Having come across a case of resistant rotator cuff (supraspinatus) impingment syndrome, I have been looking for answers. Some treatments include:
1) NSAID’s – arthritis pills. Also it is possible to augment NSAID’s with doxycycline, as mentioned in another blog note. here . SAMe had possibilities as well and was mentioned here
2) Cyriax deep frictions – I do them, but having picked the worst cases to use it on, my results have been mixed.
3) Steroid injections – Often given into subacromial bursa to avoid any tendon rupture but little evidence one shot gives lasting results. I call this the one-shot-wonder syndrome. It seems unlikely to me, that anything bad enough to need a shot, would respond easily to one shot. I would suggest kenalog 40 mg every 3 weeks times three or as needed.
4) Suprascapular nerve blocks – There is a study that demonstrated accelerated recovery with suprascapular nerve blocks.
Eura Medicophys. 2006 Sep;42(3):195-204 Pain relief in early rehabilitation of rotator cuff tendinitis: any role for indirect suprascapular nerve block? Di Lorenzo L. 1, Pappagallo M. 2, Gimigliano R. 3, Palmieri E. 4, Saviano E. 1, Bello A. 1, Forte A. 1, DeBlasio E. 5, Trombetti C.
free article here
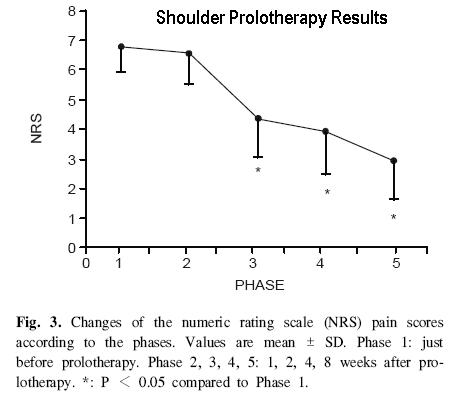
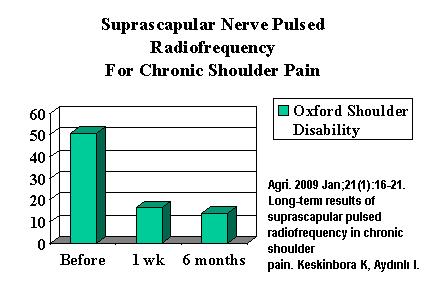
OK – this is a difficult graph – here’s it explained:
- Green had 2 supraclavicular blocks – at week 1 and 2. They also had physio which continued to end of study so that is why there are further readings.
- Blue is control but was crossed over and got shots on week 3 so are not included on chart after that point.
I would suspect further inprovement would have occurred if they continued the shots past only two.
Why did they help? My take:
- The nervous system is a necessary player in inflammation and in rats models arthritic degeneration declines without nerve involvement. Numb the nerve, slow the inflammation. The sympathetic nervous system is involved in inflammation as well, and it is temporarily shut down.
- The suprascapular nerve feeds the supraspinatus and infraspinatus muscles – they relax, their knots relax, – this loosens up the joint so it is less impinged.
- Following suprascapular nerve blocks, I have found the subscapularis is often relaxed (yes, I massage it out and It takes me around 120 rubs to do so – for any massage therapist viewers)- this muscle is huge and is a major contractor of the joint in conditions like frozen shoulder. To have it relaxed would loosen up the joint considerably. How is it possible to get that muscle relaxed? Well, I sometimes use 2% lidocaine as I do not use imaging control. The nerve to the upper subscapular nerve runs posterior to the scapular notch (where injection is given) and it must get anesthetized by spread from the suprascapular notch.
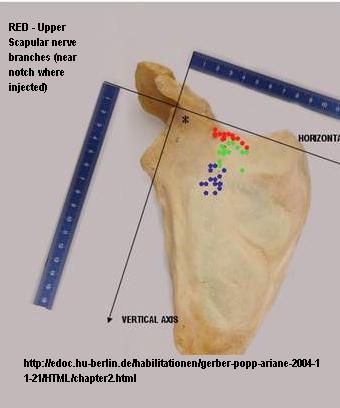
View of scapula looking at front side.
Article found shots lasted a week. I feel they should be continued for weekly 6-8 weeks to maximize benefits. The article also goes into detail of how the injection can be given so I won’t here.
3) Working the myofascial trigger – this is under study right now. article here
I spend considerable time unknotting the deltoid.
One article found “Active TrPs in the supraspinatus (67%), infraspinatus (42%), and subscapularis (42%) muscles” compared to controls
Exp Brain Res. 2010 Feb 26. [Epub ahead of print]
Muscle trigger points and pressure pain hyperalgesia in the shoulder muscles in
patients with unilateral shoulder impingement: a blinded, controlled study. abstract
Hidalgo-Lozano A, Fernández-de-Las-Peñas C, Alonso-Blanco C, Ge HY,
Arendt-Nielsen L, Arroyo-Morales M.
5) ? Botox. Botox has been shown to work well for shoulder arthrtis for 12 weeks + relief shoulder pain:
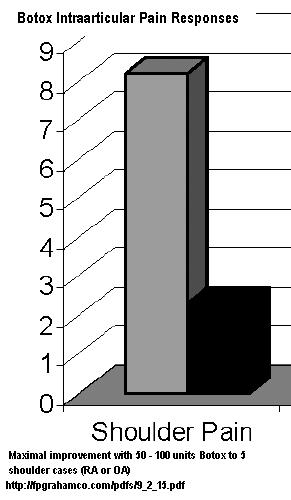
I suspect it could help other conditions like rotator cuff issues
6) Deal with any ankylosing spondylitis:
- Shoulder problems can occur in 1/4 cases of ankylosing spondylitis:
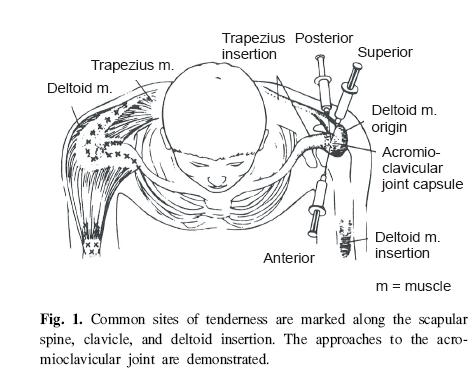
High prevalence of symptomatic enthesopathy of the shoulder in ankylosing spondylitis: Deltoid origin involvement constitutes a hallmark of disease
Robert G. W. Lambert et al. Arthritis Care & Research Volume 51 Issue 5, Pages 681 – 690
abstract here - NSAID’s (arthritis pills) may not cut it in treatment of Ank. Sp. In one review
JCCA J Can Chiropr Assoc. 2007 December; 51(4): 249–260. PMCID: PMC2077878
Ankylosing spondylitis: recent breakthroughs in diagnosis and treatment
Saeed A. Shaikh ref herethey state “In a German study conducted in 2000, there were 1080 AS patients who replied through questionnaires.- Seventy-eight percent had regularly taken NSAIDs for their disease 12 months prior to the study. 19.1% reported complete pain control, 26.8% reported pain reduction to one quarter, and a further 34.4% reported pain reduction to one half.
- However, over 20% of patients taking NSAIDs still reported insufficient pain control and more than 40% changed the NSAID due to lack of efficacy.
- One quarter of AS patients reported severe side effects from their treatment, most commonly abdominal pain, headache, dizziness, and nausea. The percentage of AS patients reporting changing their NSAID due to side effects ranged from 10.5% for celecoxib to 31.4% for indomethacin.“
- Methotrexate can be used, starting at 7.5 mg once weekly (with folic acid 5 mg/day) but may be doubled to 15 mg if lack of response to medication: Journal of Rheumatology, 22, 1104 – 1107, 1996; Methotrexate in severe ankylosing spondylitis: an open study article here another article here. However, a cochrane review is not so sure it works, (probably because lower doses don’t ?)
ref here - Pamidronate IV can give some relief but causes troubling myalgias/arthralgias after the first infusion in 2/3 of cases (and is $400 a shot)
A six-month randomized, controlled, double-blind, dose-response comparison of intravenous pamidronate (60 mg versus 10 mg) in the treatment of nonsteroidal antiinflammatory drug-refractory ankylosing spondylitis Walter P. Maksymowych, Gian S. Jhangri 1, Avril A. Fitzgerald 1, Sharon LeClercq 1, Peter Chiu 2, Alex Yan 2, Kenneth J. Skeith 2, Stephen L. Aaron 1, Joanne Homik 1, Paul Davis 1, Dale Sholter 2, Anthony S. Russell
Arthritis & Rheumatism Volume 46 Issue 3, Pages 766 – 773 abstract here“Pamidronate was administered at a dosage of either 60 mg/ml or 10 mg/ml in 500 ml of 5% dextrose over 6 hours for the first dose, and over 4 hours for subsequent doses.” – given monthly for 6 months. Noteworthy, in the study, people on Methotrexate and Sulfasalazine for ankylosing spondylitis were allowed to continue that medication, but people who had intraarticular steroid injections in the past 3 months were excluded as they could confuse results.
At 6 months, the ankylosing spondylitis disease activity was cut by 34.5%.
- Etanercept is becoming the mainstay of treatment for resistent cases of Ankylosing Spondylitis:
Arthritis Rheum. 2003 Jun;48(6):1667-75.
Six-month results of a double-blind, placebo-controlled trial of etanercept treatment in patients with active ankylosing spondylitis. Brandt J, Khariouzov A, Listing J, Haibel H, Sörensen H, Grassnickel L, Rudwaleit M, Sieper J, Braun J. full article here- However this disease is so active, one needs to stay on the drug: “After cessation of therapy, almost all patients experienced a relapse within a few weeks. Thus, it seems probable that etanercept must be administered continuously in most AS patients to achieve permanent inhibition of the inflammatory process.”
- Dose was Enbrel 25 mg vial injected twice weekly
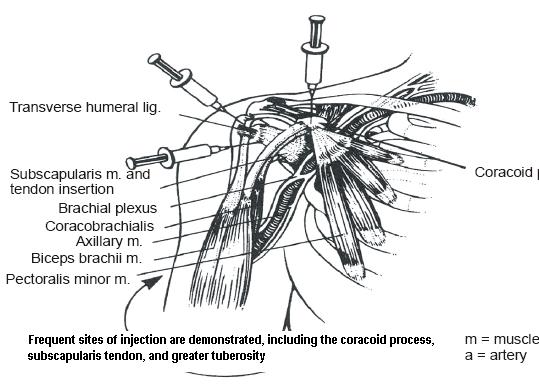
7) Check coracoid process (front shoulder bump) for additional sites of disease activity:
Enthesitis of Biceps Brachii Short Head and Coracobrachialis at the Coracoid Process: A Generator of Shoulder and Neck Pain
Karim, M Razul MD; Fann, Alice V. MD; Gray, Richard P. MD; Neale, David F. MD; Escarda, Jose Dan MD
American Journal of Physical Medicine & Rehabilitation:Volume 84(5)May 2005pp 376-380
“This series describes the outcome of diagnostic block at the coracoid process’s common origin of the biceps brachii short head and coracobrachialis for anterior shoulder pain and cervical myofascial pain syndrome in six patients. All showed significant tenderness over the tip of the coracoid process. All underwent diagnostic injection with Marcaine at the coracoid process, followed by therapeutic injection with Marcaine and DepoMedrol. All reported complete relief of pain after local injection. Enthesitis at the coracoid process needs to be considered as a causative or contributing factor in patients presenting with shoulder and neck symptoms. No study was found in the literature describing this association. Whether tendonitis of the common origin is a primary cause or result of chronic neck and shoulder dysfunction remains to be established.”
abstract repeated here
8) Check for Teres Minor tendonitis
Teres Minor Tendinitis Manifested with Chronic Myofascial Pain Syndrome in the Scapular Muscles A Case Report CF Wang, M Chen, MT Lin, TS Kuan, CZ Hong – Journal of Musculoskeletal Pain, 2006; 14(1): 39 – 43
abstract here
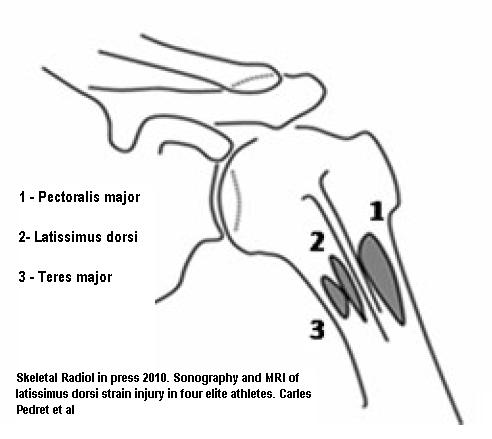
This sounds like a rare bird but I actually had a patient recently with psoariatic arthritis who had a flare with the shoulder being the worst. It seemed lower than the joint- in the deltoid and the upper triceps areas – working the area achieve zip until I injected the tender spastic insertion of the teres muscles on the humerus.
addendum – when you do that, you might be hitting tendons of lattisimus dorsi and pectoralis major some because they all course together:
8) Prolotherapy:
One reference to classic prolotherapy is:
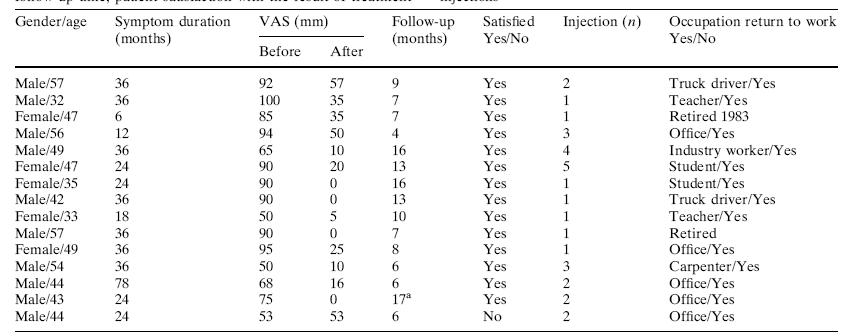
Daehyun Jo, Kyunga Ryu, Sunju Yang, Myounghee Kim
The Effects of Prolotherapy on Shoulder Pain
Korean J Anesthesiol 2004 May; 046(05): 589-592. article here (korean!)
- 15% dextrose was used. multiple sites
- Usually 3 treatments every 2-6 weeks are given but I can’t interpret text here.
- “RESULTS: For the 29 patients, prolotherapy proved to be effective and satisfactory in 83%”
I must admit, I have only used prolotherapy on unstable shoulders – this would be a new option.
9) Another Prolotherapy style Sclerotherapy targets the neurovascular painful “fuzz” that grows around injured tendons. this was a topic of discussion of another blog note here
Sclerosing polidocanol injections to treat chronic painful shoulder impingement syndrome-results of a two-centre collaborative pilot study Knee Surgery, Sports Traumatology, Arthroscopy
Volume 14, Number 12 / December, 2006, 1321-1326 Håkan Alfredson , Herlof Harstad, Simen Haugen and Lars Öhberg abstract here
- “Small volumes (0.2–0.4 ml, in total 1–2 ml) of the substances were injected into the areas of local vascularisation in the bursa wall and/or the supraspinatus tendon”
- “The patients were encouraged to start range of motion exercises the first day after treatment, but no heavy shoulder-loading activity was allowed during the first 2 weeks after the treatment. After 2 weeks there were no restrictions in the activity.”
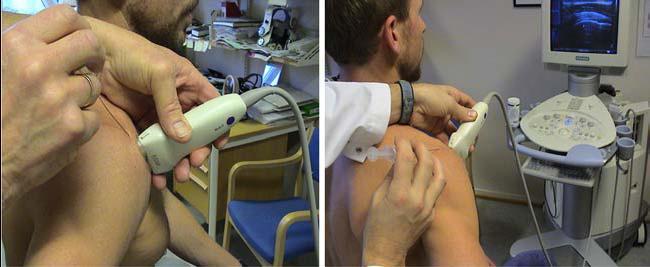
- “The patient is sitting, and the injection is performed from the cranio-dorsal side.”
Results: – sorry did not come out better – all except one were satisfied with results; 8 had 1 injection; 4 had 2; 2 had three; one had 4; and one had 5 shots.
- Enlarged blood vessels seen on US where not seen in contralateral shoulder.
- Max 5 injections
- assessment done at ~ 8 months so recovery took quite some time.
10) Don’t forget the neck – there will be segmental involvement of the neck and I use Intramuscular stimulation here. Subclinical or clinical radiculitis requires radiculitis treatments.
11) Deal with the unstable shoulder – a talk all in itself.
12) Physio exercise regimens
13) Laser, ultrasound
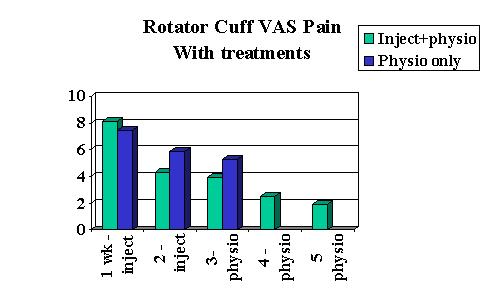
14) Old and unfit for any surgery? – pulsed radiofrequency
Kane, Timothy P.C. MRCS(Eng) a; Rogers, Peter FRCA b; Hazelgrove, Jane FRCA c; Wimsey, Simon MRCS(Ed) a; Harper, Gareth D. FRCS(Orth)
Pulsed radiofrequency applied to the suprascapular nerve in painful cuff tear arthropathy.
Source Journal of Shoulder & Elbow Surgery. 17(3):436-440, May 2008.
Abstract The purpose of this study was to assess the efficacy of pulsed radiofrequency (PRF) applied to the suprascapular nerve for pain relief in medically unfit patients with painful cuff tear arthropathy. Twelve patients with chronic shoulder pain due to cuff tear arthropathy were recruited. The mean age was 68 years (range, 60-83 years). The suprascapular nerve was targeted at the suprascapular notch with PRF. The patients were assessed with the Oxford score, Constant score, and visual analog scale (VAS) pain score before ablation and 3 and 6 months after ablation. Statistical analysis was undertaken by use of the Friedman test. Ten patients showed improvement in the VAS score (P = .24) and Constant score (P = .005) and eleven in the Oxford score (P = .001). There was a deterioration in the VAS scores between 3 and 6 months, suggesting that the benefits were starting to wear off with time (P > .05). We conclude that PRF may be a useful therapeutic adjunct in patients with painful, end-stage rotator cuff tear arthropathy who are medically unfit for surgery.
Addendum:
Pulsed radiofrequency to the suprascapular nerve was used in chronic shoulders in otherwise healthy patients in Turkey. Results were very incouraging:
PUlses were:
- not to exceed 42 º C
- 45 V intensity,
- 2 Hz frequency
- 20 milliseconds pulse width
- 120 second duration
- “with three times the width of wave period” (?repeated three times??)- not sure translation got that right…
Agri. 2009 Jan;21(1):16-21. Long-term results of suprascapular pulsed radiofrequency in chronic shoulder pain. Keskinbora K, Aydınlı I. article here (Turkish!)
The pain appears 1/3 of what it was as well (uses a crazy rating scale).
Their target is more lateral than I am used to:

Comment – sounds like dealing with the suprascapular nerve has a major impact and makes one think this could be a form of regional neuropathy combined with the neurovascular fuzz that grows around the tendon.
I would be interested in what others find helpful.
Addendum:
Came across the use of nitroglycerine patch to tendon as a treatment:
Am J Sports Med. 2005 Jun;33(6):806-13. Epub 2005 Apr 12.
Topical glyceryl trinitrate application in the treatment of chronic supraspinatus tendinopathy: a randomized, double-blinded, placebo-controlled clinical trial.
Paoloni JA, Appleyard RC, Nelson J, Murrell GA. abstract here
Patients were to apply “one quarter of a 5 mg/24-h GTN patch [Nitro-Dur,
Schering-Plough]” left on 24 hours and then changed for a new one.
Other therapy included:
(1) rest from aggravating activities in the early stages (particularly repetitive rotatory
movements of the shoulder and overhead or behind-the back activities that may cause impingement),
(2) daily range of motion exercises,
(3) daily stretching of the posterior shoulder capsule and pectoral muscles,
(4) a muscle strengthening program initially involving scapular retraction exercises and closed kinetic chain isometric exercises and gradually progressing to dynamic open kinetic chain isotonic resistance exercises.12
“Forty-six percent of patients in the GTN group reported their shoulders as asymptomatic with activities of daily living at the completion of the 6-month clinical trial. This result compares with 24% of patients in the placebo group.” – that’s double. Here’s the stats:
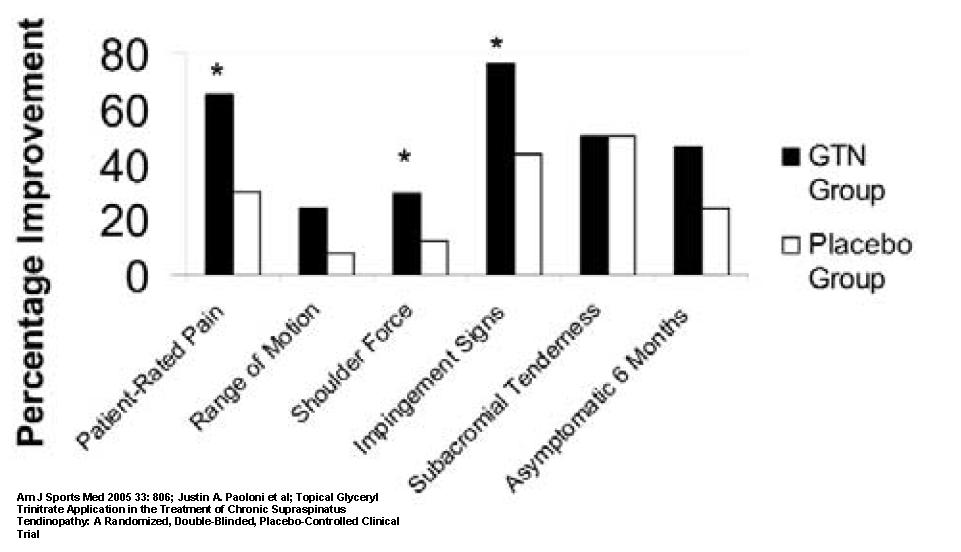
Headache was an issue and caused 8% to discontinue therapy…
Addendum:
Calcified nodules in the shoulder tendons are the most likely to get better with shots, and now it looks like the radiation therapy might help as well.
Strahlenther Onkol. 2010 Jan;186(1):18-23. Epub 2009 Dec 28.
Calcifying Tendonitis of the Shoulder Joint : Predictive Value of Pretreatment
Sonography for the Response to Low-Dose Radiotherapy.
Adamietz B, Schulz-Wendtland R, Alibek S, Uder M, Sauer R, Ott O, Keilholz L.They found different types of calcifications
Farin classification calcifying tendonitis type III – “diffuse” looking vague areas calcification
Farin Type I – discrete calcified nodules
“Radiotherapy was applied with an orthovolt machine (Stabilipan, Siemens) 250 kV, 15 mAs, 1-mm Cu filter, tubus size 10 × 15 cm, focus-skin distance 40 cm with two opposed fields. The single dose was 0.5 Gy, two to three fractions per week to a total dose of 3.0 Gy. After a break of 6 weeks treatment was continued with a second series of 3.0 Gy. We paid careful attention to the protection of the gonads, thyroid gland, and breast tissue.”
Results:
Unterschied zwischen Farin-Typ I und III (p = 0,01).
Response to RT Complete pain Partial pain No response
relief relief:
| all better | partially | no response
Farin type I(n = 11) | 5 | 3 | 3
Farin type III(n = 18) | 18 | 0 | 0
Comment – diffuse calcifications are always better – which is why I presume you have to mechanically break up hard lump ones… Now If one could just find a radiotherapist willing to work on non-cancer cases..

Wow, who would of known. My doctor just prescribed arthritis pills as a treatment, and it didnt really work.
Very Interesting Article, Thanx
Pingback: Co nowego w leczeniu Sore, Bolesna Hands, palców i nadgarstków? | Joint Specialist
Pingback: Pain Medical Musing » Blog Archive » Shoulder Pain Patient Needs Help - Any Suggestions?
Your article has all information about Resistant Shoulder Tendonitis Treatments. I read your article for three hours. It is very interesting. I can’t stop reading it. I have learned a lot of things on your blog. Keep posting this kind of blog.
Pingback: The Missing Aspects of Tennis Elbow Treatment – Axillary and Scapular Triggers to Treat Segmental Hypersensitivity | Pain Medical Musing
Very great post. I just stumbled upon your blog and wanted to mention that I have
really enjoyed browsing your weblog posts. In any case I will be subscribing on
your rss feed and I am hoping you write once more soon!