Recent study of neuropathic pain in leg associated with back pain, in a primary care setting, found MRI evidence of nerve root impingement unlikely and straight leg testing useless. Their conclusion: “[the] neuropathic pain may be caused by irritation of nervous tissue which is not directly identifiable on MRI as impingement or compression.” Confirms how useless mri’s are in certain cases of sciatica and how unreliable staight leg raise test is as well.
PAIN 152 (July, 2011) 1511–1516
Identifying neuropathic back and leg pain: A cross-sectional study
Iain D. Beith a,⇑, Andrew Kempb, Jonathan Kenyon c, Matthew Prout d, Thomas J. Chestnut abstract here
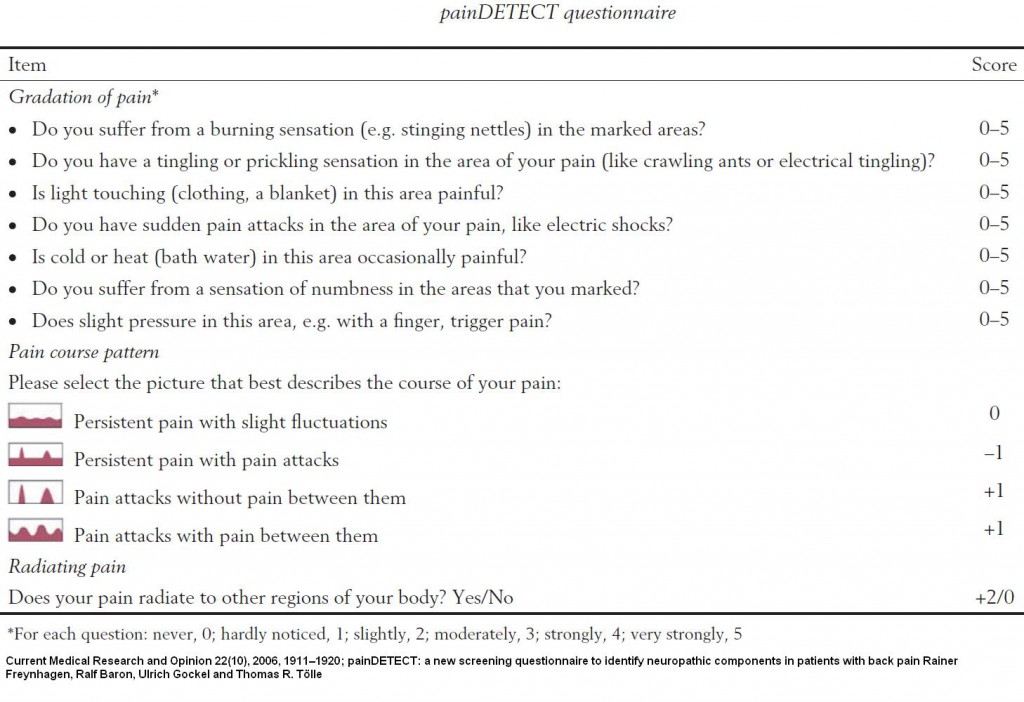
Used the Pain_DETECT questionnaire to determine neurogenic capacity:
Printable form
>score ≤ 12, a neuropathic component is unlikely (< 15%); score ≥ 19, a neuropathic component is likely (> 90%).
Current Medical Research and Opinion 22(10), 2006, 1911–1920
painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain
Rainer Freynhagen, Ralf Baron, Ulrich Gockel and Thomas R. Tölle abstract here
- 347 cases
- 204 (59%) reported likely nociceptive pain,
- 85 (25%) reported a mixture of symptoms leading to an unclear grouping
- 54 (16%) reported likely neuropathic pain
- Straight leg raising was only reduced 10 degrees in the back and leg pain cases (50-55 versus 60-65)
Pain. 2008 Mar;135(1-2):65-74.
Pseudoradicular and radicular low-back pain–a disease continuum rather than different entities? Answers from quantitative sensory testing.
Freynhagen R, Rolke R, Baron R, Tölle TR, Rutjes AK, Schu S, Treede RD abstract here
The answer was found years ago by Dr. Chen Gunn of Vancouver:
J Bone Joint Surg Am. 1976 Sep;58(6):815-25.
Tenderness at motor points. A diagnostic and prognostic aid for low-back injury.
Gunn CC, Milbrandt WE.
In patients with low-back injury the motor points of some muscles may be tender. Of fifty patients with low-back “strain”, twenty-six had tender motor points and twenty-four did not, while forty-nine of fifty patients with radicular signs and symptoms suggesting disc involvement had tender motor points, and the one without uch tender points had a hamstring contusion which limited straight leg raising. Of fifty controls with no back disability, only seven had mild tender points after strenuous activity, while forty-six of another fifty controls with occasional back discomfort had mild motor-point tenderness. In all instances the tender motor points were located in the myotomes corresponding to the probable segmental levels of spinal injury and of root involvement, when present. Patients with low-back strain and no tender motor points were disabled for an average of 6.9 weeks, while those with the same diagnosis but tender motor points were disabled for an average of 19.7 weeks, or almost as long as the patients with signs of radicular involvement, who were disabled for an average of 25.7 weeks. Tender motor points may therefore be of diagnostic and prognostic value, serving as sensitive localizers of radicular involvement and differentiating a simple mechanical low-back strain from one with neural involvement.Subtle radiculitis is associated with triggers that correspond to the nerve root level involved. It only has taken 35 years to potentially confirm his findings – he was way ahead of his time.
Needling these muscles and the back speeds the recovery in what Dr. Gunn called Intramuscluar Stimulation (IMS).
After I read his articles at the time, I made certain to take training with him and was among the first group to train with him.
I have 2 present cases with neuropathic level pains in leg with back pain. Straight leg raising is not significantly effected but the disability was real. I have wondered whether an MRI would be useful – now it appears probably not.
There continues to be the insurance company gimmick that if nothing is found on MRI, nothing can be the matter. I have written several articles on how this is not so. Such case workers needs to be reported to their superior and their college and have all their prior cases re-evaluated.
Previous articles on uselessness of MRI’s include:
People With Longstanding Lumbar Nerve Root Problems Have “MRI Invisible” Lesions
