Methotrexate is a fairly safe medication but studies of it solo have failed to help Ankylosing spondylitis. Chinese study found when used with methylprednisolone had a therapeutic effect and improved inflammatory markers.
Observation of the curative effect of methylprednisolone combined with methotrexate in the treatment of ankylosing spondylitis and its regulating effect on patients’ serum interleukin-17/ interleukin-4
Xinzheng LI; Lei JING; Bing ZHANG.
Chinese Journal of Postgraduates of Medicine ; (36): 921-925, 2021.
https://pesquisa.bvsalud.org/portal/resource/pt/wpr-908700
- 117 cases
Treatment:
methylprednisolone – usually given IV;
According to:
Wong EC, Brown G. Does pulse dosing of methylprednisolone have an acute effect on serum creatinine concentrations?
Can J Hosp Pharm. 2014 Nov;67(6):458-9
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4275145/
“A typical pulse regimen ranges from 500 to 1000 mg IV daily for 2–4 consecutive days”
Article is unavailable but suspect it would be 1 gm x 3 days which I have seen as standard
How often I suspect would depend on response but monthly has been used in CIDP
Methotrexate – still not clue on dose but suspect would be 1-1.5 gm weekly with folate
Enbrel and designer ‘Mab” drugs are regulated for rheumatologists to use but these specialists fail to recognize nonradiologic axial spondyloarthritis. I have found this to be quite painful for someone told they just have “Fibromyalgia” but has inflammatory symptoms.
one author for more widespread disease criteria included:
Roychowdhury, B., et al.
Is methotrexate effective in ankylosing spondylitis?.
Rheumatology 41.11 (2002): 1330-1332.
https://academic.oup.com/rheumatology/article/41/11/1330/1788035?login=false
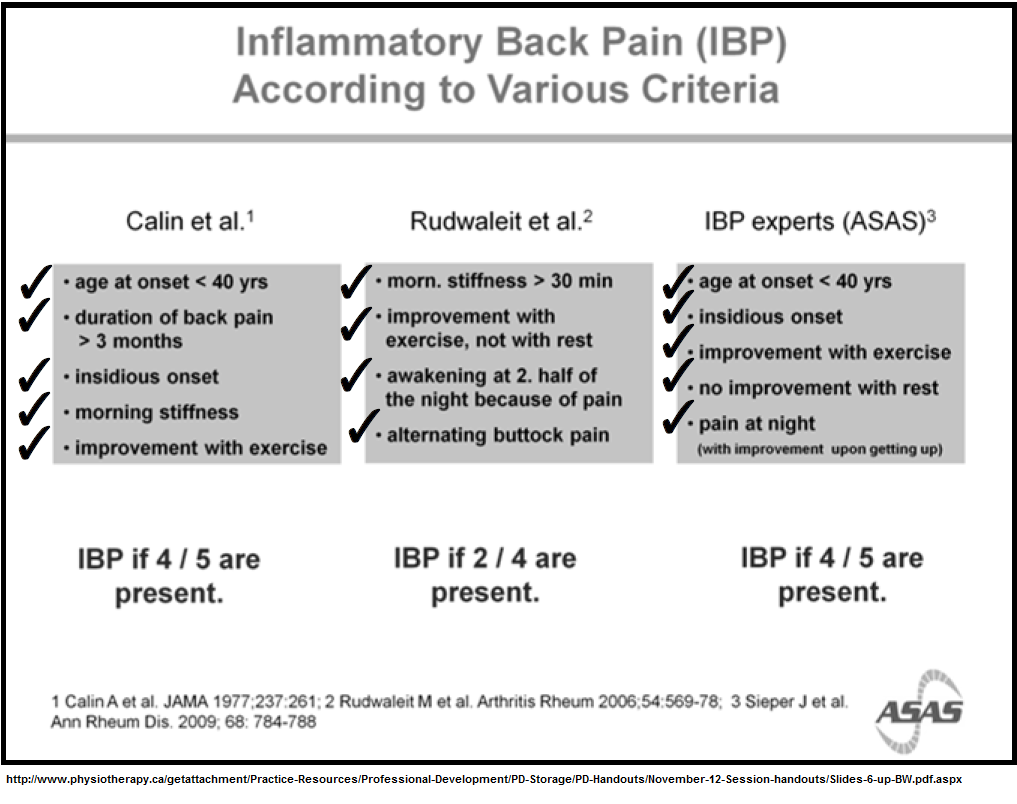
(i) morning stiffness of at least 30 minutes;
(ii) disturbed sleep due to pain and stiffness;
(iii) peripheral arthritis;
(iv) ESR >30 mm in the 1st hour, or CRP >20 mg/l;
(v) spinal pain; and
(vi) pain in both buttocks during the day or night.
IV methylprednisolone is very time consuming and very hard on veins which led to the substitution of oral dexamethasone instead:
here it was substituted for pulse IV in cases of Chronic Demyelinating Inflammatory Polyneuropathy- it has now become standard treatment:
Molenaar, D. S., P. A. Van Doorn, and M. Vermeulen.
Pulsed high dose dexamethasone treatment in chronic inflammatory demyelinating polyneuropathy: a pilot study.
Journal of Neurology, Neurosurgery & Psychiatry 62.4 (1997): 388-390.
https://jnnp.bmj.com/content/jnnp/62/4/388.full.pdf
- They used 40 mg orally a day for 4 days every 4 weeks – I gave dexamethasone 4 mg – 4 am, 3 afternoon, 3 evening = 10/day.
- This dosage is hard on the nerves and sleep so I often prescribe Alprazolam 0.5 mg 1/2 – 1 three times as needed daily during four day course (surprised how many people who thought they didn’t need it grateful for it)
A four day pulse monthly does not seem to impact on bone density..
Methotrexate alone may have little effect on Ankylosing spondylitis:
Roychowdhury, B., et al.
Is methotrexate effective in ankylosing spondylitis?.
Rheumatology 41.11 (2002): 1330-1332.
https://academic.oup.com/rheumatology/article/41/11/1330/1788035?login=false
“oral methotrexate 10 mg weekly, or placebo, for 24 weeks”
“In this 24 week, double‐blind, placebo‐controlled study of methotrexate in AS, there did not appear to be a significant benefit of methotrexate treatment compared with placebo”
though there might be responders as they had to admit:
“This is in contrast to two small open studies that suggested methotrexate might improve clinical symptoms [7, 8]”
7) Sampaio‐Barros PD, Costallat LT, Bertolo MB, Neto JF, Samara AM. Methotrexate in the treatment of ankylosing spondylitis.
Scand J Rheumatol 2000 ;29 :160–2.
https://www.tandfonline.com/doi/abs/10.1080/030097400750002021?journalCode=irhe20
they used injectable IM 12.5 mg weekly over a period of a year. 53% responders. side effects: 23 patients (68%) “side effects which included dyspeptic syndrome, transient elevation of liver enzymes, and dizziness”
studies showed subcut levels are 14% higher than oral making it at least 14.25 mg orally so it might be said 10 mg double blind study using 10 mg was under-dosed. It is a bit odd when current suggestions are for RA:
https://www.cadth.ca/sites/default/files/pdf/htis/may-2011/RC0265_Methotrexate_for_Rheumatoid_Arthritis_final.pdf
“Oral methotrexate should be started at 10-15 mg/week, with escalation of 5 mg every 2-4 weeks up to 20-30 mg/week, depending on clinical response and tolerability; parenteral administration should be considered in the case of inadequate clinical response or intolerance.”
Should study have increased the dose in non-responders at 2 weeks? Given poor response of 10 mg in their study, should they have started doses at 15 mg?
8) Biasi D, Carletto A, Caramaschi P, Pacor ML, Maleknia T, Bambara LM. Efficacy of methotrexate in the treatment of ankylosing spondylitis: a three‐year open study.
Clin Rheumatol 2000;19:114–7.
https://www.academia.edu/download/47292270/s10067005002720160717-27290-12nikyn.pdf
“Methotrexate (7.5–10 mg/week) was administered for 3 years.”
“We obtained a good and relatively prompt clinical response except for peripheral arthritis and iridocyclitis”
Comment – I see methotrexate has been combined with more 4th generation agents but steroid pulses this would be a cheap and simple possibility. Sounds like methotrexate should be started at 15 mg/day. I will write Chinese author and ask for dose specifics and response rates..
