A Canadian study on full thickness tears found the no-op subgroup did well over 5 years. A Netheraland study found removing bursa (B) and taking off acromium(A) not any better than just removing bursa alone in chronic subacromial shoulder pain. Tear progression was not statistically different though at trend for A+B. Both suffer from not examining the patient subsequently to see what troubles they did actually have. British study found no clinically relevant benefits to Arthroscopic sub-acromial decompression
What happens to patients when we do not repair their cuff tears? Five-year rotator cuff quality-of-life index outcomes following nonoperative treatment of patients with full-thickness rotator cuff tears
Richard S. Boorman et al
J Shoulder Elbow Surg (2018) 27, 444–448
www.jshoulderelbow.org/article/S1058-2746(17)30669-9/abstract
-
Age of 40 to 85 years;
- ended up with 63 cases with 17 ops and 46 non-ops
-
Symptoms for 3 months or more
-
Full-thickness tear of supraspinatus or infraspinatus
Excluded the following:
- complete tears of subscapularis and/or teres minor
-
“Concomitant pathology of the affected shoulder (eg, instabil-ity, high-riding humeral head indicating cuff tear arthropathy,or osteoarthritis)”
-
“Substantial cervical spine pathology and/or radiculopathy”
- excluded WCB cases (this might limit cases to those who don’t need to use arm at work some)
contacted by phone/email
- half were traumatic other half insidious
- 72% dominant side
- No difference in Quality of life between those that did and didn’t have surgery
Comment – those who needed strength for work were WCB excluded. Those that had continued pain/problems went for surgery. There is a subgroup 46/63 = 73% that can co-exist with tears if it is an isolated problem in the shoulder. They mentioned one case that did well until he did something wrong with a golf swing and then ended up with surgery. Seems to suggest that subgroup that did well may also have to lie low and not stir things up in shoulder as well. My work is not physically demanding and I would probably take the lie low alternative.
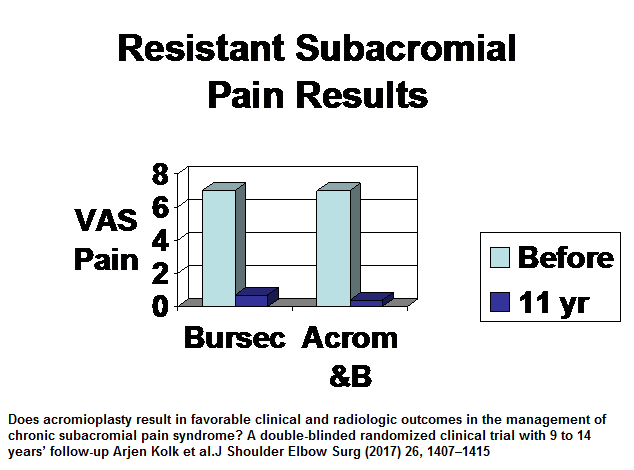
Does acromioplasty result in favorable clinical and radiologic outcomes in the management of chronic subacromial pain syndrome? A double-blinded randomized clinical trial with 9 to 14 years’ follow-up
Arjen Kolk et al.
J Shoulder Elbow Surg (2017) 26, 1407–1415
http://www.jshoulderelbow.org/article/S1058-2746(17)30188-X/fulltext
- mean age 44 (B), 50 (A+B)
- bursectomy 20; bursectomy and acromioplasty 23 – 43 patients
- 12 years followup
- They did procedure arthroscopically and were able to preserve anterior deltoid which could have helped results. Portals – posterior , lateral portal, and anterior.
- Procedure: – “First, the subacromial bursa was debrided with a motorized shaver or an electrocautery probe (OPES; Arthrex, Naples, FL, USA). When the patient was allocated to the acromioplasty group, a motorized burr was used to conduct a partial resection of the anteroinferior surface of the acromion and the distal coracoacromial ligament through the lateral and posterior portals until a flat surface was created.”
Results
- They found full thickness tears showed up in 17% of bursectomy and 10% of acromioplasty and bursectomy but this was not significantly different.
Comment – a letter complained they were underpowered to show significant differences that would have showed up if they had more patients but authors didn’t think so. I am impressed on results either way and wonder if there would be less full thickness tears with A+B
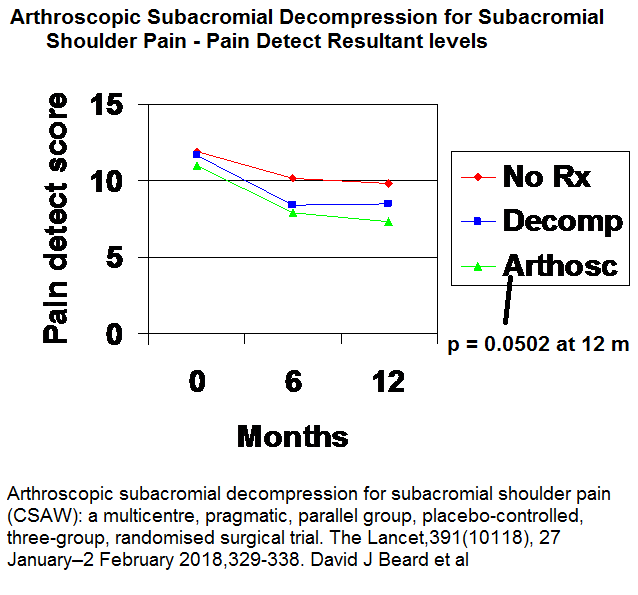
Beard, David J., et al.
Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial.
Lancet Volume 391(10118), 27 January–2 February 2018, 329-338
https://www.sciencedirect.com/science/article/pii/S0140673617324571\
- 90 patients – decompression
94 – arthroscopy
90 – no treatment
Results – showed some statistical improvement which was so little it was not clinically significant.
Pain:
Quality of Life:
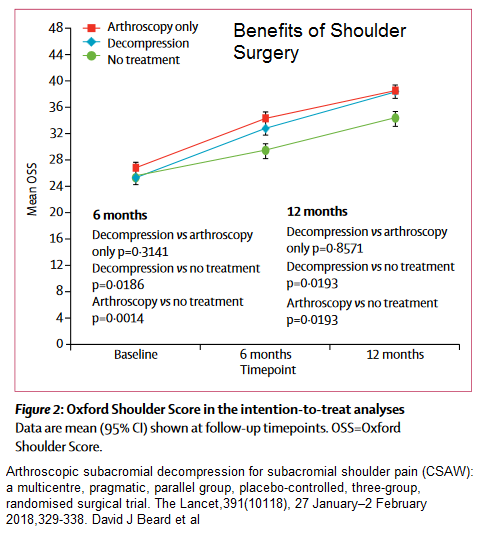 comment – study was done without any attempt to explain why subjects where not better – did they have ac joint issues? was the neck and levator scapula an issue?Was there facet syndromes in neck? was the shoulder tip an issue? Was t4 interscap an issue? was there a pectoralis minor thoracic outlet syndrome?was there regional hypersensitivity that nerve blocks could have helped? was there triggers in deltoid, infraspinatus, and subscapularis muscles? All the above I have seen in past week. People who put their faith in surgery are going to be disappointed. Can’t explain why mid study did well and last so poorly.
comment – study was done without any attempt to explain why subjects where not better – did they have ac joint issues? was the neck and levator scapula an issue?Was there facet syndromes in neck? was the shoulder tip an issue? Was t4 interscap an issue? was there a pectoralis minor thoracic outlet syndrome?was there regional hypersensitivity that nerve blocks could have helped? was there triggers in deltoid, infraspinatus, and subscapularis muscles? All the above I have seen in past week. People who put their faith in surgery are going to be disappointed. Can’t explain why mid study did well and last so poorly.