Chronic diseases with negative “blood work” might in fact be a cytokine inflammation disease. Moderate fibromyalgia has now be found to be a cytokine inspired disease.
I wrote about importance of cytokines 12 years ago:
Cytokine Inflammation Diseases Will Be the Diseases of the 21st Century
http://painmuse.org/?p=361
Then connection to multiple diseases were seen (headaches, irritable bowel, diabetes, alzheimer’s, chronic pancreatitis, chronic fatigue, depression and now depression.
Back in 2013 I wrote a draft that was never published:
“Could Elevated Cytokines Become a Test For Fibromyalgia (FM)?” Now it has.
Below is an update on tests in Fibromyalgia and cytokine relation
Straub, Liza, and Anne Mounsey.
FM/a blood test for diagnosis of fibromyalgia.
American Family Physician 103.9 (2021): 566-567.
https://www.aafp.org/pubs/afp/issues/2021/0501/p566.html
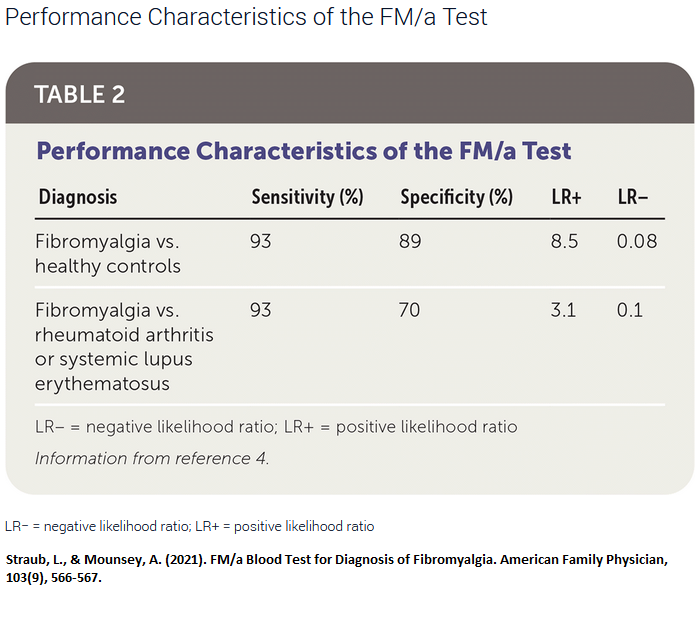
“A study of 160 patients with fibromyalgia based on the American College of Rheumatology criteria and 119 healthy control patients found that a positive FM/a Test result has a sensitivity of 93% and a specificity of 89% (Table 2).4 The positive likelihood ratio was 8.5, and the negative likelihood ratio was 0.08. However, this type of study design, which uses a control group of healthy patients, overestimates accuracy. In the same study, when using a more appropriate comparison group of patients with known rheumatoid arthritis (RA) or systemic lupus erythematosus (SLE) who did not have co-occurring fibromyalgia, the specificity was only 70%, with a positive likelihood ratio of 3.1 and a negative likelihood ratio of 0.1. The most appropriate study design would enroll patients with clinically suspected fibromyalgia, but this type of study has not been performed.”
 They based their review on:
They based their review on:
Wallace DJ, Gavin IM, Karpenko O, et al.
Cytokine and chemokine profiles in fibromyalgia, rheumatoid arthritis and systemic lupus erythematosus: a potentially useful tool in differential diagnosis
Rheumatol Int. 2015;35(6):991-996.
https://link.springer.com/article/10.1007/s00296-014-3172-2
Cytokines have been used in treatments on humans (interferon) and also causes:
- depression and fatigue
- insomnia
- psychomotor slowing
- cognitive impairment
A review of their negative effects is here:
Felger JC, Miller AH. Cytokine effects on the basal ganglia and dopamine function: the subcortical source of inflammatory malaise.
Front Neuroendocrinol. 2012 Aug;33(3):315-27.
doi: 10.1016/j.yfrne.2012.09.003.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3484236/pdf/nihms409347.pdf
comment – differentiation with rheumatoid was less because both are inflammatory diseases. Morning stiffness is bad with both and always bemused my diagnosis in the past. The test at time costed over $1000 US. Remember these were cases of moderate+ FM so unknown how positive in milder cases (please correct me if I am wrong)
EpicGenetics will do it and claim covered by USA medicare
https://www.fmtest.com/
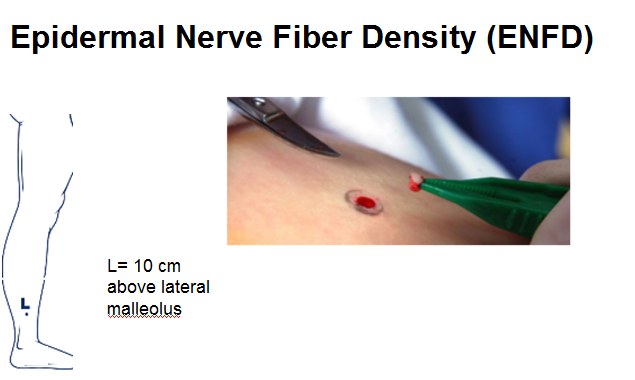
In Canada, until it is available, FM patients may continue to gain no respect. 40% of FM is a small fiber neuropathy which is potentially diagnosable by skin biopsy of the ankle. This test is available in Saskatchewan. IN the USA, Therapath will run the test but used to cost $700.
 addendum – What is going to become important now are Janus Kinase inhibitors that inhibit cytokines:
addendum – What is going to become important now are Janus Kinase inhibitors that inhibit cytokines:
Choy EH.
Clinical significance of Janus Kinase inhibitor selectivity.
Rheumatology (Oxford). 2019 Jun 1;58(6):953-962.
doi: 10.1093/rheumatology/key339
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6532440/
“Oral JAK inhibitors (JAKi) have been developed as anti-cytokine therapy in RA (rheumatoid arthritis). Two JAKi, tofacitinib and baricitinib, have been approved recently for the treatment of RA, and many JAKi are currently in development.”
I have yet to see its use in Fibromyalgia as still early use in Rheumatoid
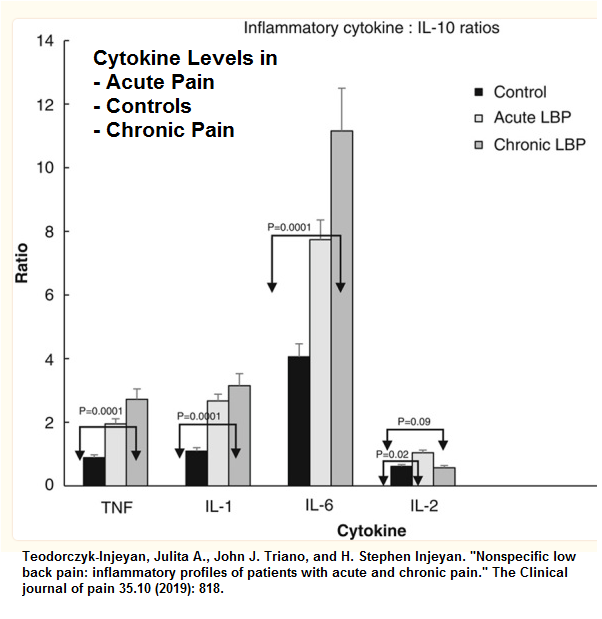
Even chronic back pain has a cytokine connection:
Chronic Back pain is associated with elevations of Tumor Necrosis Factor and
Interleukin 6:
Teodorczyk-Injeyan, Julita A., John J. Triano, and H. Stephen Injeyan.
Nonspecific low back pain: inflammatory profiles of patients with acute and chronic pain.
The Clinical journal of pain 35.10 (2019): 818.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6735949/