A recent study found doctors had a poor knowledge of the features of Ankylosing Spondylitis (AS) which is why only 6% of women with this disease are properly diagnosed by GP’s. This will mean women with active spinal arthritis might have to wait 7 years to be diagnosed. Men with concomitant back injuries can suffer the same fate
Up to 11 Years to Diagnose
In:
Clin Rheumatol. 2008 Apr;27(4):457-62. Epub 2007 Sep 26. Diagnosis delay in patients with ankylosing spondylitis: possible reasons and proposals for new diagnostic criteria. Dincer U, Cakar E, Kiralp MZ, Dursun H. abstract here
They state “The average of diagnosis delay was 6.05 +/- 5.08 years.” I have seen cases missed for over ten years.
Doctor – Poor Awareness
Part of the reason is GP’s have poor training in what are features of the disease (you only see what you know):
Below is a study that found Doctors had poor recall of AS features:
Rheumatology (Oxford). 2008 Jun 24. [Epub ahead of print] Recognition of inflammatory back pain and ankylosing spondylitis in primary care. Jois RN, Macgregor AJ, Gaffney K.
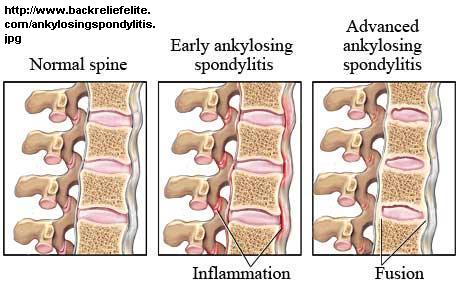
AS FACTS
AS is a spinal arthritis which often affects young people. It can cause persistent “insidious” back pain – comes with no reason and persists. The “give away” is the morning stiffness – it can take let say 30 + minutes to get the soreness improved by moving around. This concept is not well understood by some patients who say they are stiff all day; stiffness is a finding that works its way out by activity. Undiagnosed, not only do these people suffer unnecessarily, they are not offered medications that can prevent progression of the disease – Entanercept – Enbrel. – tumor necrosis factor(TNF) inhibitors.
WCB MISSED CASES
People who are really disadvantaged are those who have concomitant (at same time) back injuries. I have seen two young men with WCB discogenic back injuries who never got better. WCB was on their case for non-resolution. Recognition and treatment of the AS gives some relief but there is still some disc disease. However, this would give WCB the excuse to axe their cases. The only thing that works to their advantage here is that rheumatologists in this province seem to be unable to make that diagnosis without imaging evidence of sacroilitis. This can take 10 – 20 years to show so one can say there is no hard evidence (so there is doubt…).
The argument is made that these back-injured WCB cases developed AS before the average onset of the disease and hence the injury precipitated the early onset of AS.
In:
Clin Rheumatol. 2008 Apr;27(4):457-62. Epub 2007 Sep 26. Diagnosis delay in patients with ankylosing spondylitis: possible reasons and proposals for new diagnostic criteria. Dincer U, Cakar E, Kiralp MZ, Dursun H
ONSET AGE
In above article, “The average age of patients at disease onset was 23.18 +/- 9.59,“.
In the below article, the average ages were “27.7 years in B27– and 24.8 years in B27+ AS”
Rheumatol Int (2003) 23: 61–66
Ernst Feldtkeller et al.
Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis
I had a patient who wanted to claim the injuries prematurely brought on the AS – you would have to be significantly earlier than the average age to even make a case.
DELAYED RECOGNITION DEPENDS ON HLA-B27 status:
HLA B27 is one of many body markers that needs to be matched in organ transplants. When it is positive, it increases the chances of AS by 100X. However, depending on the population, maybe only 20% cases have these markers.
In Feldtkeller et al (2003), the delays in diagnosis were terrible: “The average age at disease onset was 27.7 years in B27– and 24.8 years in B27+ AS (P<0.01). The average age at diagnosis was 39.1 and 33.2 years and the average diagnosis delay 11.4 and 8.5 years, respectively.”
WOMAN WORSE OFF
Woman are worse off because the joints first affected are the sacroiliac joints. These joints are often too mobile in women – part hormonal, and definitely related to childbirth. So they endure low back pain for years thinking it is just the SI joints. By the time they were so bad off that they were referred to a rheumatologist, about 50% of men had been diagnosed, but only 6% of woman had been. Why were they sent to a rheumatologist? – because they have “Fibromyalgia”. One McGill study found many people referred for Fibromyalgia actually had subclinical rheumatic disease:
Rheumatology (Oxford). 2003 Feb;42(2):263-7. Inaccuracy in the diagnosis of fibromyalgia syndrome: analysis of referrals. Fitzcharles MA, Boulos P. abstract here
“At the final evaluation the accuracy of the diagnosis regarding FM by either the referring physician or by the rheumatologist at the time of the initial visit was correct in 34% of patients.”
The majority were early stages of rheumatic diseases (including AS). Not surprizingly, they found “prolonged early morning stiffness and limitation of lumbar spinal mobility in more than one plane was more common in the non-FM group”
AS FEATURES
Features that reflect AS include:
- Family history of arthritis – these people with a family history of rheumatoid or ankylosing spondylitis don’t have to wait as long because there is heightened suspicion.
- Early onset (20’s and older)
- Insidious back pain – In patients with persistent back pain for no reason, 17% (1/6) will be AS
- Morning stiffness > 30 minutes. I would not depend on the 30 minute time limit. I have had cases in which there was a dramatic response to arthritis pills yet only 15 minutes of morning stiffness. I think any morning stiffness might be suspicious.
In a related disease, Rheumatoid Arthritis, 15% of cases had morning stiffness less than 15 minutes:
J Rheumatol. 2004 Sep;31(9):1723-6. Morning stiffness in patients with early rheumatoid arthritis is associated more strongly with functional disability than with joint swelling and erythrocyte sedimentation rate. Yazici Y, Kautiainen H, Sokka T.
abstract here
- Pain relieved by NSAID’s – Rapid response to arthritis pills and relapse off this medication. I think this is probably my favorite – what good is the diagnosis if you can’t treat it? However, I have seen cases in which a Kenolog 60 mg IM shot or Enbrel 25 mg sc./IM shot was necessary to see the good response.
- Symptom duration > 3 months
- Nocturnal pain – (second half of the night only) one of the main deformities that can occur in AK is flexion in the lumbar spine. Tummy sleeping becomes impossible that way. Inflammation does not take a rest so it turns up at night as well. However, if one has significantly bad back pain and there is no position to get rid of the pain, then cancer needs to be ruled out – this person needs a bone scan.
- Pain improved with exercise
- Pain not relieved by rest
the prior two demonstrate the opposite of what you would expect with mechanical back pain – mechanical (disc and facet) back pain generally gets better with rest and worse with activity. AS subjects stiffen up with rest and limber up with activity. I know people I am diagnosing with AS will be resistant to that diagnosis so I often ask undiagnsed patients to explain why they are worse with rest and better with activity. - Alternating buttock pains – SI joint pain is generally NOT a back pain – it is belt line or lower. The finding of buttock pains, particularly switching sides, is suspicious.
- Psoriasis – finding of back pain in someone with psoriasis automatically makes one think of psoriatic arthritis
- Inflammatory bowel disease – strong connection with spondylitis (active back arthritis). Conversely people with AS will often have subclinical bowel inflammation. This bowel inflammation would get worse if the NSAID’s (arthritis pills) causes bowel ulcers ( yes, NSAID’s do more than just cause stomach ulcers – they can occur in the bowel as well). There are some bowel diseases – microscopic colitis and cleliac disease – that can be associated with spondylitis. I am very suspicious of AS in people with bad “irritable bowels” (though Irritable bowel causes psoas spasm which triggers increased back issues). I have another blog writeup on how these bowel conditions cannot be diagnosed properly in Saskatchewan.
- Uveitis – of people with acute red eye uveitis, if they are HLA-B27 positive, 55% have AS; only 4% if not; abstract here
- Genitourinary/gut infection in the last month – non-gonococcal/non-specific urethritis (often hurt to pee but many have subclinical disease) caused by chlamydia/mycoplasma is implicated as a trigger for AK. Inflammatory bowel disease does likewise
- Enthesitis – this is tenderness at tendon, ligament, or joint capsule which is a better indicator of AS severity whole text here
(I made the illustarion big because I thought people would be interested – the spine and rib and other joints can complain without clinical arthritis leading some to do point counts for “Fibromyalgia”)
(pics: Mander, M., 1986)
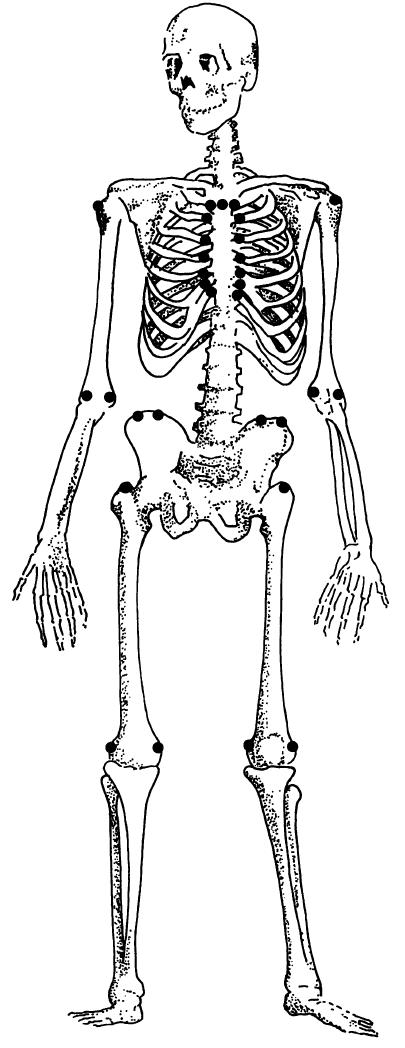
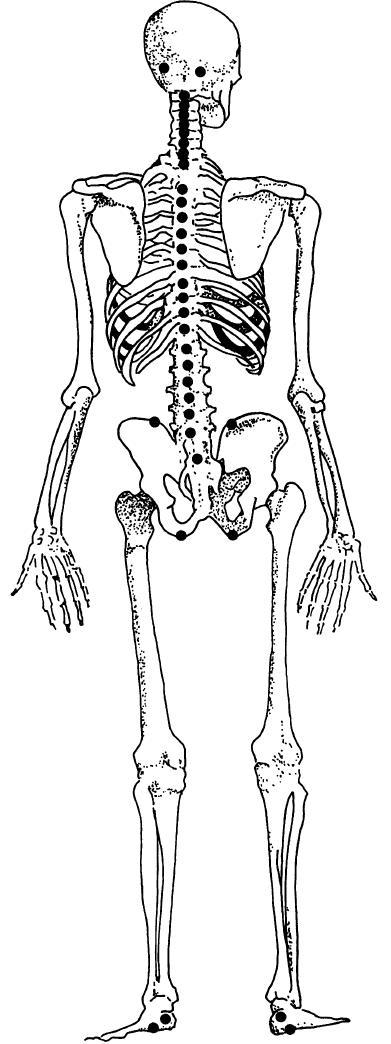
Most frequently scored enthesis points at baseline, at one year follow up, and at two year follow up in order of detection during the data reduction process. Heuft-Dorenbosch, L.,2003
Baseline
Proximal insertion of Achilles tendon left
Iliac crest left
5th Lumbar spinous process
7th Costochondral joint left
1st Thoracic spinous process
One year follow up
7th Costochondral joint right
1st Costochondral joint right
Proximal insertion of Achilles tendon left
4th Lumbar spinous process
9th Thoracic spinous process
Two year follow up
5th Lumbar spinous process
7th Costochondral joint right
Posterior superior iliac spine left
4th Costochondral joint left
Anterior superior iliac spine right†
- Dactylitis – swollen fingers
- Inflammatory markers – ESR useless but CRP may help if not ignored – these tests correlate poorly with severity of disease however.
IN:
J Rheumatol. 1999 Apr;26(4):980-4. Relative value of erythrocyte sedimentation rate and C-reactive protein in assessment of disease activity in ankylosing spondylitis; Spoorenberg A, van der Heijde D, de Klerk E, Dougados M, de Vlam K, Mielants H, van der Tempel H, van der Linden S.
“The median CRP and ESR were 16 mg/l and 13 mm/h, respectively, in the spinal group and 25 mg/l and 21 mm/h, respectively, in the peripheral/IBD[inflammatory bowel disease] group.”
These tests could be worse than useless – a negative test, if considered adequate to Rule out AS, would eliminate even the average AS. ESR N= 0-20 so they would be normal in AS; CRP level normally range from 0-5 so actually seems much more sensitive.
- HLA-B27 testing -Given that most AS are negative, it is only of use where positive. A positive test does not ensure accuracy of diagnosis but makes it 100X more likely. This in an expensive test that has to be co-ordinated ahead of time with a Saskatoon lab. Blood is drawn from a local lab on a Monday and sent up. They don’t want GP’s doing the test because some will do it on every patient with back pain. I managed to get one done by saying that the Rheumatologists can be just as stupid. The patient in question had significant morning stiffness, good response to NSAID’s and was on disability – most certainly did not just have Fibromylgia. She turned out to be HLA-B27 positive.
- Spinal Xrays and Bone scan useless in early
Finding out how useful these xrays are begs a question. How sensitive are X-rays? If you take a group of already diagnosed people then you preselect those advanced enough to likely have radiological findings. A more realistic approach would be to go back 5-10 yrs when they were having symptoms and see if they were diagnosable then. One study, however,came out with the following specificities and sensitivities.
The evaluation of sacroiliitis using 99mTc-nanocolloid and 99mTc-MDP scintigraphy
YILDIZ, A.1,*; GUNGOR, F.1; TUNCER, T.2; KARAYALCIN, B.1
Nuclear Medicine Communications
Issue: Volume 22(7), July 2001, pp 785-794
- XRAYS – Only 25% sensitive but 80% specific – this means what I have always known – Xrays in early AS are useless
- 99mTc-nanocolloid scintigraphy – 47% sensitivity and 90% specificity – means a negative result is no better than the flip of a coin. The authors concluded “99mTc-NS was neither specific nor sensitive enough in the detection of sacroiliitis”.I had a case of rather severe AS that had a concomitant back injury that delayed his diagnosis.He had the classic morning stiffness and fatigue. Response to NSAID’s was dramatic. I sent him to Saskatoon to our teaching hospital because there is poor early pickup of these cases here. The Rheumatologist asked if I would do the bone scan in Regina but I thought they would do more at that tertiary center – maybe speck or planar bone imaging with the scan. Unfortunately just a plain old bone scan was done. It was, of course, negative. The Rheumatologist anounced that the patient did not have AS. Problem is, patient had zero ability to extend his back and his psoas muscles were NOT in spasm. So he had significant “ankylosing” already. He went to physio who wanted to know how old this Rheumatologist was… I felt the same way. Steroid injections into his SI joint gave him good relief.
Rheumatologists can be as bad as GP’s
I will repeat this for emphasis:
Rheumatology (Oxford). 2003 Feb;42(2):263-7. Inaccuracy in the diagnosis of fibromyalgia syndrome: analysis of referrals. Fitzcharles MA, Boulos P. abstract here”
At the final evaluation the accuracy of the diagnosis regarding FM by either the referring physician or by the rheumatologist at the time of the initial visit was correct in 34% of patients.”
The issue relates to the quote above initial visit – i.e. first impressions. Many of the chronic pain patients I see have a complex set of problems; much can get missed until you work out a few and “unlayer things” . Then you get to see what is left. The clinical course and response to various medications gradually makes things more evident.
Another important issue is the fact that Rheumatologists are very reluctant to make early diagnosis. I think they must have been wacked over the head by their supervisors in training until they were willing to accept that this is what they must do. I have had to fill out AS criteria forms explicitly in past if there is doubt to emphasize their features.
To make things worse, there is a subgroup that will get back arthritis but no sacroiliac involvement:
Arthritis Rheum. 2008 Jun 24;58(7):1981-1991. [Epub ahead of print]
Efficacy of adalimumab in the treatment of axial spondylarthritis without radiographically defined sacroiliitis: Results of a twelve-week randomized, double-blind, placebo-controlled trial followed by an open-label extension up to week fifty-two. Haibel H, Rudwaleit M, Listing J, Heldmann F, Wong RL, Kupper H, Braun J, Sieper J.
https://onlinelibrary.wiley.com/doi/abs/10.1002/art.23606
MRI – There are frequent studies reporting MRI superior but I think the experience of the radiologist is going to be the prime factor. MRI cannot be ordered by GP’s in our province.
Bottom Line
If one is a woman with persistent low/belt line and below back pain (obviously pain tends to spread so other areas will be involved & AS affects neck and rib joints as well) – I would look very closely at the morning stiffness, whether you are better with rest or activity, and whether arthitis pills give you substantial help. It appears you should not trust your doctor’s initial opinions too much and maybe not even the Rheumatologist if s/he only sees you once and renders an opinion.
I find I can not give this topic justice but there are Ankylosing Spondylitis organization sites.
addendum:
Women are less likely to show HLA-B27 changes as well:
Xiong J, Chen J, Tu J, Ye W, Zhang Z, Liu Q, et al.
Association of HLA-B27 status and gender with sacroiliitis in patients with ankylosing spondylitis. Pak J Med Sci 2014;30(1)
http://www.pjms.com.pk/index.php/pjms/article/view/3896/1929
I would be interested in others views on the subject.

Back in 2003 I seen a GP about persistent back pain, apparently he had AS. Though he did not tell me the name of the condition he seemed positive I was on the same road. He recommended physio-therapy and had an X-ray done. End of consult.
Five years later I again felt compelled to consult with a doctor regarding my back pain, again an X-ray was done, but this time the doctor not only showed me the X-ray, but took the time to read the report that accompanied it. But again, physio-therapy was the only recommended treatment. This time the doctor did identify the condition as AS. The report said I had mild spondylitis.
At what point should I be consulting with a rheumatologist? The diagnosis has been made yet no referral has ever been made.
My family has: Ankylosing Spondylitis, Raynaurd’s, Erythromelalgia, and Spondylothropies. Diagnosis took 30+ years for AS, 5-6 yrs for the Erythromelalia. Thank you from the bottom of my heart for this article.
Your article is so informative and has been so helpful to me; it has given me hope again!
I have a family history of AS (one of my parents, one of my siblings, one of my children, and they are just the ones I’m certain of; there are several more). I am HLA-B27 positive, I have had 3 or 4 flares but the most recent was the most severe by far: within a few weeks I lost a lot of the mobility in my left arm. I have pain in both sacroilliac joints, my shoulder, arm, shoulder blade, colar bone, wrist, spine at the back of my neck, and jaw (all on my left side plus right sacroilliac) and I am in constant pain especially at night. I am feaful that more damage is occuring and I will lose mobility elsewhere. I have been going to my GP for this occurence since January when I had the flare, and he still tells me that he thinks it is a rotator cuff issue. Thankfully he has finally and reluctantly referred me to a Rhematologist, but I am not at all confident that the rheumatologist will diagnose me correctly; i saw the same one a few years ago. One of my parents also has Raynaurd’s, and of my children has Erythromelalgia which has a huge impact on her life. I am trying so desperately to help her and now I am not well. It is a a scary, lonely road and I feel like no one will really listen. It was 6 years of trying and searching to get my daughter dianosed, 30_+ years for my sister and she was only diagnosed because I sent her to an AS site and she went to her Dr and insisted on testing (her GP said to her “you don’t have AS. AS is a terrible disease. You would be much sicker if you had it, and stop listening to your sister” and then the x rays showed her spine and ribs fusing. Again, thank you sincerely and please continue to both research, and publish on the web, your wonderful work. If you every have more recent info that you have time to send, please, please feel free to do so. fax 1-877-776-6847 phone 250-727-2047, email lynda_smith@live.ca kindest regards, Lynda Smith
Hello! I have been looking all night to find info regarding bone scans and AS.
I have Sjogren’s and mixed connective tissue, I did not present with typical dry eye, etc., though I do have that now. I just got sick, lost weight, I’ve had a fever every day for two years, it goes on and on. But one thing I have had through out is this horrible lower back pain, particularly in the lower right hip area. Now, I can hardly sit down and I have to sit on one of those blow up donut things when I drive. The pain in my hips, bum, through my legs, some times right down to my ankle. It is like my bone is cramping, the pain is so deep. Sorry so long.
My question is……….I just had a bone scan that came back neg. Does that mean that I don’t have arthitis at all? I had an x ray that showed thoracic spondylosis.
I’ve just been given celebrex and it is actually helping. I have gastric ulcers, so have been unable to take ibprofen nsaids. Still, right here as I type it hurts. It hurst so much that without knowing it I’ve been flexing or tightening my legs to the point they are raised off the bed.
Anyway, sorry for the book I just wrote. Thanks
Rose
Difficult aspect about doctor patient partnership in managing chronic pain, is that some docs are unable to trust the possibility that inflammatory arthritis or AS can be diagnosed using accepted criteria such as stiffness relieved by activity and the rest. Fibromyalgia as a diagnosis has not helped women at all. GPs who are poorly informed will frequently resort to prescribing low dose anti depressant as treatment. This has been proven to be no better than placebo. Mindfulness meditation and mindful self compassion practice are of more benefit and should be encouraged and prescribed for women who wish to manage their pain with a level of acceptance. Being able to separate the thinking about pain from the experience of pain is a wonderful tool for managing this difficult problem. Other benefits can result such as improved sleep, less reactivity, increased tolerance in dealing with difficult emotions and the rest.