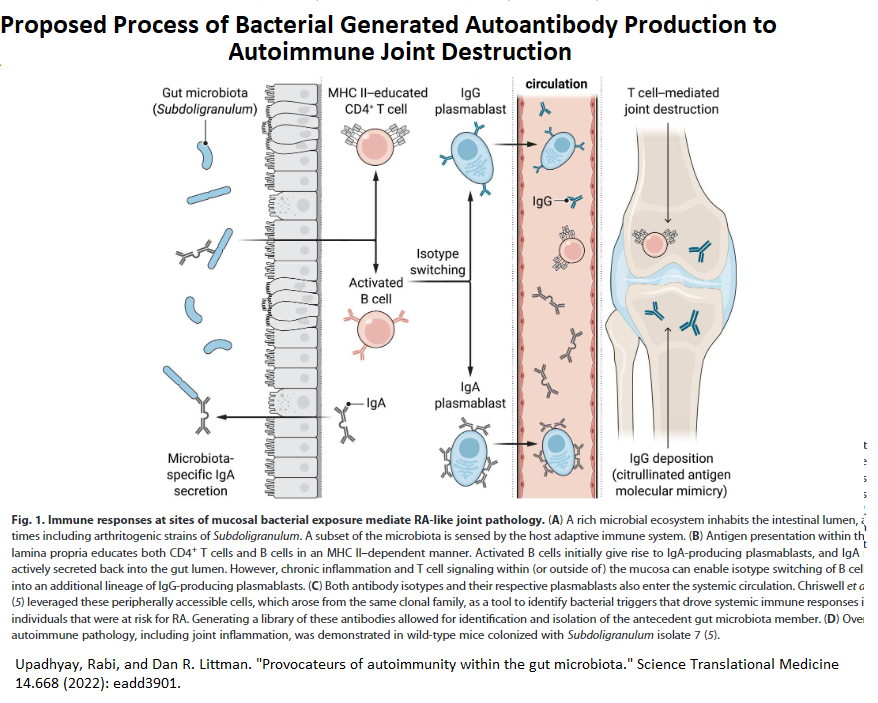
Recent Study found a strain of previously unrecognized strain of Subdoligranulum in gut was associated with Rheumatoid arthritis (RA) autoantibodies. This bacterium, if introduced into guts of mice, replicated the arthritis seen in humans. This strain is only seen in RA victims.
So, both gut bacterial and periodontal disease can potentially trigger antimmune responses. This leads to new implications on prevention and treatment of Rheumatoid arthritis.
Chriswell, Meagan E., et al.
Clonal IgA and IgG autoantibodies from individuals at risk for rheumatoid arthritis identify an arthritogenic strain of Subdoligranulum.
Science Translational Medicine 14.668 (2022): eabn5166.
https://www.science.org/doi/abs/10.1126/scitranslmed.abn5166
- Bacteria or antibodies related to this bacteria found in 20% of RA victims and not in normal subjects
- bacteria put into guts of rodents will induce RA looking disease
Author discusses it here:
Newly discovered gut bacteria may be a culprit behind rheumatoid arthritis
https://bigthink.com/health/gut-bacteria-arthritis/
He is not convinced eradicating bacteria will help but preventing it might prevent it from occurring so I suspect stool test will eventually be devised.
Also recently, periodontal disease has been linked to RA
Porphyromonas gingivalis (Pg), a periodontal pathogenic bacterium, can induce anti- citrullinated protein antibody (ACPA)which “forms an immune complex with citrullinated proteins in the joints, thereby inducing arthritis”. ”
ACPA is a main marker of RA with a sensitivity of 70% and specificity of 90%. Previous studies reported that serum immunoglobulin G (IgG) antibody titer to Pg was significantly higher in patients with RA than that in those without RA.”
It was concluded ” Pg infection may be considered to be associated with ACPA-positive RA. In addition, the severity of periodontitis has been reported to be significantly associated with RA activity.”
Periodontitis is a bad disease linked to heart disease:
giMougeot, JL C., et al.
Porphyromonas gingivalis is the most abundant species detected in coronary and femoral arteries.
Journal of oral microbiology 9.1 (2017): 1281562.
https://www.tandfonline.com/doi/abs/10.1080/20002297.2017.1281562
This was a confirmation of an earlier study:
Kozarov, Emil V., et al.
Human atherosclerotic plaque contains viable invasive Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis.
Arteriosclerosis, thrombosis, and vascular biology 25.3 (2005): e17-e18.
https://www.ahajournals.org/doi/full/10.1161/01.atv.0000155018.67835.1
and alzheminer’s:
Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors
Stephen S. Dominy et al
Science Advances 23 Jan 2019: Vol. 5, no. 1, eaau3333
DOI: 10.1126/sciadv.aau3333
http://advances.sciencemag.org/content/5/1/eaau3333
RA patients might need to see dentist/periodontist. Smoking is a big no-no.
Antibiotics have been proven helpful in RA
Antibiotics, particularly clarithromycin, tetracyclines and flouroquinolones, have been shown to be beneficial:
Ogrendik, Mesut.
Antibiotics for the treatment of rheumatoid arthritis.
International journal of general medicine 7 (2014): 43.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3883615/
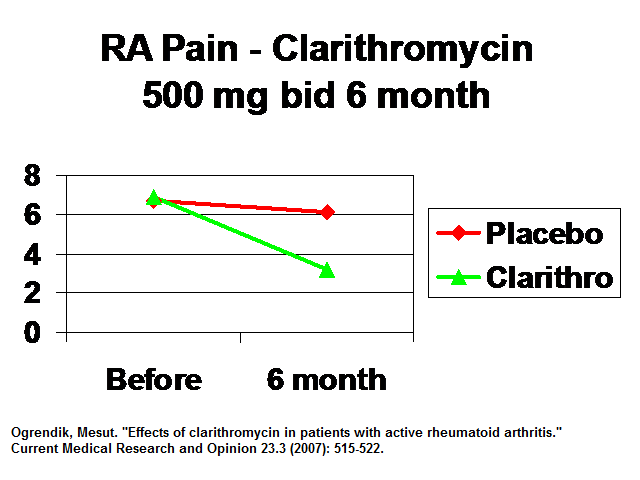
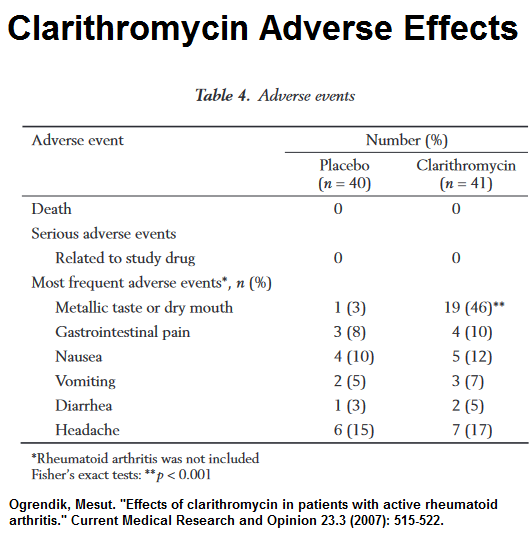
Clarithromycin effects in a early RA solo study:
Ogrendik, Mesut. “Effects of clarithromycin in patients with active rheumatoid arthritis.” Current Medical Research and Opinion 23.3 (2007): 515-522.
https://www.tandfonline.com/doi/abs/10.1185/030079906X167642
- early RA vs placebo
- clarithromycin 500 mg od 6 months
- Pains drop to 1/2
Side Effects – metallic or dry mouth but nil else.
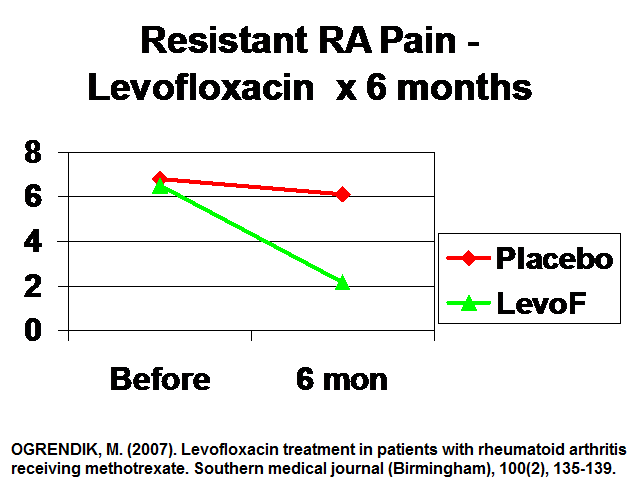
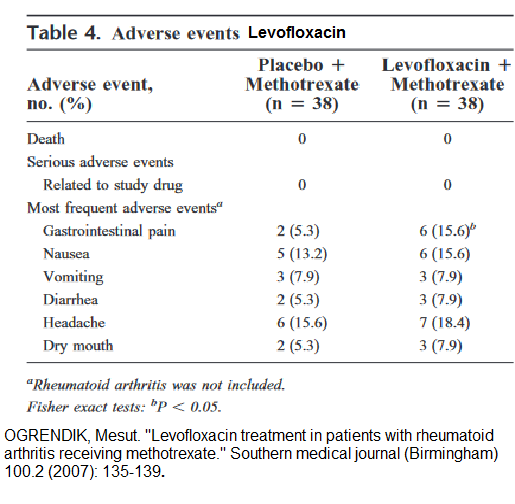
 Levofloxacin
Levofloxacin
Ogrendik, Mesut. “Levofloxacin treatment in patients with rheumatoid arthritis receiving methotrexate.”
Southern medical journal 100.2 (2007): 135-140.
https://pubmed.ncbi.nlm.nih.gov/17330681/
- Resistant RA – “76 patients with persistently active rheumatoid arthritis despite at least 6 months of methotrexate therapy at a stable dose of 15 to 25 mg per week”
- levofloxacin (500 mg) or placebo orally once daily
Results – cuts pain to 1/3 in Resistant Cases:
 Adverse effects vs methotrexate alone:
Adverse effects vs methotrexate alone:
 Potentially serious side effects include and probably preclude chronic use though I have had to use it in chronic prostatitis for 3 weeks- 3 months.
Potentially serious side effects include and probably preclude chronic use though I have had to use it in chronic prostatitis for 3 weeks- 3 months.
- irreversible peripheral neuropathy
- spontaneous tendon rupture and tendonitis
- QT prolongation/torsades de pointes.( do ECG before start?)
Minocycline
O’Dell, James R., et al.
Treatment of early Rheumatoid Arthritis with minocycline or placebo. Results of a Randomized, double‐blind, placebo‐controlled trial.
Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 40.5 (1997): 842-848.
http://okmicro.sakura.ne.jp/Abt/MinocyclineERA1.pdf
Results about 1/2 better functioning
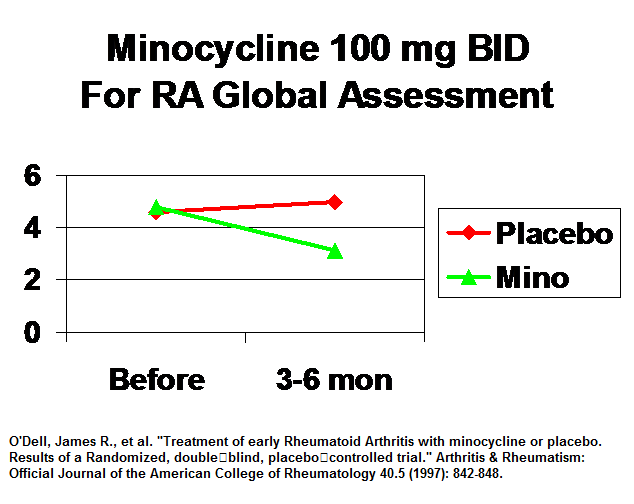 Side effects minimal though I have seen a case of jaundice from minocycline for acne.
Side effects minimal though I have seen a case of jaundice from minocycline for acne.
another article reported “common side effects can be seen in up to 18% of patients. These include photosensitivity, hyperpigmentation, dizziness, nausea, headache, tinnitus, diarrhea, and abdominal pain.” Risk of Clostridium difficile infection is low.
Heydari-Kamjani, Milad, Michelle Demory Beckler, and Marc M. Kesselman. Reconsidering the use of minocycline in the preliminary treatment regime of rheumatoid arthritis.
Cureus 11.8 (2019).
https://www.cureus.com/articles/19619-reconsidering-the-use-of-minocycline-in-the-preliminary-treatment-regime-of-rheumatoid-arthritis#references
Azithromycin no benefit at 3 months:
Kvien, T. K., et al. “Three month treatment of reactive arthritis with azithromycin: a EULAR double blind, placebo controlled study.” Annals of the Rheumatic Diseases 63.9 (2004): 1113-1119.
https://ard.bmj.com/content/annrheumdis/63/9/1113.full.pdf
Comment – they used 1 gm weekly for 12 weeks. I used 500 mg bid x3 days then 500 mg twice weekly in a severe neck pains with benefit and also suspect in RA more than 3 months is needed. Giving meds once weekly, is just asking for resistance to follow easily, as levels will be significantly low by end of week…
Doxyxycline no benefit
van der Laan W, Molenaar E, Ronday K, et al.: Lack of effect of doxycycline on disease activity and joint damage in patients with rheumatoid arthritis. A double blind, placebo controlled trial . J Rheumatol. 2001, 28:1967-74.
|https://www.jrheum.org/content/28/9/1967.short
though ran for only 3 months 50 mg bid
Comment – Being older, I now brush, floss and mouth wash twice daily. I have any dental problems attended to.
I believe that many chronic diseases will turn out to be infection related like the recent association of Multiple Sclerosis and Mononucleosis:
Soldan, Samantha S., and Paul M. Lieberman. “Epstein–Barr virus and multiple sclerosis.” Nature Reviews Microbiology (2022): 1-14.
https://www.nature.com/articles/s41579-022-00770-5
Problem relates to Rheumatoid arthritis – will bacterial positive cases be the new “Tuberculosis-like” pariahs? Will triple antibiotic treatments like those for Helicobacter infections be used? Given only 20% of cases of stool site study had this organism either it was cleared or other factors like dental are implicated suggesting shutting off the bacteria by itself will not necessarily help the disease.
Antibiotic resistance is going to be an issue. A case of RA induce with bacterial endocarditis resolved with effective treatment of endocarditis with intravenous ceftriaxone.
Mukherjee A, Jantsch V, Khan R, et al.
Rheumatoid arthritis-associated autoimmunity due to aggregatibacter actinomycetemcomitans and its resolution with antibiotic therapy.
Front Immunol. 2018, 9:2352. 10.3389/fimmu.2018.02352
https://www.frontiersin.org/articles/10.3389/fimmu.2018.02352/full
Given recent article suggestion to use Minocycline,
Heydari-Kamjani, Milad, Michelle Demory Beckler, and Marc M. Kesselman. Reconsidering the use of minocycline in the preliminary treatment regime of rheumatoid arthritis.
Cureus 11.8 (2019).
https://www.cureus.com/articles/19619-reconsidering-the-use-of-minocycline-in-the-preliminary-treatment-regime-of-rheumatoid-arthritis#references
in fresh cases of RA, minocycline 100 mg bid should probably be tried to damping any contributing bacterial infection. Chlarithromycin is a backup plan. In methyltrexate resistant RA cases, I would be tempted to use levofloxacin…
However doctors are very slow to change so getting them to buy into bacterial infection might take some doing:
https://getpocket.com/explore/item/to-fix-the-social-sciences-look-to-the-dark-ages-of-medicine?utm_source=pocket-newtab
Interesting point here: treatment of back pain with clavulin 500 mg tid results – look familiar?
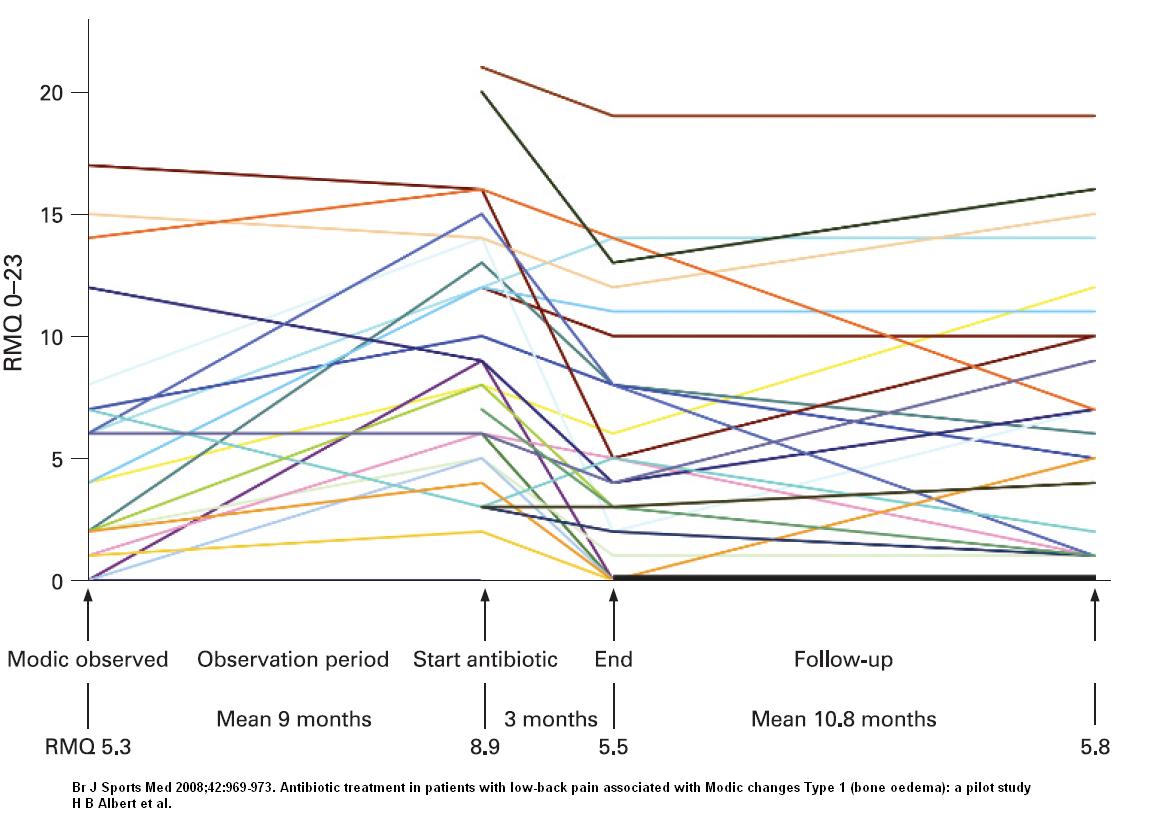
Perhaps clarithromycin 500 mg bid x6 month should be used there… (not sure how effective minocycline is to p.acne)…