiting, and dizziness – which would be worse in the 8 mg+ group and might have blunted its efficacy. These side effects were worse the first few days and one wonders if an anti-emetic should be used initially until people get used to them after day 3.
Lastly was a dud of a study using mini-doses of BUP
Yovell, Yoram, et al.
Ultra-low-dose buprenorphine as a time-limited treatment for severe suicidal ideation: a randomized controlled trial.
American journal of psychiatry 173.5 (2015): 491-498.
https://ajp.psychiatryonline.org/doi/pdf/10.1176/appi.ajp.2015.15040535
“beginning with 0.1 or 0.2 mg/day. Once a week, at the decision of the study psychiatrists, the daily dose could be raised in 0.1 – 0.2 mg increments, to a maximal daily dose of 0.8 mg.”
No effect on depression but did find that suicidality decreased significantly in BUP group.
Comments – this was one of the most arduous efforts I have had to do. Studies with poor results overplayed their stats and made articles unreadable. However, some things do stand out:
- They probably work as well as atypical anti-psychotics to augment antidepressants
- Might be able to tell if it is going to work because response can be apparent within hours – so responder selection by early response might cut unnecessary costs
- In an opioid naive patient 2 mg/day might work but suspect best used twice daily rather than od(once daily) as many of the studies liked to do.
- adding a opioid blocker to BUP may be suboptimal – one can use all the help one can get. Having said that, those without the blocker are likely to have more rebound depression once off the drug and so more long-term use might be needed. ? 16 wks? I have a major problem with using ketamine in pain patients with depression. I have not sure re any long-term benefits with ketamine as I use it. Unless they undergo behavioural activation and CBT mobilization during periods they feel better, less long-term might happen.
- Use in suicidal patients is noteworthy and suspect they include a subgroup more likely to respond to BUP – but may need to work up to 2 mg+/day
- Articles did mention borderline personality cases more likely to respond.
- I suspect its use in ECT failures was not by itself, but was augmenting effect of ECT therapy (like enbrel worked best in cases that had “failed steroid epidural” just prior).
- in Canada, an oral – through-the gum-absorbed dose has recently become available. It is called Belbuca. Its monogram is here:
http://purdue.ca/wp-content/uploads/2018/02/Belbuca-PM-EN.pdf
comes in:
0.075 mg
0.150 mg
0.3 mg
0.450 mgsounds like one could start with 0.45 mg/day and work up to 4/day =1.8 mg. Each tablet according to a recent handout I was given costs $4.20/each. With 4/day would be 16.80/day or $504.00/30 days – - Suboxone (buprenorphine + naloxone) is used in addicted cases similarly to methadone. Its restrictions have been reduced recently in Canada:
http://www.cbc.ca/news/canada/toronto/suboxone-announcement-1.3801321 - BuTrans Patch is a once weekly form ideal for use once steady state achieved. Skin irritation is common.
5 mg = 0.2 mg /day
10 mg = 0.4 mg/day
20 mg = 0.8 mg /day
30 mg = 1.2 mg /day
40 mg = 1.6 mg /day
I start with 10 mg (5 in elderly) and work up. Had trouble with 20 mg in one elderly.
Expensive but once/week use is tantalizing. - Have to definitely try in ECT failure cases.
NOTE – PHARMACY HAS MADE IT CLEAR BELBUCA NEEDS TO BE STARTED AT THE LOWEST DOSE – 0.075 MG OD AND ONLY WORK UP AFTER 4 DAYS.
addendum – had a case with severe depression age 65. Already on large doses venlafaxine. Has some chronic pain issues but not wanted painkillers. Has drug coverage so started butrans 10 1/wk (equivalent to 0.4 mg/day). After 1 week is beck 14 = borderline so am impressed. He changes patch slightly before 1 week because pains start coming back. Plan would be to keep on butrans 10 as near zero addiction potential and less pain probably helps quality of life – there is some recurrence of depression at 20 wks if stopped at 12. He was obviously a responder and he noted effects within 1 day. Good responders like that are maybe 1/3 cases.
Any experiences would be appreciated.

ola maria. tenho depressão pos parto e estava tomando esc durante o dia e clonazepam para dormir a noite, estava me dando bem com o esc. porem quando voltei a trabalhar comecei a desregular o remedio e tive recaida, minha irma sisma q mesmo com o esc eu durmo muito durante o dia, ele me da um certo sono depois q acabo de tomar ele. ai a dra falou pra tomar o esc durante a noite e de manha tomar o bup pra ver se me levanta. mas to com medo de começar a tomar o bup e nao me dar bem como estavame dando com o esc. vc sentiu diferença?? qual foi o melhor no seu caso e pq?
Hello Maria. I have depression after childbirth and was taking ESC during the day and clonazepam to sleep at night, I was getting on well with ESC. but when I went back to work I began to deregulate the remedy and I had a relapse, my sister even if with the esc I sleep a lot during the day, it gives me a certain sleep after I have just taken it. Oh, the doctor told me to take the esc at night and in the morning take the bup to see if I get up. but I’m afraid to start taking the bup and it does not give me good as it was giving me with esc. Did you feel any difference ?? What was the best in your case and why?
Maria,
It would take probably 2 week to work up to near 2 mg buprenorphine/day. Once at that dose, you should notice some benefits within days. If not, maybe forget it.