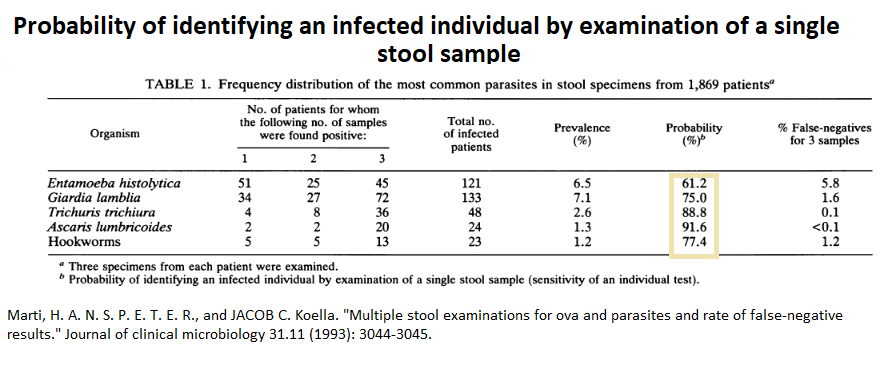
People who come in with recently developed chronic diarrhea are a challenge. Reliance on stool tests might be suspect if just relying on Ova and Parasite micro exam. Given excretion is episodic, O&P testing by microscopy would miss 39% of amebiasis and 25% of giardiasis. Even the antigen tests could miss 10+%. This leads to plan B – Metronidazole treatment as a viable option but could still not help up to 30% of cases.
Marti, H. A. N. S. P. E. T. E. R., and JACOB C. Koella.
Multiple stool examinations for ova and parasites and rate of false-negative results.” Journal of clinical microbiology 31.11 (1993): 3044-3045.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC266208/pdf/jcm00023-0218.pdf
- “Each specimen was fixed in SAF fixative [ sodium acetate-acetic acid-formalin] and concentrated as described by Yang and Scholten (3). The sediment was then microscopically examined for ova and parasites by experienced laboratory technicians”
Results:
 In biopsy taken cases, pick up is only 50%:
In biopsy taken cases, pick up is only 50%:
Shen M (Jasmine), Voltaggio L, Robertson S.
Giardia Is Often Overlooked on Histopathologic Examination: A High-Volume, Single-Institution Experience. International Journal of Surgical Pathology. 2021;29(3):257-262. doi:10.1177/1066896920947795
Such pathetic results had led me to just treat chronic diarrhea cases with metronidazole.
One suggested treatment for giardiasis with metronidazole has been;
PRESCRIBING INFORMATION METRONIDAZOLE
https://www.aapharma.ca/downloads/en/PIL/2019/Metronidazole_EN_PI.pdf
“One 250 mg tablet twice daily for 5 to 7 days”
This is confirmed here:
Argüello-García, Raúl, et al.
Drug resistance in Giardia: mechanisms and alternative treatments for giardiasis.
Advances in Parasitology 107 (2020): 201-282.
https://www.researchgate.net/profile/Andre-Buret/publication/338186289_Pathogenesis_and_post-infectious_complications_in_giardiasis/links/600731f5a6fdccdcb8688893/Pathogenesis-and-post-infectious-complications-in-giardiasis.pdf#page=216
“maximum of 750 mg/day orally in three doses for 5–10 day”
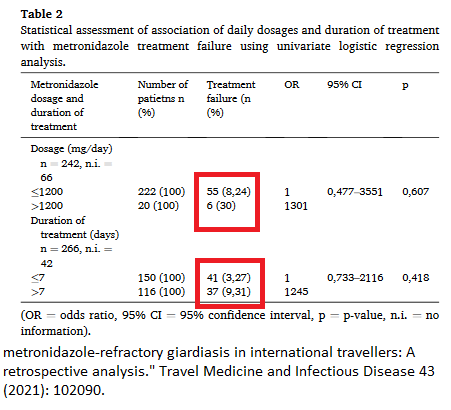
However German experience found a 24-30% failure rate:
Tanja E. Peters, Benno Kreuels, Marylyn M. Addo, Egbert Tannich, Camilla Rothe,
Risk factors for and management of metronidazole-refractory giardiasis in international travellers: A retrospective analysis,
Travel Medicine and Infectious Disease,Volume 43, 2021,102090,
https://www.sciencedirect.com/science/article/abs/pii/S1477893921001319
It was mentioned once that metronidazole works best on the trophozoite organisms and not on the cysts. So what does one do with resistant cases?
Tinidazole has been used for resistant cases:
Cenkowski, Monica, et al.
Metronidazole-resistant trichomoniasis: Two Canadian cases.
Official Journal of the Association of Medical Microbiology and Infectious Disease Canada 6.1 (2021): 63-68.
https://jammi.utpjournals.press/doi/pdf/10.3138/jammi-2020-0044?download=true
but according to google:
” Is tinidazole available in Canada? pre-formulated tinidazole is not available in Canada; therefore, only compounded tinidazole can be used.”
above link used: “oral tinidazole 2 g once daily for 5 days, which is only available in compounded form from a specialized compounding pharmacy.”
Comment – giardia can be carried by Canada geese. They crap all over our parks and it has been a concern to me.
Chronic giardiasis can mimic irritable bowel syndrome – in:
Chester, Alexander C., et al.
Giardiasis as a chronic disease.
Digestive diseases and sciences 30.3 (1985): 215-218.
https://www.academia.edu/download/72297774/bf0134788620211012-6461-1hh2equ.pdf
“The m e a n duration o f symptoms was 3.3 years. When compared to acute giardiasis, an increased frequency o f constipation and upper gastrointestinal complaints was noted in the chronic population.”
In:
Bartelt, Luther A., and R. Balfour Sartor. ”
Advances in understanding Giardia: determinants and mechanisms of chronic sequelae.” F1000prime reports 7 (2015).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4447054/pdf/biolrep-07-62.pdf
In adults, cognitive impairment and chronic fatigue are mentioned as well as “immunologic phenomena (reactive arthritis, inflammatory ocular manifestations, and urticaria) that are not necessarily dependent on severity of diarrheal manifestations and may persist even beyond detection of the parasite.”
Unwell with diarrhea? As initial mentioned, you could be in trouble relying on testing.
Microscopic exam is done by provincial labs but only in certain circumstances:
https://rrpl-testviewer.ehealthsask.ca/Home/Details?id=65
“NOTE: Relevant history is required for an Ova and Parasite Exam. The Microbiology requisition lists the following as relevant:
∙Travel/immigration outside Canada or U.S. within the last 2 years (state when and where)
∙immunosuppressed
∙suspected helminth infection (other than Enterobius vermicularis)
∙eosinophilia
∙age <13 years
∙symptoms >2 weeks
∙unsafe food/water
∙prior parasite
∙case contact
∙other (must provide reason)
NB: Diarrhea is NOT adequate history for performing an O&P examination.”
Giardia antigen testing is available:
https://rrpl-testviewer.ehealthsask.ca/Home/Details?id=530
The Newer tests available are described here:
Al, Funda Doğruman, et al.
The use of enzyme linked immunosorbent assay (ELISA) and direct fluorescent antibody (DFA) methods for diagnosis of Giardia intestinalis.
Turkiye Parazitol Derg 30.4 (2006): 275-8.
https://tparazitolderg.org/pdf/pdf_TPD_205.pdf
trichrome staining method, 84.0% accurate;
monoclonal ELISA method 88.6% accurate;
monoclonal DFA method 79.5% accurate
Still over a 10% + miss rate
Fecal calprotectin (FC) stool leukocyte test been positive mean levels (above than 50 ng/ml) could be helpful but not a high yield:
- 38(41.75 %) for Entamoeba histolytica
- 10(21.27 %) for Giardia lamblia
- 1(3.22 %) for Blastocystis hominis;
- FC levels were at negative level for Dientamoeba fragilis and Chilomastix mesnili.
interestingly, “Co-existence of Helicobacter pylori (H.pylori) was seen with protozoan infections, 122 (71.34 %), with high dominant incidence38(41.45 %) was for Entamoeba histolytica.”
Could use anyone perspective here as I would just treat any chronic diarrhea with flagyl/metronidazole even with negative testing as might help bacterial overgrowth as well. – but could still not help 24-30% so should I routinely go into using tinidazole after?