I recently wrote about how they are only now finding certain abdominal wall injections work for chronic abdominal pain in adults – confirming source is the abdominal wall – what already???
I suspect it is even worse with children in which 30% of chronic abdominal pain is thought originated from the abdominal wall and amenable to injection. Study in press documents features and treatment.
Eur J Pediatr. 2018 Mar 7.
doi: 10.1007/s00431-018-3125-y. [Epub ahead of print]
Diagnostic characteristics of anterior cutaneous nerve entrapment syndrome in
childhood.
Siawash M et al
https://www.ncbi.nlm.nih.gov/pubmed/29516161
- puts incidence at 1:2000
- more in females(77%) and 2/3 on right side.
- quote 4 references stating abdominal wall is the source of pain ip to 30% of chronic abdominal pains in children:
9. Gray DW, Dixon JM, Seabrook G, Collin J (1988) Is abdominal
wall tenderness a useful sign in the diagnosis of non-specific ab-
dominal pain? Ann R Coll Surg Engl 70:233 – 234
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2498809/pdf/annrcse01551-0051.pdf
found 45% acute abdominal pains ended up having chronic non-specific abdominal pain of which 28& of those had abdominal wall tenderness = 45 x 28 = 12.5% incidence
12. Lindsetmo RO, Stulberg J (2009) Chronic abdominal wall pain —
a diagnostic challenge for the surgeon. Am J Surg 198:129 – 134
https://www.scholars.northwestern.edu/en/publications/chronic-abdominal-wall-pain-a-diagnostic-challenge-for-the-surgeo
states 30%
13. McGarrity TJ, Peters DJ, Thompson C, McGarrity SJ (2000)
Outcome of patients with chronic abdominal pain referred to chron-
ic pain clinic. Am J Gastroenterol 95:1812–1816
https://www.nature.com/articles/ajg2000459
19. Srinivasan R, Greenbaum DS (2002) Chronic abdominal wall pain:
a frequently overlooked problem. Am J Gastroenterol 97:824– 830
https://www.sciencedirect.com/science/article/pii/S0002927002040182
states 10% in general population;
So not really that much to quantify in children
Most of the chronic abdominal pains are thought related to anterior cutaneous nerve entrapment syndrome (ACNES). In adults features were:
- stabbing/burning pain sensation;
- superficial or deep abdominal pain;
- pain spot fixed or varying through time
- pain aggravation due to exercise.
their exam included supine exam:
- light touch: – swab test food side first, then other thorax – groin. feedback marks it as numbish or painful
- cold test – one speaker suggested a cold tuning fork was a good option
study found 9/10 had ” somatosensory disturbances such as hypo- or hyperesthesia and altered cold perception of an approximately 3 × 5 cm area of skin overlying a fixed point ”
- Pinch test – light pin good and bad sides and se if produces excessive tenderness.
- Carnett’s test – have subject lift head and heels and press abdomen for tender spots
- My test – found by accident – have lie with bad side up. Engage tissues laterally with fingers and push tissues medially. Will come to a very tight muscle edge especially at worst level and this will be tender. Avoids need to press down to where abdominal structures lay. Also can inject tight muscle edge laterally without having to aim down too much. Can feel tight painful structures without them tensing with arms and legs up – more sensitive that way.
injection technique based on:
Siawash, M., Mol, F., Tjon-A-Ten, W., Perquin, C., van Eerten, P., van Heurn, E., Roumen, R. and Scheltinga, M. ,
Anterior rectus sheath blocks in children with abdominal wall pain due to anterior cutaneous nerve entrapment syndrome: a prospective case series of 85 children.
Paediatr Anaesth,2017. 27: 545–550.
doi:10.1111/pan.13084
http://onlinelibrary.wiley.com/doi/10.1111/pan.13084/full
- skin covering the most painful spot was
stretched between two digits of one hand. - 10 ml syringe with a 21 gauge needle
- inject with other hand – (my take): – usual spot is a fascial depth so could sweep needle back and forth a bit until hit level where it is grabbed by fascia -“Needle length matched the thickness of subcutaneous fat.”
- Pull back on plunger to ensure not in a blood vessel
- Inject 4 ml lidocaine 1% and a steroid (1 ml methylprednisolone 40 mg)
Alternate approach of mine: –
- bad side up on side
- engage tissues laterally and push medially with index and middle finger bit separated.
- tissues will heap up away from abdomen as you engage tight tender tissues more medially
- Once tender spot located, can inject more lateral to medial against heaped up mass between two separated fingers
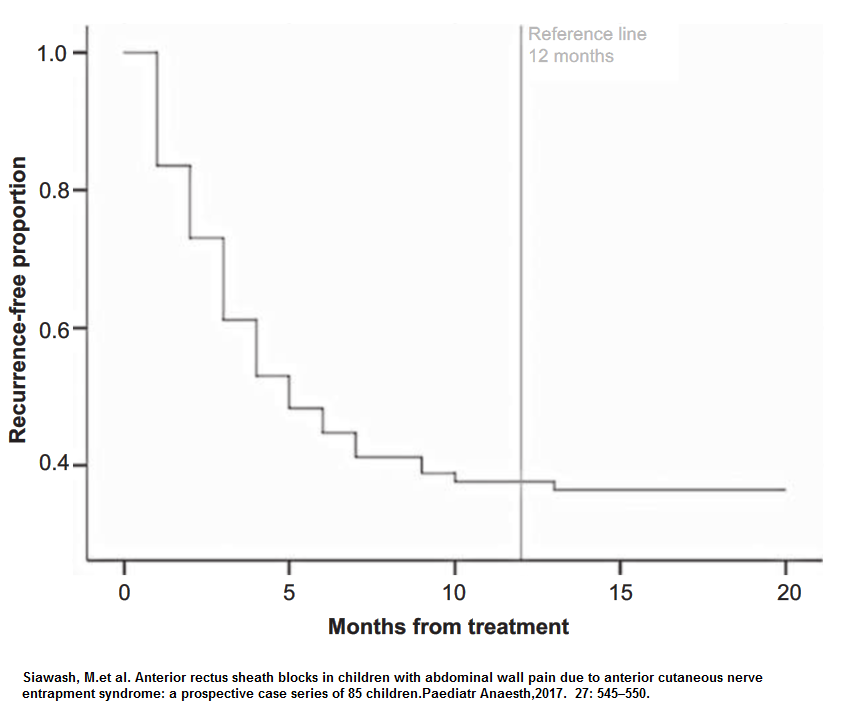
Results –
- Children had up to 3 injections
- they claimed at 38% long success rates – ie helps in more than one-third
- older children responded less well
first article (Siawash M et al) claimed “ substantial pain relief to more than 75% of patients, often for prolonged periods, and may be confirmatory for the source of the complaint”
Comment – a proportion on children are suffering needlessly and could be help by injection.