Post-Craniotomy Headaches are annoyingly common – “Headaches following craniotomies are reported in up to 91% of neurosurgical cases”. Injecting craniotomy edge defect triggers, scar neuromas, and botulinum to temporalis muscle are local treatment options.
Surgical scar injection (both articles by same group)
Ferreira, Karen dos Santos, Fabíola Dach, and José Geraldo Speciali.
Scar neuromas as triggers for headache after craniotomy: clinical evidence.
Arquivos de neuro-psiquiatria 70.3 (2012): 206-209.
http://www.scielo.br/scielo.php?pid=S0004-282X2012000300010&script=sci_arttext
Dach, Fabíola, et al.
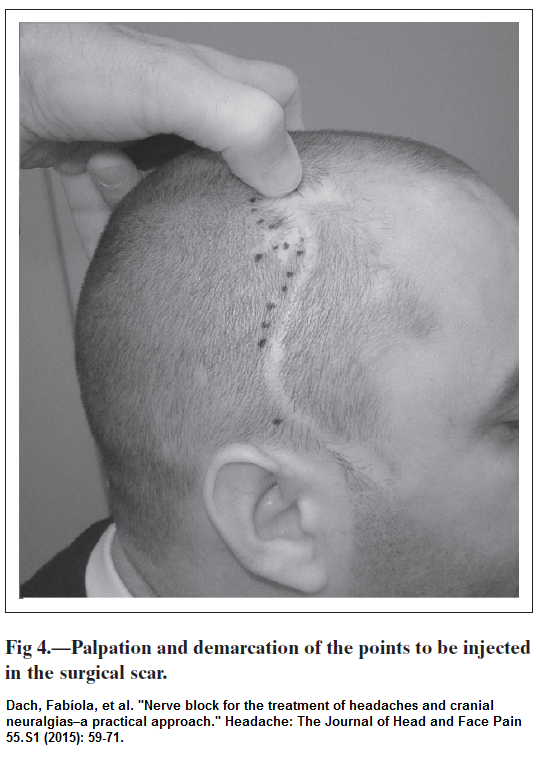
Nerve block for the treatment of headaches and cranial neuralgias–a practical approach.” Headache: the Journal of Head and Face Pain 55.S1 (2015): 59-71.
https://onlinelibrary.wiley.com/doi/full/10.1111/head.12516
 Edges of craniotomy treatment:
Edges of craniotomy treatment:
- There may be plenty of triggers as seen in above pic.
- “With respect to neurosurgical scar blockage, in order to avoid intracranial diffusion of the anesthetic agent through a bone defect, we recommend some cautions. First of all, the region to be injected must be carefully palpated, looking for bone defects. Second, demarcate the points to be injected with a nontoxic ink pen. Third, the needle should be inserted 5 mm at an angle of approximately 30 degrees with the skin surface.”
- I also suggest fluid should bleb up skin some as injected.
- “At every new consultation, the scar is again palpated looking for trigger points of pain, and if they exist, they are infiltrated again.”
- “in cases of headache attributed to craniotomy, in which multiple infiltrations
may be needed” - They appear to use 2% lidocaine but I would be more likely to use 1%
- For cases not responding to local injections, suggest three – weekly nerve block injections
- Having said, they move on to blocks if necessary, they don’t exactly say how well treatment goes, but implication was that it goes well but is a lot of work with multiple sites done and blocks to nerves as well.
- Injecting through a hairy site isn’t exactly sterile so I give cephalexin 500 3 tabs prior and tab 1 qid x 1 -2 day
scar neuroma treatment:
- digital pressure reproduces pains
- case 1 -frontoparietal severe (9/10), throbbing for up to 12 hours, with nausea and photophobia. “inject the most painful points of the scar with a solution of lidocaine 2% (1.5 mL) and dexamethasone 10 mg/2 mL (0.5 mL). We repeated the procedure three more times during the next four months”
- case 2 – severe temple episodes pain lasting minutes – injected points with a solution of lidocaine 2% (1.5 mL) with dexamethasone 10 mg/2 mL (0.5 mL).
- case 3 – right frontotemporal throbbing +/- burning; severe (10/10) ass’d ipsilateral conjuntival injection and lacrimation . Worse with physical activity – 3 to 4 times per week – “most painful points of the surgical scar with a solution of lidocaine 2% (1.5 mL) plus dexamethasone 10 mg/2 mL (0.5 mL).” one rx better
- case 4 – right temporal throbbing, severe (8/10)), with photophobia and tearing ipsilateral to the pain side lasting 72 hours weekly. Injected the most painful points of the surgical scar with a solution of lidocaine2% (1.5 mL) and dexamethasone 10 mg/2 mL (0.5 mL) – cut problem to 1/3
Botulinum treatment:
Ranoux, Danièle, et al.
Delayed-onset post-craniotomy headache responsive to botulinum toxin A: a case series.” Acta neurochirurgica 159.8 (2017): 1375-1378.
https://link.springer.com/article/10.1007/s00701-017-3215-z
The botulinum cases were chosen because of temporalis enlargement post surgical
- 4 cases of temporofacial pain after temporal craniotomy
- temple pain
- last 10 – 60 min
- often referral around the eye
- 1-3 times daily
- mostly sharp, compressing pain
- not affected by jaw action
- hypertrophy temporalis though maybe only seen when chewing – and maybe only part of muscle
- dilute botulinum 100 u in 1 ml and inject 25 – 50 units – most often a single point
- attacks either ceased or reduced 90%
Lastly, if skin has in-folded over craniotomy edge, then surgical revision can help:
Milan, Spaić, and Aleksić Vuk.
Cranioplasty for the Relief of Chronic Pain: 70 Years after the Debridement of the War-Penetrating Craniocerebral Injury.
Indian Journal of Neurotrauma 14.01 (2017): 043-045.
https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0037-1603815
Comment –
- repeated injection of post craniotomy patients either locally or nerve root blocks can make a major difference. Injecting neuralgic areas with botulinum by self may not reduce the problem but the areas are then more easily deadened by local/steroid blocks after. I found this out working with a case of occipital neuralgia. I would inject tender nerve and areas with botulinum and then in ensuing weeks inject with 5% local with control of symptoms for up to 12 weeks. This has worked for 17 years despite him working hard “grunt” labor jobs. I would not inject 5% in a post craniotomy area though.
- number of areas needing injecting, according to picture is daunting but apparently well worth it.
- looking for neuroma sites should be utmost importance

