For years, I have been working and injecting the muscles around the knee to promote relief from knee pains. Sometimes it makes a big difference; sometimes the joint line osteoarthritis is more important. Two studies hi-light muscle issues in patellofemoral pains but also cases waiting for knee replacement pains.
First of all, I would like to summarize some of the areas about the knee that I have seen as a problem:
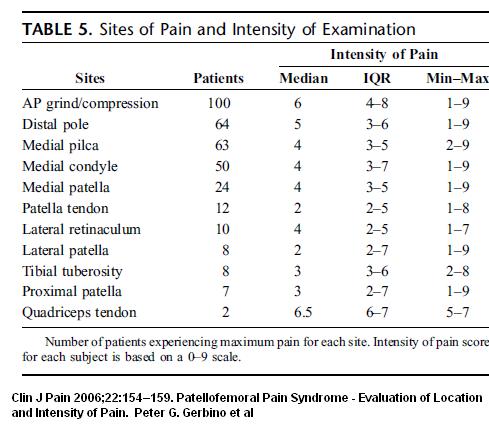
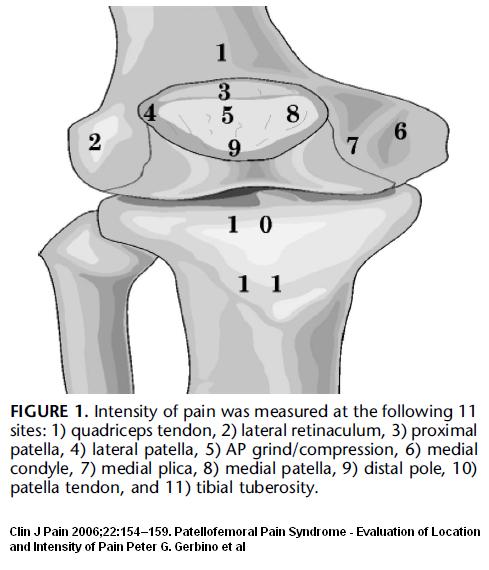
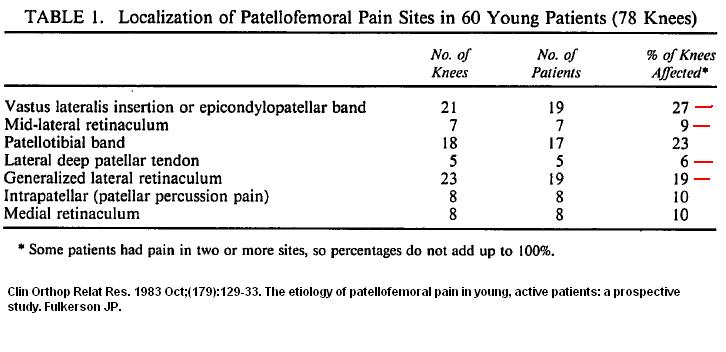
Various areas external to the knee are involved in knee pains. Though article below ignores areas beyond patella like adductor muscles because only discussing patellofemoral pain – it does document some locations :
Clin J Pain. 2006 Feb;22(2):154-9.
Patellofemoral pain syndrome: evaluation of location and intensity of pain.
Gerbino PG 2nd, Griffin ED, d’Hemecourt PA, Kim T, Kocher MS, Zurakowski D, Micheli LJ. abstract here
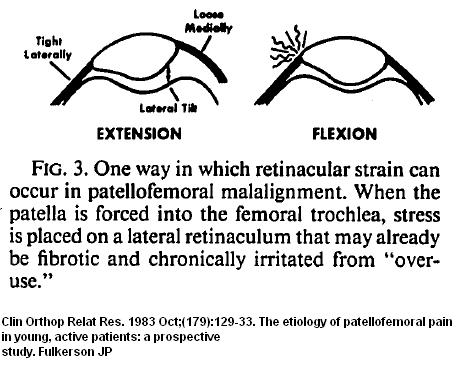
Lateral Retinaculum as Source of Pain
Above article mentions Fulkerson
Clin Orthop Relat Res. 1983 Oct;(179):129-33.
The etiology of patellofemoral pain in young, active patients: a prospective study.
Fulkerson JP. abstract here
and stated:
“In his 1983 report in which he was specifically looking for the etiology of patellofemoral pain, Fulkerson found that 90% of patients had lateral retinacular pain, and only 10% had pain with patellar compression.7″
Here is Fulkerson’s list – remembering that lateral retinaculum is divided into various parts:
The nerve to the lateral kneecap goes through this tissue and can be irritated or damaged by the tissues. In Peter G. Gerbino et al article (first one) they say “Neuromatous
degeneration in the lateral retinaculum, originally described by Fulkerson (above) and later by Sanchis-Alfonso.”
The Fulkerson article would be:
Fulkerson JP, Tennant R, Jaivin JS, et al. Histologic evidence of retinacular nerve injury associated with patellofemoral malalignment.
Clin Orthop. 1985;184:196–205. abstract here
He found that there was in that lateral reinaculum, there was “consistent evidence of nerve damage (demyelination and fibrosis)” that looked very much like the damage one sees in a morton’s neuroma. This gets my attention because morton’s neuroma can cause severe neuropathic pain. To make things more interesting author states in these severe patellofemoral cases, “little or no evidence of chondromalacia patellae in these patients” – suggesting most of the pain came from the lateral retinaculum.
This nerve damage in the lateral retinaculum was confirmed by :
Am J Sports Med. 1998 Sep-Oct;26(5):703-9.Quantitative analysis of nerve changes in the lateral retinaculum in patients
with isolated symptomatic patellofemoral malalignment. A preliminary study.
Sanchis-Alfonso V, Roselló-Sastre E, Monteagudo-Castro C, Esquerdo J. abstract here
Sanchis-Alfonso went on to demonstrate elevated levels of neural growth factor associated with the proliferation of painful neurovascular tissue ‘angiogenesis’
Acta Orthop Scand. 2001 Apr;72(2):146-9.
Neural growth factor expression in the lateral retinaculum in painfulpatellofemoral malalignment.
Sanchis-Alfonso V, Roselló-Sastre E, Revert F.
“Neural growth factor is related to neural proliferation in vessels and perivascular tissue and to the release of neuroceptive transmitters, such as substance P. We postulate that both mechanisms are involved in the pathogenesis of pain in isolated symptomatic patellofemoral malalignment.”
I have written about how important this neurovascular tissue growth is – it is seen in chronic tendonitis: – painful neurovascular fuzz
Does Pain “Grow” at Tendon injury sites? -and Treatment tennis elbow
and neurovascular growth has been seen in the foraminal outlets in sciatica/radiculopathy.
Sanchis-Alfonso went on to develop a “Neural model” of anterior knee pains in young patients:
Acta Orthop Scand. 2003 Dec;74(6):697-703.
Anterior knee pain in the young patient–what causes the pain? “Neural model”.
Sanchis-Alfonso V, Roselló-Sastre E. abstract here
“On the basis of our recent research, we suggest a “neural model”. In our view, hyperinnervation in the lateral retinaculum, mainly nociceptivesubstance P-positive nerves induced by the release of neural growth factor, is involved in the pathogenesis of anterior knee pain. We hypothesize that periodic short episodes of ischemiamay trigger neural proliferation.”
Lateral retinculum tighness is well known in knee disorders and it was felt that knee flexion constantly tugged on lateral retinaculum and irritated it:
.
.
.
.
.
.
.
.
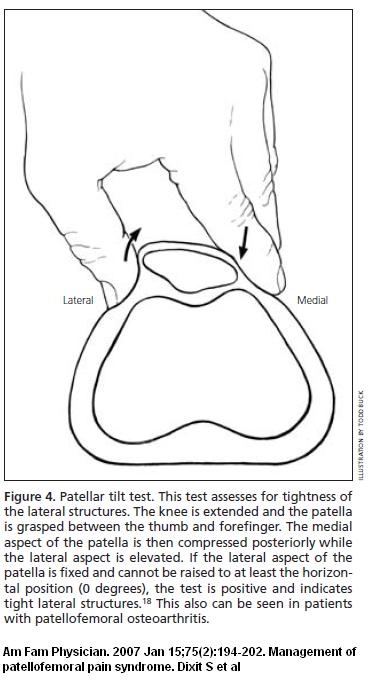
.This tighness can be confirmed by the inability to medial tilt the patella to horizontal:
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
and inability to move kneecap at least 1/4 of the kneecaps breath (one quadrant) medially:
.
.
.
.
.
.
.
.
.
.
.
.
I push the lateral retinaculum medially using no-slip latex goves until it releases some (very painful and then knuckle it back and forth until it releases. Often I will not get a release and will inject the suprapatellar lateral retinculum areas with semineurolytic 5% lidocaine (up to 2 mls at as treatment) and then work muscles completely out. A few treatments will render it relatively painfree.
Medial retinaculum
Less common than lateral but the nerve to the medial upper kneecap traverses it and it does get painful usually in combination with lateral retinacular issues. Is strained by patellar dislocations. I would inject it the same way.
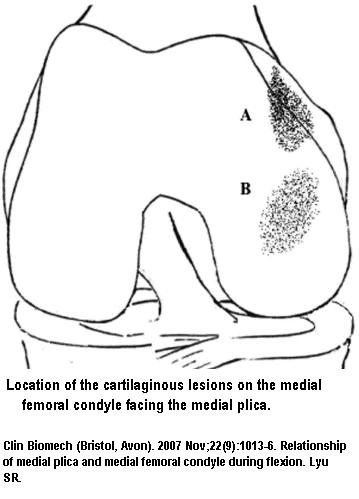
Medial Plica Syndrome
I find this is common and missed. One author stated “most commonly missed diagnoses in the knee”. Just media to the kneecap, there is a band of tissue that goes down the side of the kneecap and into the joint.
.
.
.
.
.
.
.
.
.
.
.
- Put your thumb on the inside of the kneecap – there will be some “stringlike tissue there” – if you hold pressure on it and bend the knee, it might snap and be painful as you hold pressure on it.
- Gerbino above discussed it and stated “Some believe that direct trauma produces an inflamed plicathat rubs the medial condyle ridge, leading to pain at both sites. Others have stated that a lateral-tracking patella causes fibrosis and inflammation to an otherwise normal plica as it rubs against the condyle. A high incidence of lateral patellar tracking would be expected in those patients with both PFS and plica syndrome.”
It has been said the plica tightens the medial knee compartment and accelerates medial OA knee:
.
.
.
.
.
.
.
.
.
.
.
One author found cutting that plica was useful in OA Knee;
Bone Joint Surg Br. 2008 Sep;90(9):1186-92.
Arthroscopic medial release for medial compartment osteoarthritis of the knee:the result of a single surgeon series with a minimum follow-up of four years.
Lyu SR. abstract here
- In 255 knee, it had a 77.3% satisfactory results in relieving OA knee pains medial knee
- “Based on these observations arthroscopic medial release is an effective treatment for osteoarthritis of the medial compartment of the knee joint and can be expected to reduce the pain in the majority of patients for at least four years post-operatively.”
- I asked a local orthopod about this study over 1 year ago and he laughed it off like it was crazy – now it looks quite possibly helpful – though replications need to be done – sadly, I found none so far.
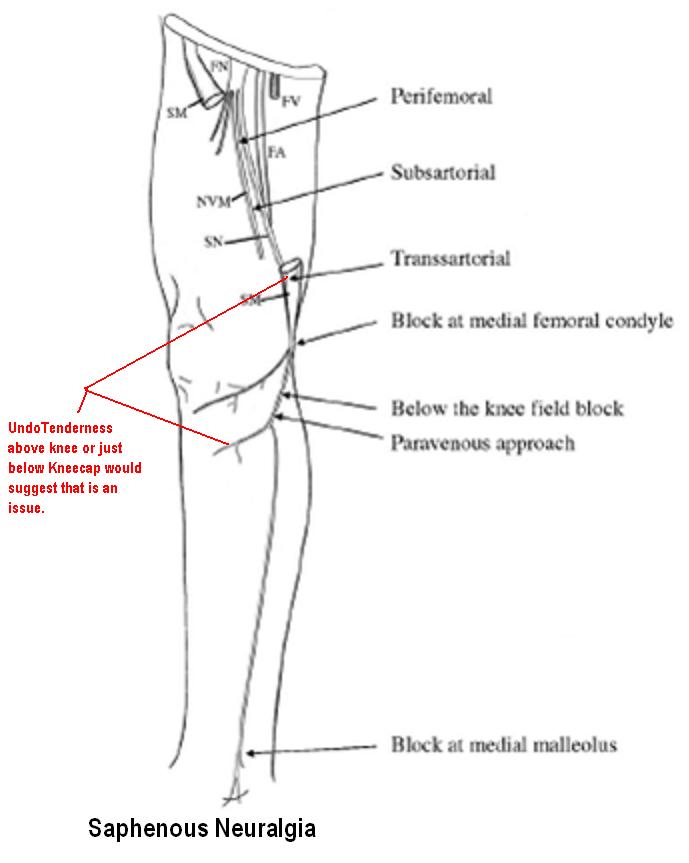
Saphenous Neuritis
I am surprised how often I see this condition. There will be out of propotion pain in the leg/knee and undo tenderness above the knee where saphenous nerve exits and below knee where infrapatellar extensons curl. I am often amazed to find the tenderness can be tracked all the way medial knee to the obturator nerve area below lateral pubis.
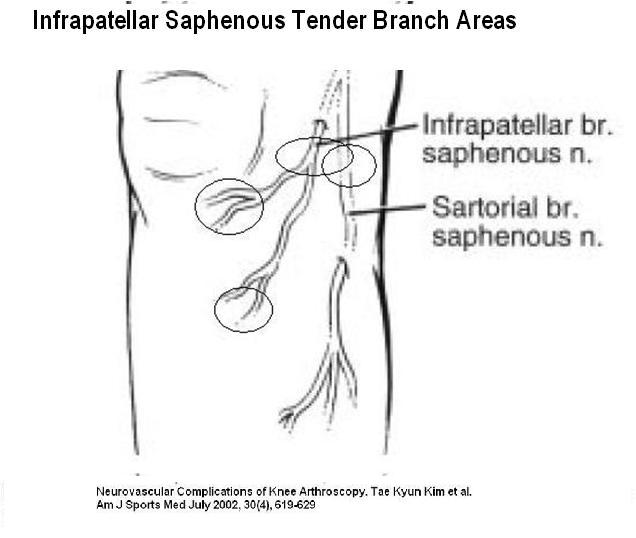 .
.
Described in detail by:
J Am Acad Orthop Surg. 2002 Mar-Apr;10(2):130-7.
Saphenous neuritis: a poorly understood cause of medial knee pain.
Morganti CM, McFarland EG, Cosgarea AJ. abstract here
- Medial Knee Pain – indolent and poorly understood
- Associated with double crunch, medial knee OA or anserinus bursitis
- Exquisite tenderness to spots lower than patella or above medial joint line – though annoyingly could be joint line but only one spot tenderness
- Activity worsening but most importantly REST PAIN
- ?Tinels sign – if post operative not been that lucky
- Adductor canal tenderness
- Response to blocks – its easier to do in adductor canal level in Saphernous Nerve but sometimes the whole medial leg is sore so I give it at Obturator nerve level
One case I had was
- a former policeman with post laminectomy and left knee OA (double crunch for sure)
- pains knee very bad
- Consuming Morphine 100 mg multiple doses at a time yet poor control pain
- Area below knee very tender as well as one spot on knee joint medially;
- rest pain
- Saphenous nerve Blocks re-established some control until had knee surgery
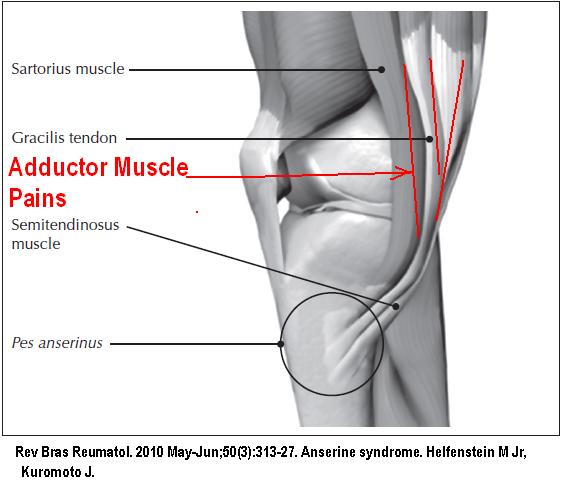
Adductor Muscles and Anserine Bursitis
- I do find the medial adductor area is often tender in OA knee and how much it contributes to pain is an issue:
.
.
.
.
.
.
.
.
.
.
.
- The only sure way I have found to tell the difference between anserine bursitis and adductor muscle issues is to work out the muscles. While wearing latex gloves for grip I will grab the muscle on hand below the other and push on side and pull the other as hard as I can – it can be quite painful but eventually (after several back and forward changes) the muscles will release and any residual pains can be knuckled back and forth out.
- Sometimes I am amazed to find a localized small area below knee remains present though in many cases there is nothing left at all. This would go along with the finding that many do not have any evidence of buristis on ultrasound or MRI (only 2.5% – 8.3%). Those with the small round area of soreness left behind I would inject with steroid.
- A study, as far as I can tell that did not attempt to make the distinction, did not find the addition of steroid helped at all:
Reumatol Clin. 2012 Mar-Apr;8(2):63-7.
Safety and efficacy of methylprednisolone infiltration in anserine syndrome treatment.
Vega-Morales D, Esquivel-Valerio JA, Negrete-López R, Galarza-Delgado DÁ, Garza-Elizondo MA.
– The injection technique was performed in the most painful spot – which, when the muscles are sore, could be a large area.
– pain went from 7 10 2.5 in steroid group and 7.1 to 2.0 in in the just local group at 4 weeks – making you wonder if local should be tried first. - Some cases may be merely a branch of the saphenous nerve at the knee.
- One interesting observation I have had was that Botox injected in the knee will give relief of knee pain but none for the anserine concurrent area, while steroid in the knee joint seems to work for both. Want better – longer lasting effect of steroid? Cases where I then had to use steroid to mop up what was left after botox then had more profound – long lasting relief.
Quadraceps expansion just above kneecap
In knee contractured following knee replacement , this can be very tight and need injection (under antibiotic coverage) and vigorous muscle work.
Tibio-fibular joint
Surprising as it may seem, I have seen cases of “intractible knee pains” that weren’t even in the knee but just below it laterally in the tibiofibular joint. This responds well to injection.
Now for the two recent studies:
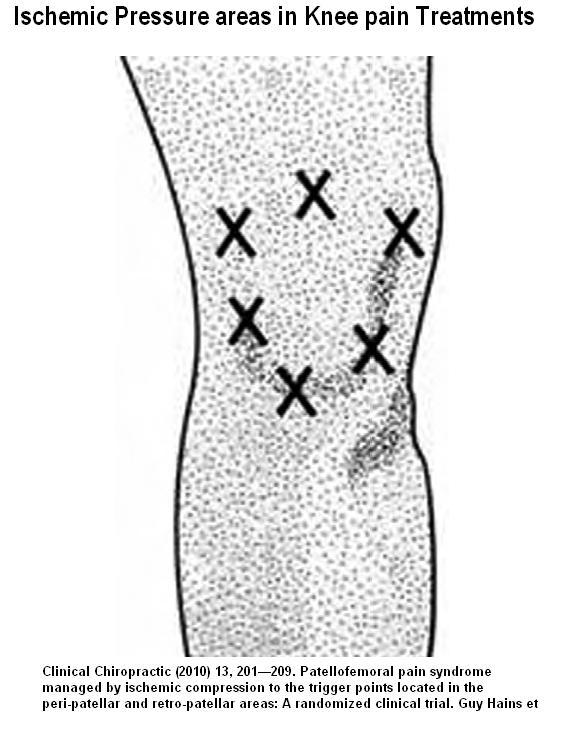
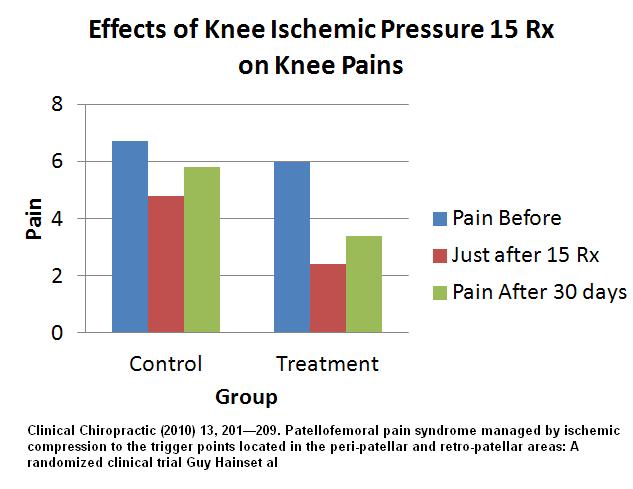
Clinical Chiropractic (2010) 13, 201—209
Patellofemoral pain syndrome managed by ischemic compression to the trigger points located in the peri-patellar and retro-patellar areas: A randomized clinical trial
Guy Hains, Franc¸ois Hains free article here
- 15 sessions of manual ischemic compression applied to peri-patellar and retro-patellar regions vs control group that did compression over gluteal muscles –
- Procedure (is involved so quoted):
“Ischemic compression therapy was used in both groups (in different areas). It consisted of the practitioner applying a sustained digital pressure to the areas of elicited pain for between 5 and 15 s. The practitioner began with light firm pressure and gradually increased the pressure used until the patient’s maximum pain tolerance was reached. To accommodate patient comfort, when many trigger points were elicited during examination, each point was held for less time than if fewer trigger points were elicited.””The treatment group received ischemic compression therapy to elicited trigger points (if any) in the peri-patellar region (see Fig. 1). Beginning with light pressure, one thumb on the other, compression was applied to hyperirritable foci. Pressure was gradually increased up to the patient’s maximum pain tolerance. Using at each visit the patellar-grinding test to locate the hyperirritable foci (if any) located under the patella (retro-patellar trigger points), the author would apply a compressive force on the patella by grasping it using a broad contact (web of the practitioner’s hand) and pushing it towards each hyperirritated focus. Since this maneuver could be extremely painful, the practitioner would apply pressure very carefully and within the patient’s pain tolerance limits. This modification to ischemic compression was used for retro-patellar pain. It was based on the hypothesis that passive oriented patellar mobilization would function in the same manner as ischemic compression and would result in the elimination of retro-patellar trigger points. This procedure was applied until complete elimination of the trigger points or until the completion of the 15 treatments. “
.
.
.
.
.
.
.
.
.
.
.
Results:
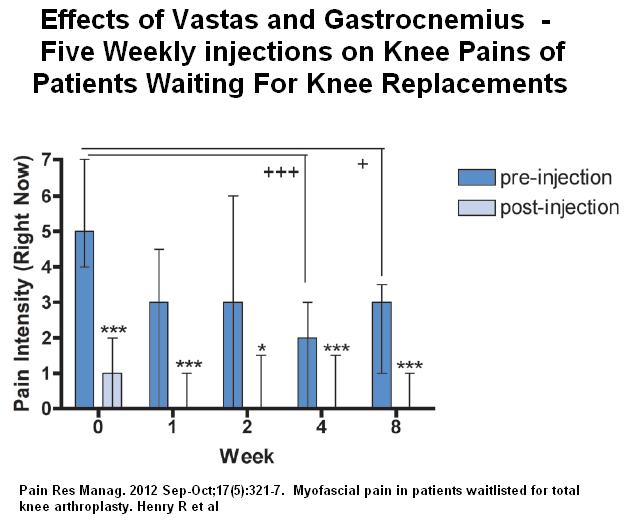
Second Study:
Pain Res Manag. 2012 Sep-Oct;17(5):321-7.
Myofascial pain in patients waitlisted for total knee arthroplasty.
Henry R, Cahill CM, Wood G, Hroch J, Wilson R, Cupido T, Vandenkerkhof E. abstract here
- 25 cases waiting for knee replacement
- Injected triggers in:
Medial Vastas – 67%
Lateral Vastas – 29%
Medial Gastrocnemius – 92%
Lateral Gastrocnemius – 29%
- 62.5 % had trigger only in medial muscles; 0% in only lateral muscles and 37.5% in both
- 0.25% bupivacane;
- 25 gauge needle,
- 1.5 inch needle
- “were made at points of maximal tenderness … until pain ceased or no further trigger points were found.”
- 5 weekly injections
- Felt that not only could they help with the burden of knee pains but also perhaps in the need for Total Knee Replacement
Comment – refreshing to see both manual and injections techniques developed to help chronic knee pains. They latter is a warning to patients that knee replacement might leave behind sore muscles that need fixing before one would feel better. I usually combine my injections with interposed sessions of just massage/stretching and manual techniques; I wonder if the latter study could have moped up some areas missed by injections.




Pingback: Flossing Saphenous Nerve For Saphenous Neuralgia | Pain Medical Musing