Although the question of whether one is dealing with hip bursitis or is this referred from back is important, I wanted to clarify what steroid injection would do for seemingly glutues medius bursitis. One study suggests it was good in 72% of cases at one month while another suggested it was good up to 6 weeks. Thereafter however, is problematic with PRP injection outshining it after 6 weeks. Problem is and I quote “an isolated passive intervention cannot hope to address the often complex mix of pre-existing and subsequent impairments”.
Labrosse JM, Cardinal E, Leduc BE, et al. Effectiveness of ultrasound-guided corticosteroid injection for the treatment of gluteus medius tendinopathy.
AJR Am J Roentgenol . 2010;194(1):202-206
- 54 cases mostly women average age 55
Technique:
- “a 22-gauge spinal needle fixed to a 10-mL syringe filled with 2% lidocaine (Xylocaine, AstraZeneca) was inserted via an anterior approach.
- Using continuous ultrasound real-time monitoring, the operator progressively advanced the needle while intermittently injecting a small amount of lidocaine. This injection technique allowed deeper local anesthesia to be obtained and also helped to localize the tip of the needle by mobilizing surrounding tissue.
- The fascia lata was traversed with the needle, and its tip was positioned at the surface of the lateral part of the distal gluteus medius tendon .
- Approximately 1 mL of lidocaine was injected with peritendinous fluid pooling to confirm proper needle positioning. A peritendinous cortisone injection(30 mg of triamcinolone and 3 mL of bupivacaine 0.5%) was then performed under continuous ultrasound monitoring.”
Results: – 72% had some relief with pain dropping from 7.4/10 to 2.9/10 at 4 weeks
Comment – 30 mg triamcinolone is not much for such a big tendon which leads me to wonder if a repeat of 30 mg should be done at 6 weeks
Fitzpatrick, Jane, et al.
The Effectiveness of Platelet-Rich Plasma Injections in Gluteal Tendinopathy: A Randomized, Double-Blind Controlled Trial Comparing a Single Platelet-Rich Plasma Injection With a Single Corticosteroid Injection.
The American journal of sports medicine (2017): 0363546517745525.
http://journals.sagepub.com/doi/abs/10.1177/0363546517745525
- average age 60 with male: female 1:9
- 37 cases for corticosteroid and 39 for Platelet Rich Plasma (76)
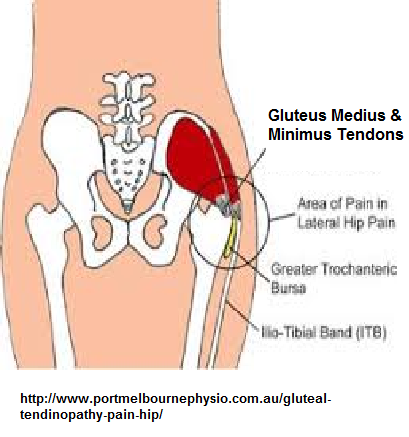
- pain lateral hip including greater trochanter
- 21/76 = 27% cases altogether had partial gluteal tears; full thickness ones were excluded from study
Techniques:
- “6 to 7 mL of trial substance (PRP or corticosteroid) was injected into the affected area of the tendon in 5 to 6 passes using ultrasound guidance”
- I had to write the author to get exact dosages but it looks like Celestone Chronodose Injection 1 ml (which contains betamethasone 5.7 mg, as betamethasone sodium phosphate 3.9 mg (in solution ) and betamethasone acetate 3 mg (in suspension) in an aqueous vehicle) – seems equivalent to 40 mg triamcinolone ( my favorite)
- PRP was made from 55 ml blood – though that much blood was drawn from both to maintain double blind.
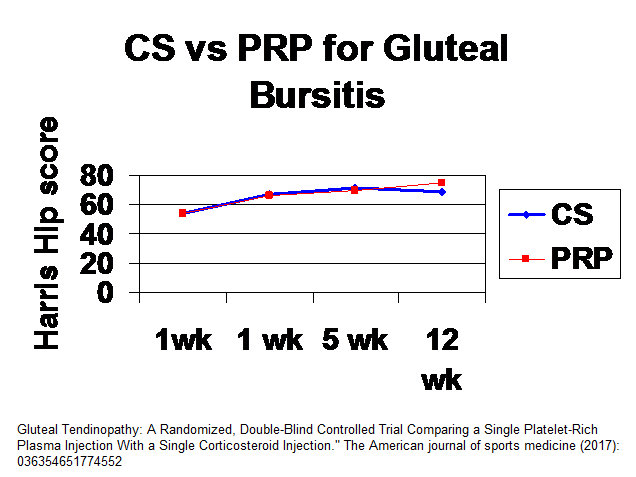
Results – they used some composite score (Harris hip score which I cannot quantify properly. but did find steriods gave benefit for 5 weeks but PRP bit better thereafter (higher the better)
At present there is great confusion over what involves proper treatment:
Grimaldi, Alison
Conservative management of lateral hip pain: the future holds promise.
Br J Sports Med January 2017; 51 (2) (2017): 72-73
http://mobile.dl.yums.ac.ir/bitstream/Hannan/188973/1/2017%20Sports%20Medicine%20%2817%29.pdf
- extracorporeal shockwave therapy (ESWT) – no help
- “Active intervention is recommended in the management of tendinopathy; however, the only published clinical trial investigating the effects of home exercise on GTPS reported disheartening results. Early outcomes were poor and patients only gained promising success rates at 15 months”.
- A trial called LEAP (load management and exercise program) is underway and there are big hopes it will offer some guidance:
Mellor, Rebecca, et al.
Exercise and load modification versus corticosteroid injection versus ‘wait and see’for persistent gluteus medius/minimus tendinopathy (the LEAP trial): a protocol for a randomised clinical trial.
BMC musculoskeletal disorders 17.1 (2016): 196.
https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-016-1043-6
Comment – gluteal weakness is common; partial tears at 27% and input from back plus with active trigger points in gluteal muscles combine to make this a near no win scenario but I do think working trigger knots , the back and maybe repeat injection at 6 weeks (or PRP instead) could make the difference.
A clean up of bursa and perhaps repair gluteal tendons has been tried endoscopically with benefit:
Coulomb, R., et al.
Clinical results of endoscopic treatment without repair for partial thickness gluteal tears. Orthopaedics & Traumatology: Surgery & Research 102.3 (2016): 391-395.
https://www.sciencedirect.com/science/article/pii/S1877056816000487
- 16 women 1 man average age 53.5
Technique verbatum:
- “Subcutaneous dissection was performed carefully to spare the sensory branches of the lateral cutaneous nerve of the thigh.
- A trocar was introduced in a posterior direction towards the space between the iliotibial band and the greater trochanter. Sweeping movements were used to palpate the contours of the greater trochanter. A 70° scope was aimed distally to locate the vastus ridge of the vastus lateralis and the trochanteric bursa.
- An accessory lateral instrument portal was made distal to the tip of the greater trochanter, after being located with a needle over the quadrate tubercle of the vastus lateralis.
- The appearance of the bursa was evaluated, and then it was resected using a radiofrequency probe and shaver.
- The gluteal medius and minimus muscles were evaluated after the proximal bursectomy. A probe was used to confirm that the enthesis was not completely torn. Treatment of the PTGT consisted of carding along the direction of the abductor fibres using a scalpel and making microperforations in the enthesis with a 1/18 K-wire (Figs. 3 and 4). These procedures were carried out through an anterolateral pretrochanteric approach; the greater trochanter was rotated as needed to complete the procedure from front to back.
- A calcification was removed in two patients with calcifying tendinopathy.
- In the three patients with hip snapping, a diamond-shaped endoscopic decompression of the iliotibial band was performed using the technique described by Ilizaliturri and Camacho-Galindo.
- The incisions were closed with interrupted sutures. Dry dressings were used to cover the surgical wounds. The patients were discharged from the clinic on the day after the procedure.
- The patients were required to use two crutches for 6 weeks to unload the hip joint”
Results:
- pain dropped from 7.2 to 3.3
- Harrisan hip score went from 53.5 to 79.8 – a 26.3 difference which they called modest so I don’t know what the 6 point spread between PRP and CS results in prior article would be called…