This is a newly described condition. Ignored as a possible cause of head pain (astoundingly, 6/15 had a prior supraorbital nerve block but not trochlear). Tip off is it’s near midline location. Pressing or stabbing is the usual nature and 9/15 had an intermittent nature with great variability and length. Inner upper orbital rim is tender.
4/15 had bilateral pains, making it more difficult to access. 3-5/15 got lasting effects from blocks; no one drug was consistently used.
Headache. 2017 Oct;57(9):1433-1442. doi: 10.1111/head.13158. Epub 2017 Aug 18.Supratrochlear Neuralgia: A Prospective Case Series of 15 Patients.
Pareja JA et al
https://www.ncbi.nlm.nih.gov/pubmed/28833061
- 51 cases – 13/15 are women
- age 51 +/- 17 years at time study
- age onset 46+/- 17 years
- duration 3 months – 38 years
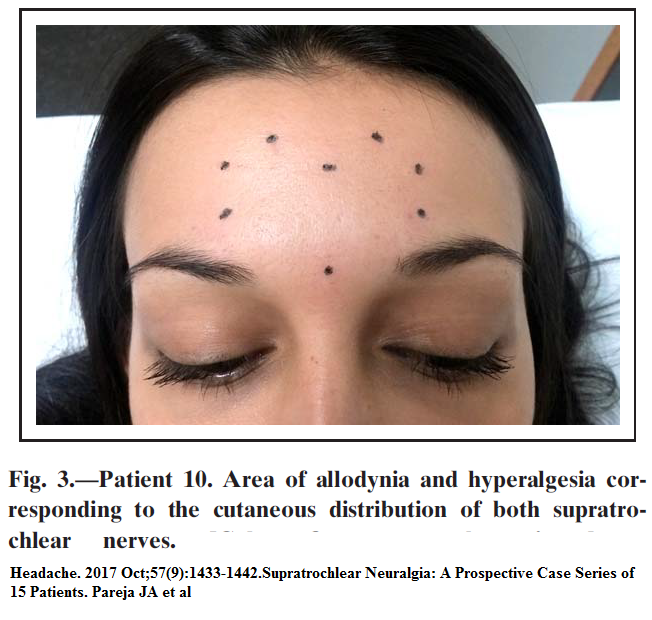
- location is solely in distribution of trochlear nerve though 4/15 had it bilaterally which could make it very confusing
- Pressing 8/15
- stabbing 4/15
- both pressing and throbbing 1/15
- both pressing and electric 1/15
9/15 the pains were intermittent with considerable variability:
from 1 per week (lasting up to 24-72 hours) to 10-15 per day (lasting 5-10 seconds) - 4/15 had bilateral pains
- tenderness near midline forehead and upper inner 1/3 of orbital rim
Possible precipitating causes include tight headband, tight hat, oxygen
mask, or swimming goggles.
Diagnosis was confirmed by trochlear block:
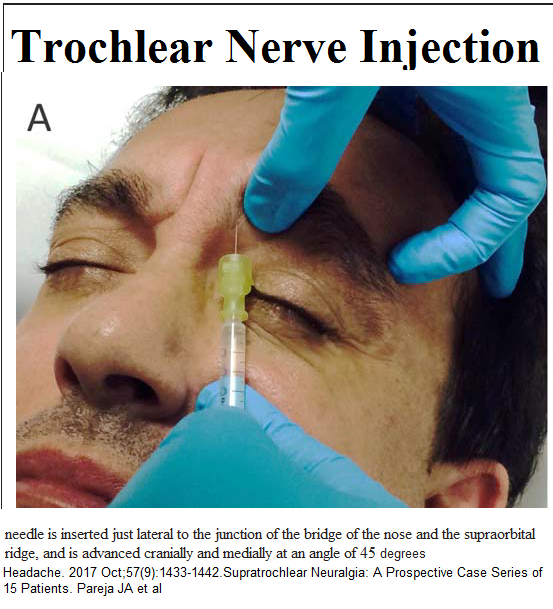
Technique they used:
“Patients were asked to lie supine with the head in a neutral, relaxed position. Local anesthetic was administered through a 30G needle inserted over the emergence
of the supratrochlear nerve along the orbital margin, between the supraorbital notch and the upper external corner of the nasal bone. The needle was directed cranially and medially at an angle of 45 degree (Fig. 1A). A total volume of 0.5 mL of either bupivacaine
0.5% (8 patients), lidocaine 1% (5 patients), or mepivacaine 2% (1 patient) was delivered at the injection site”
Treatments
5/15 blocks worked
3 had lasting effects from block
2 had repeated blocks
Drug treatment included: – one on each of
lacosamide – epilepsy drug for partial seizures not covered by EDS
lamotrigine
amytriptyline
pregabalin
one on duloxetine and pregabalin combo
Comment – sounds similar to trochlear headache
Primary trochlear headache: A new cephalgia generated and modulated on the trochlear region
J. Yangüela, MD*; M. Sánchez-del-Rio, MD*; A. Bueno, MD*; A. Espinosa, MD;
P. Gili, MD*; N. Lopez-Ferrando, MD; F. Barriga, MD*; J.C. Nieto, MD; and J.A. Pareja, MD, PhD*
NEUROLOGY 2004;62:1134–1140
http://www.neurology.org/content/62/7/1134.short
It refers to a wider area:
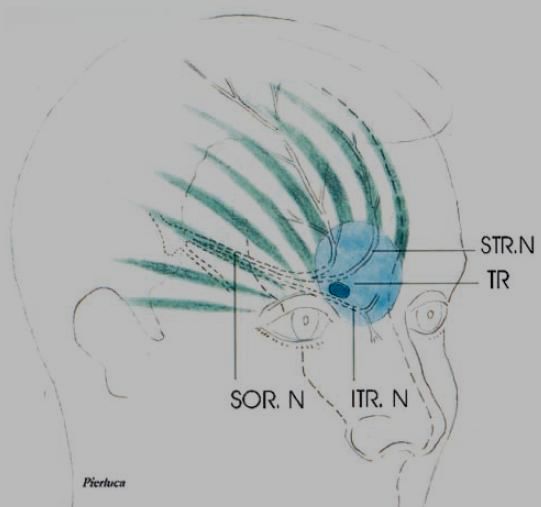
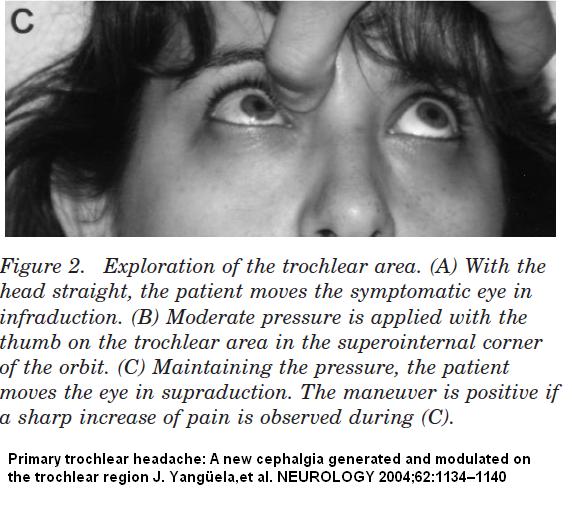
They differentiate it by saying primary trochlear headache originates from originating in the superior oblique muscle-tendon-trochlea complex. I suspect differentiating point would be pain there on pressure that is worse when looking up while holding pressure there:
Primary trochlear headaches respond to a short with cortisone – gave lasting relief though some needed repeats. One wonders if tochlear neuralgia could use steroid in the injection as well. I have been injecting trochlear pains for some time and patients are extremely grateful for no doctor including neurologists/neurosurgeons have thought of injecting there. Author of artcile mentioned cases that had issues for decades. I might have missed bilateral cases but at least injected corrigator muscles with botulinum for it.
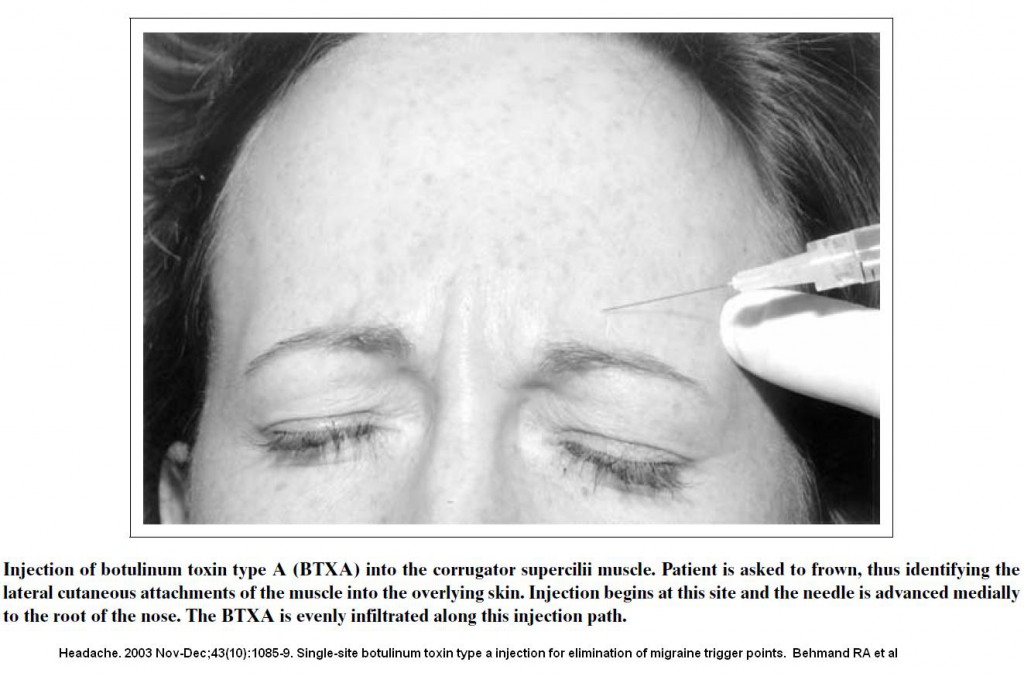
I discuss that technique here – though more likely to inject closer to skin to avoid ptosis issues
http://painmuse.org/?p=2886

I have been suffering with the most debilitating migraines since I had a halo and had screws drilled into my skull in 2000. I can tell you I have tried almost every migraine medication on the market. Nothing and I mean nothing has ever worked as well as the injections or pain blockers. This treatment is the real deal. I am also most excited to report this next part, it didn’t just lessen the pain, it took it away! It was completely gone. I kept waiting for it to come back after a few hours, it didn’t!! It works.
You will have to continue with injections as they will obviously not last forever, however it’s a heck of a lot better than any alternative.
I can’t thank you enough Dr. Montbriand.
You do more for us suffering with chronic illness’s than you could ever know. This world needs more doctors like you!