Analysis of 41 cases of juvenile widespread pain found “definite SFPN (small fiber polyneuropathy) in 59%, probable SFPN in 17%, and possible SFPN in 22%. Steroids or IV gamma globulin subjectively helped 80% of those that tried them.
Oaklander, Anne Louise, and Max M. Klein.
Evidence of small-fiber polyneuropathy in unexplained, juvenile-onset, widespread pain syndromes.
Pediatrics 131.4 (2013): e1091-e1100.
Oaklander AL, Klein MM. Department of Neurology, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4074641/pdf/peds.2012-2597.pdf
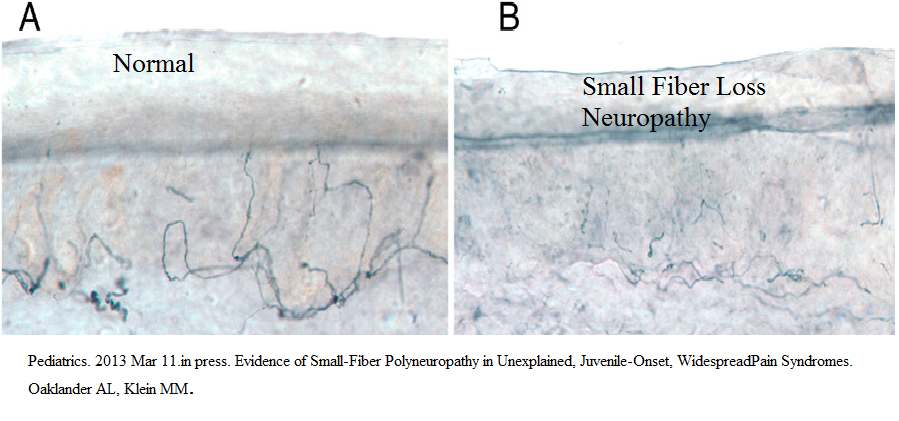
Biopsies would show small fiber loss:
Symptoms:
- Pain began or mostly in legs
- 63% Chronic disabling headaches
- 83% Chronic disabling fatigue
Other Symptoms: – mostly autonomic
- 90% cardiovascular – refractory hypotension, chronic tachycardia usually well tolerated, POTS with postural hypotension, labile Blood Pressure
- 82% gastrointestinal – nausea, vomiting, constipation, irritable bowel, functional dyspepsia; maybe gastroparesis lazy bowel syndrome
- 4 cases polycystic ovaries obese, irregular periods, multiple cysts on ovaries in US
- 3 Ehlers-Danlos syndrome – hypermobility syndrome with elastic skin
- Psychiatric – somatization, conversion diagnosis though actually only one depression
- 34% Urologic – annoyingly does not say what symptoms are, but assume either painless full bladder with overflow or spastic bladder with frequency and trouble voiding.
- few cases erythromelalgia (pain worsened by heat, plus redness and swelling) that was worse in face cheeks and ears but also affected legs
- patchy sweating issues
Predisposing – “Sixty-one percent of patients/families attributed onset of their illness to preceding infections or injuries. Twenty five percent had documented preceding infections including Mycoplasma pneumoniae, Bordatella pertussis, Mycobacterium tuberculosis, group A Streptococcus, mononucleosis, influenza, and parvovirus. Among the 11 documented injuries shortly preceding onset of widespread pain, 10 were limb injuries (eg, fractures, sprains, frostbite) featuring excess pain and swelling interpreted as complex regional pain syndrome. These had largely resolved and were distinct from the later widespread and multifocal pain illnesses studied here.”
Physical exam:
- “Neurologic examinations identified reduced sensation in 68% and vasomotor abnormalities in 55%, including 23% with erythromelalgia”
- I presume those w1th POTS would show differences in upright versus lying BP’s
- Those with GI symptoms may show bowels loaded with stool.
- hypermobility maybe
- obesity and polycystic ovaries maybe
Lab Tests
Most subjects were submitted to a wide variety of tests – all below normal:
- Cerebrospinal fluid tests: All tests were normal in 11 patients
- Blood tests: Complete blood count, electrolytes including glucose, renal, liver, and thyroid function, hemoglobin A1c levels, lipids, vitamins, and immunoglobulins, serum protein immunofixation
- Urine tests: Heavy metals, protein immunofixation, porphyrins, amino and organic acids
- Infectious tests: Hepatitis C, syphilis, human immunodeficiency virus, deer-associated zoonotic infections including Lyme, babesiosis, and human monocytic ehrlichiosis
- Immune tests: Rheumatoid factor antibody, Sjögren’s autoantibodies (Ro/SS-A, La/SS-B), lupus autoantibodies (anti-dsDNA, Sm, RNP), antineutrophil cytoplasmic antibodies, total complement
- Genetic tests: Only occasionally performed: all tests for genetic neuropathy includingCharcot-Marie-Tooth, Fabry, transthyretin, hereditary neuropathy with liability to pressure palsy, also familial hemiplegic migraine, cystic fibrosis
Abnormal blood tests included:
- Elevated ESR (>/= 15 mm/h) 37% (15/41)
- Elevated antinuclear antibodies (>/= 1:80 dilution) 45% (17/38
- Reduced C3 (<85 mg/dL) 21% (6/29)
- Reduced C4 (<20 mg/dL) 46% (13/28)
Any 1 or more of the above blood test abnormalities 89% (32/36)
Concomitant illnesses included
- 2 Sjogren’s spectrum disorder
- One type 1 diabetes which was not relevant as subject responded to steroids.
Autonomic Function Testing (AFT)
Autonomic function testing was more sensitive. They included “cardiovagal, adrenergic, and sudomotor small-fiber function”.
– heart rate variability during deep breathing (6 breaths per minute while supine)[used manufacturer’s ranges] 27 vs 3% controls abnormal
–Valsalva maneuver – In:
DETECTION OF SMALL-FIBER NEUROPATHY
BY SUDOMOTOR TESTING
VICTORIA A. LOW, MS, PAOLA SANDRONI, MD, PhD,
ROBERT D. FEALEY, MD, and PHILLIP A. LOW, MD
Muscle Nerve 34: 57–61, 2006
“For the Valsalva maneuver, the subject was rested and recumbent and was asked to maintain a column of mercury at 40 mm Hg (I presume blowing out) for 15 seconds. The Valsalva ratio is the ratio of maximal to minimal heart rate.”
–Tilt test: Hemodynamic responses during 80° head-up tilt. “For tilt testing, abnormal was a systolic blood pressure drop >20 mm Hg, diastolic blood pressure drop >10 mm Hg,42 and/or heart rate increase >/=40 (</=18 years) or >/=30 beats per minute (>18 years) within 3 minutes of tilt.”
– sudomotor sweat testing – “involves applying Alizarin red indicator to the skin before controlled heating; it is orange when dry and turns purple when wet.”
11 skin biopsies, 2 nerve biopsies – definitive – 32%
22 – Minor abnormalities in skin biopsies – 54%
? 14% normal
18 AFT were definitively – 44%
14 minor AFT abnormalities – 34%
?22% normal
only 1/41 had totally normal results.
Treatments:
- avoiding potentiating medications
- increased fluid intake
- avoid prolonged standing,
- contracti leg muscles while standing,
- elevating head of the bed
- compressive stockings
- abdominal binders
- midodrine
fludrocortisone
For tachycardia: – calcium-channel blockers or beta-blockers as long as not hypotensive
Abdominal problems:
- high fiber diets
- small meals
- elevating the head of the bed,
- avoiding lying down after eat
Constipation and nausea/vomiting : meds; 3 needed admission for fecal disimpaction
Chronic Widespread Pain – gabapentin; nortriptyline and desipramine if cardiovascular stable. rarely opioids.
Erythromelalgia – mexilitine
Steroids
5 severely ill hospitalized patients : intravenous methylprednisolone (1 g/day for 5 days) followed by a prednisone taper – 2 responded over 3 month; 3 no help but had it for years
Outpatient:oral prednisone (1 mg/kg/day for 4 weeks followed by rapid taper), – 8 improved; 2 did not.
Complications – One case of cataracts
Intravenous Immunoglobulin (IVIG)- 11 cases – > 3 times of dose 2 g/kg – 3 did not have enough; 5 responded and continued with treatments
Complications – One had a Deep vein thrombosis and rash
“Treatment with corticosteroids and/or intravenous immune globulin objectively and subjectively benefited 80% of patients [who tried it](12/15).” Corticosteroids helped 67% (10/15) cases where employed.
Comment – Condition appears like Chronic Inflammatory demyelination Polyneuropathy (CIDP) except there, the authors settled for four days of oral dexamethasone 40 mg/day X four days because methyprednisolone was too hard on veins( for adults)
J Neurol Neurosurg Psychiatry 1997;62:388-390
Pulsed high dose dexamethasone treatment in chronic inflammatory demyelinating polyneuropathy: a pilot study.
D S Molenaar, P A van Doorn, M Vermeulen free article here
This high a dose had also been in ITP (a platelet disorder):
Andersen JC.
Response of resistant idiopathic thrombocytopenic purpura to pulsed high-dose dexamethasone therapy.
N Engl J Med 1994;330:1560-4.
I wonder if this could be scaled down for children.
News of this needs to reach parents desperate for treatment of their children with widespread pain.

Pingback: Postural Orthostatic Tachycardia Syndrome (POTS) – More Complex in Chronic Pain | Pain Medical Musing