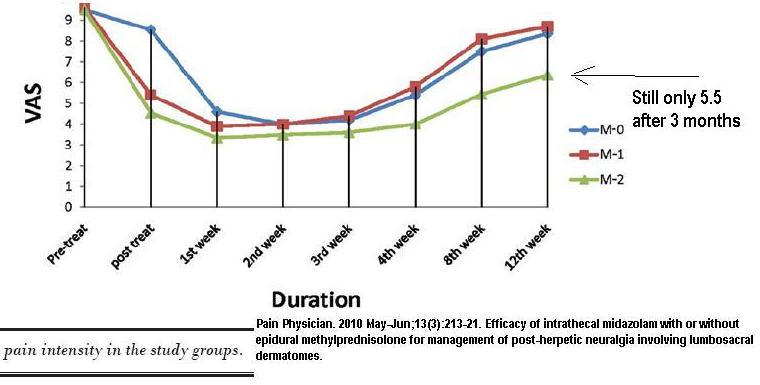
Post Herpetic Neuralgia (PHN) is a horrendous disease with limited options. A group with low back version of this were treated with 60 mg methylprednisolone and 2 mg midazolam in saline epidurally. Note – no local anesthtic block was necessary. Though pains started at near 10/10 on the pain scale, the highest it got after 3 months was 5.5/10. On average, painkiller pill consumption went from 25 tablets/day to 5/day even after 3 months. These results are miraculous and I hope to spread the news.
Pain Physician. 2010 May-Jun;13(3):213-21.
Efficacy of intrathecal midazolam with or without epidural methylprednisolone for management of post-herpetic neuralgia involving lumbosacral dermatomes.
Dureja GP, Usmani H, Khan M, Tahseen M, Jamal A. free article here
- 150 cases – randomized to either methylprednisolone alone (m0), midazolam alone (m1), , or the combo (m2) (I’m impressed – 50 cases each group gives it good statistical power)
- Epidural technique fairly standard: “The patients were kept in the left or right lateral position with the affected side down. The epidural injections were given either at the L1-L2 or L2-L3 intervertebral
space. An 18-gauge Tuohy needle was used for injection into the epidural space which was identified by
the loss of resistance technique.” They used dye to confirm placement but in clinical practice one could leave that out. - Spinal Intrathecal technique: – “The intrathecal injections were given at one segment lower than epidural injections i.e. L2-L3 or L3-L4 intervertebral space using a 23-gauge, Quincke spinal needle. The intrathecal injection was given after confirming the free flow of cerebrospinal fluid (CSF) through the spinal needle.”
- They had an interesting technique for inducing allodynia (painful touch) – “allodynia was elicited by stroking the skin with a 2 cm wide electrical toothbrush (Oral-B, Procter and Gamble Ltd).”
- Side effects: – “One patient in Group M-2 complained of difficulty in breathing after the intrathecal injection. On examination, the patient had an increased respiratory rate and heart rate, but there was no change in mean arterial pressure and arterial oxygen saturation on air from the baseline value.” – was better after 1/2 hour.
– Sedation was an issue – They monitored it on a four point scale.
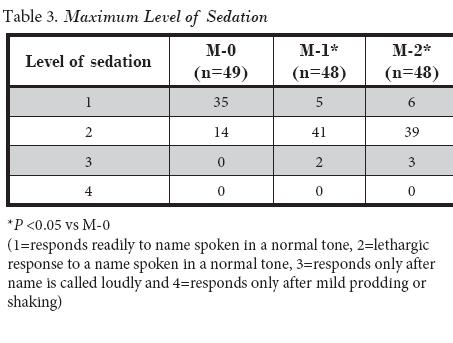
Given that Midazolam is a “doctor rape” drug where I live, its use in females should not be done without a female assistant or a family member present. - Results:
- Comment – I have tried to make a list of some alternate approaches here:
Alternate Approaches to Post-Herpetic Neuralgia (PHN)
If they were combined with those injections, I bet one could cut that pain in at least half that.
- A prior article using midazolam spinal found it had good results in mechanical back pain:
Pain. 1992 Jan;48(1):5-12.
Intrathecal midazolam for the treatment of chronic mechanical low back pain: a controlled comparison with epidural steroid in a pilot study.
Serrao JM, Marks RL, Morley SJ, Goodchild CS. abstract here
They felt it worked better than 80 mg methylprednisolone.
When I used to do caudal blocks I added it in (large volume dilution), I found patients preferred it because there was no headache afterwards. Then, when news came out that it could be a doctor rape drug , I got rid of it. I suspect it will have to be used epidurally for both drugs if done thoracic level. - Also, I have a plea to doctors – this study made point of saying they used preservative free saline. You can greatly make your steroid more preservative free by letting the steroid settle out and draw out the white powder segment only for use – the rest is just preservative.
- One wonders it it could all be given spinally as was done in a New England Journal of Medicine article:
N Engl J Med. 2000 Nov 23;343(21):1514-9.
Intrathecal methylprednisolone for intractable postherpetic neuralgia.
Kotani N, Kushikata T, Hashimoto H, Kimura F, Muraoka M, Yodono M, Asai M,
Matsuki A. free article here
they gave 60 mg methylprednisolone acetate and 3 mls of 3% lidocaine spinally though an L2 puncture and were able to help people with thoracic and cervical post herpetic neuralgia. Technique was:
“For patients whose pain was located in the upper thoracic or cervical area, we tilted the operating table into the head-down position immediately after the intrathecal injection to allow the injected material to spread to the upper thoracic canal and to the nerves of the involved dermatomes. Patients with abdominal or lower-body pain were kept in a horizontal position.” This was faciliated by having a specific gravity of 1.035 so it would flow up. In their study the lidocaine alone had no effect. Theoretically, one could give steroid alone and add 7.5% dextrose (sp.gr only 1.025 though). The addition of midazolam to that mix would make it work better but I’m not sure about tilting that up…
NOTE there were FOUR weekly injections
They got good – excellent pain relief in 82/89 cases that persisted for up to 2 years – wow
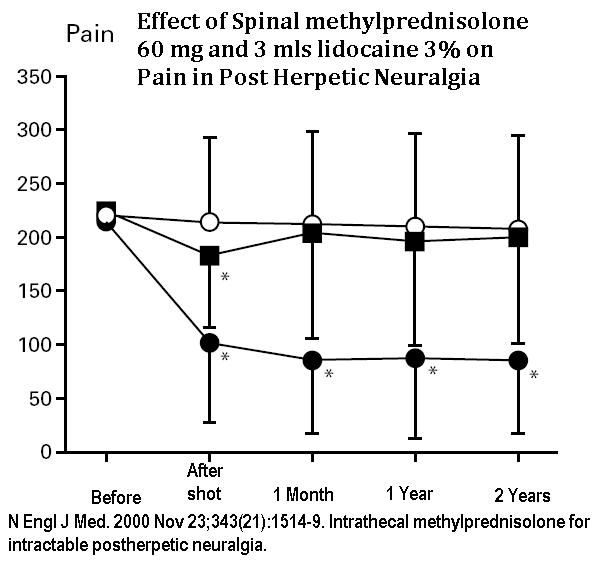
Area of allodynia was reduced 70% as well.
In a commentary of this study the NEJM editor mentioned “Adhesive arachnoiditis with chronic inflammation and scarring in the arachnoidea mater around the spinal cord and nerves is one of the most worrisome complications of intrathecal injection.” – I suspect if the steroid was allowed to settle out, the preservative drained off the top, and only the white settled powder used, fears of that would be much less. He did mention none was seen in the two year followup. He did wonder if facial PHN would be treatable – “Perhaps future studies in patients with intractable postherpetic neuralgia should assess the use of injections of corticosteroids into Meckel’s cave, which is the area of the subarachnoid space around the trigeminal ganglion.“
Comment – perhaps using midazolam 2 mg and 60 mg methylprednisolone in preserative free saline without local would be a good combination. Putting patient sidelying bad side down might help as well.
Any comments or experience with such?

Pingback: Sweet Epidural Caudal Sugar-Water Injections Cut Back Pain Longterm | Pain Medical Musing