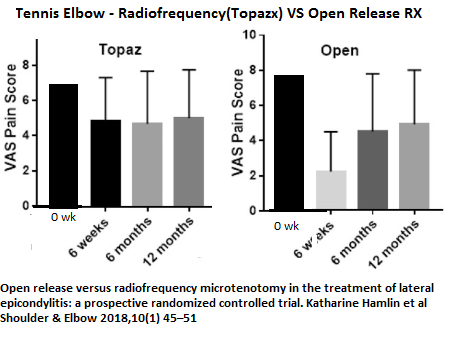
Randomized trial of open release (OR) or radiofrequency microtenotomy (RFMT) for tennis elbow. Article suggests: “As a result of the extra expense of RFMT, we therefore recommend that OR is offered as the standard surgical management.”
Open release versus radiofrequency microtenotomy in the treatment of lateral epicondylitis: a prospective randomized controlled trial
Katharine Hamlin et al
Shoulder & Elbow 2018, Vol. 10(1) 45–51
http://journals.sagepub.com/doi/abs/10.1177/1758573217715255
- 23 RFMT; 18 open; more women in RFTM group
- Subjects had at least one cortisone shot and failed
- Same incision for either procedure
- Open release procedure: “A distally based horseshoe shaped flap was raised in the common extensor origin, the underlying bone surface was smoothed and any obvious inflammatory or degenerate tendon debrided. The flap was not repaired. The capsule was not breached, nor was the joint entered.”
- Radiofrequency Microtenotomy: – “The common extensor origin was identified and, using a TOPAZ Microdebrider coblation Wand (Arthrocare, Austin,
TX, USA), multiple passes were made with the tip through the tendon at approximately 5-mm intervals to varying depths and for varying lengths of time.”
Results:
- pain drops from Seven-ish/10 to four-ish which is not great but for I presume resistant cases is something
- The results of open surgery are initially much better but then it gradually rises up to 4-ish again over next 4 months
Reasons for failure to get all better?
- Subject is involved in work at overstrains forearm. I remember an older carpenter whose work style contributed to his issues.
- They are no longer dealing with tennis elbow – they are dealing with what is now a regional pain syndrome. I saw an elderly lady last week who injured her supraspinatus tendon lifting a casserole (pain on resisted abduction). To my horror she was already getting super-imposed pain in shoulder tip and right side of neck. The fact that pain regionalizes to affect many muscles and the facet at level of pain involvement seems to be continued to be ignored. Massage therapist don’t ignore it but physicians pretend it doesn’t exist. Dr. Chen Gunn, founder of intramuscular stimulation, was the first to deal with it and took WCB patients and made them better by needling regional muscles and having a physiotherapist US facet joints.
Can Med Assoc J. 1976 May 8;114(9):803-9.
Tennis elbow and the cervical spine.
Gunn CC, Milbrandt WE.
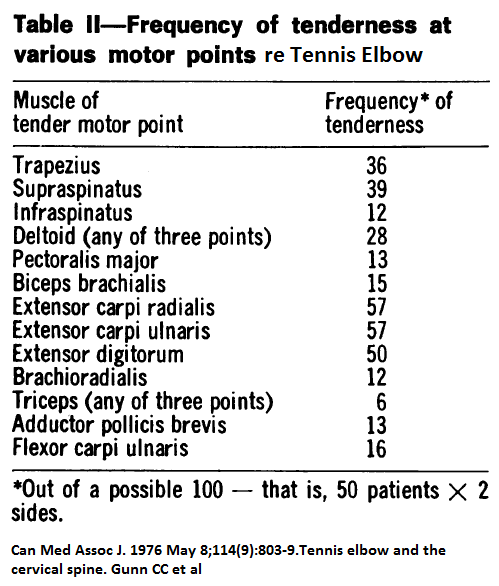
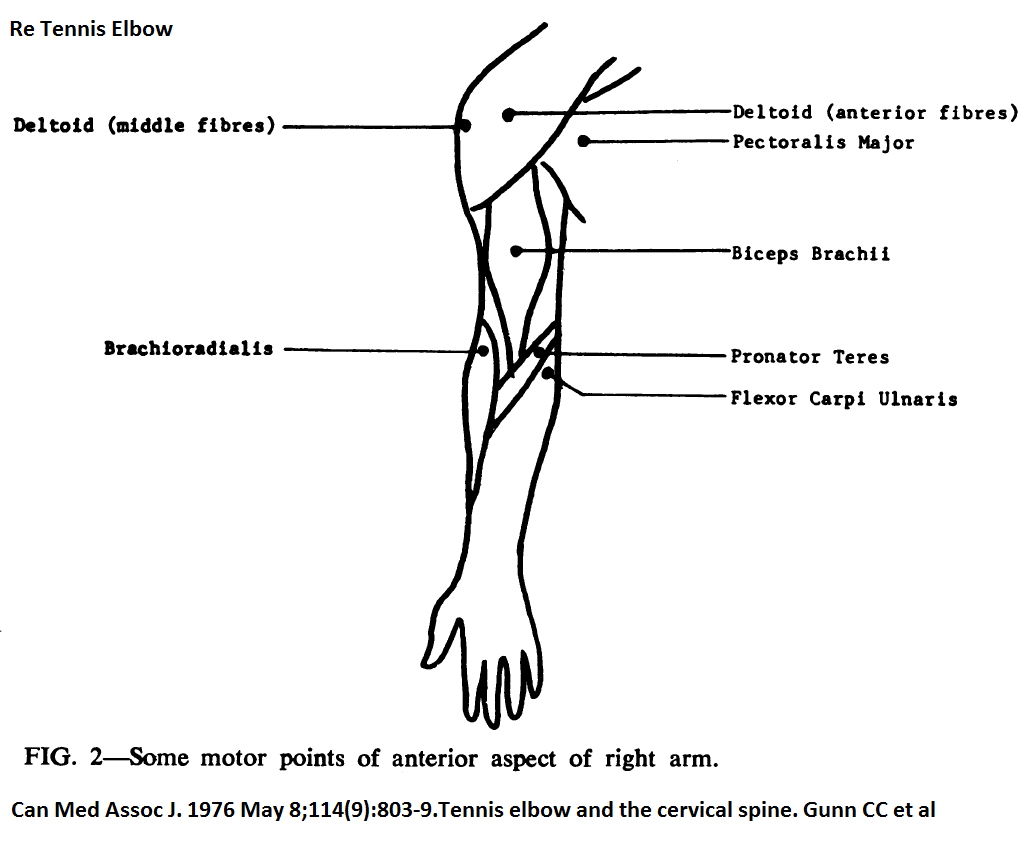
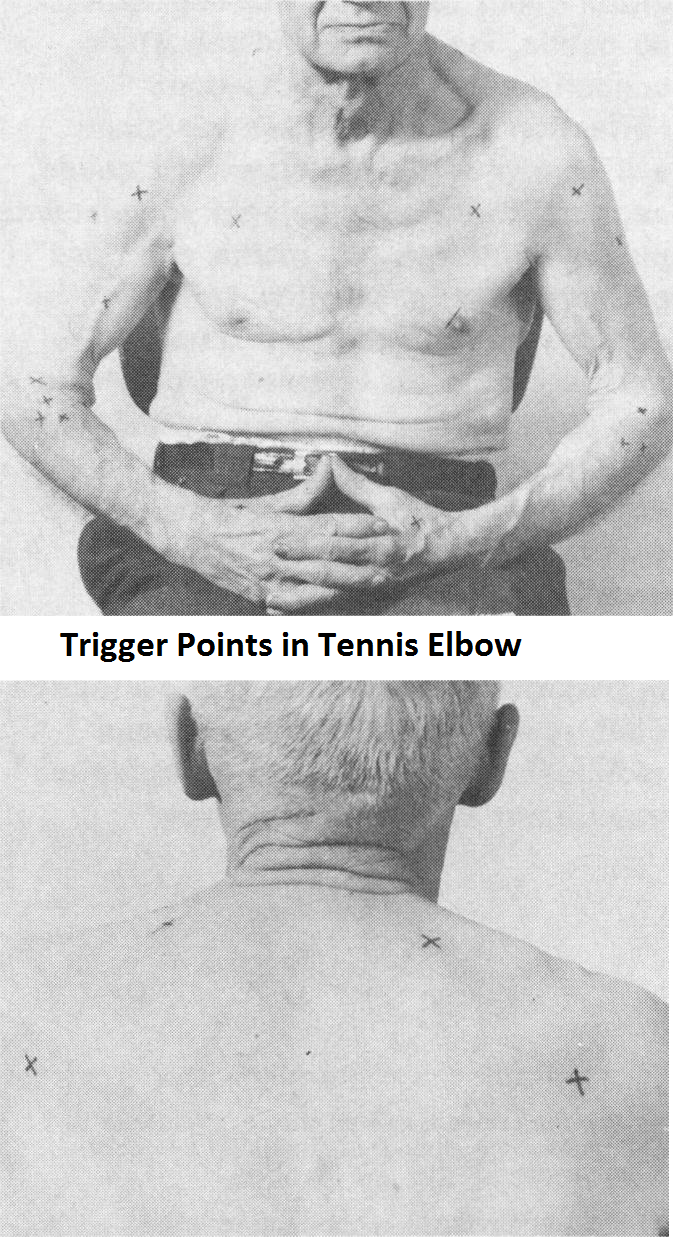 Note the date on that…To be fair, some of the tennis elbow cases were probably regional pain syndromes to start with – from then neck – both disc bulges, facets, and early radiculitis could be involved. However, I will content that some of them started with the elbow and spread out to encompass many of the tissues and the neck. Getting the pain down from 4/10 will in part involve dealing with regional triggers and the cervical spine.
Note the date on that…To be fair, some of the tennis elbow cases were probably regional pain syndromes to start with – from then neck – both disc bulges, facets, and early radiculitis could be involved. However, I will content that some of them started with the elbow and spread out to encompass many of the tissues and the neck. Getting the pain down from 4/10 will in part involve dealing with regional triggers and the cervical spine.
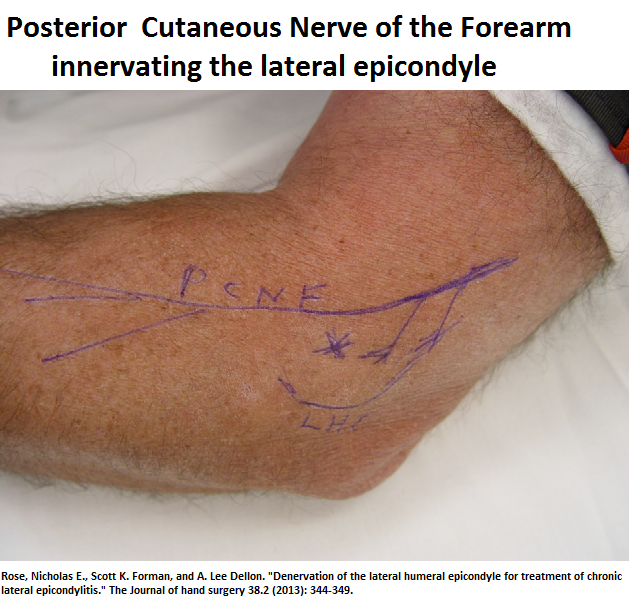
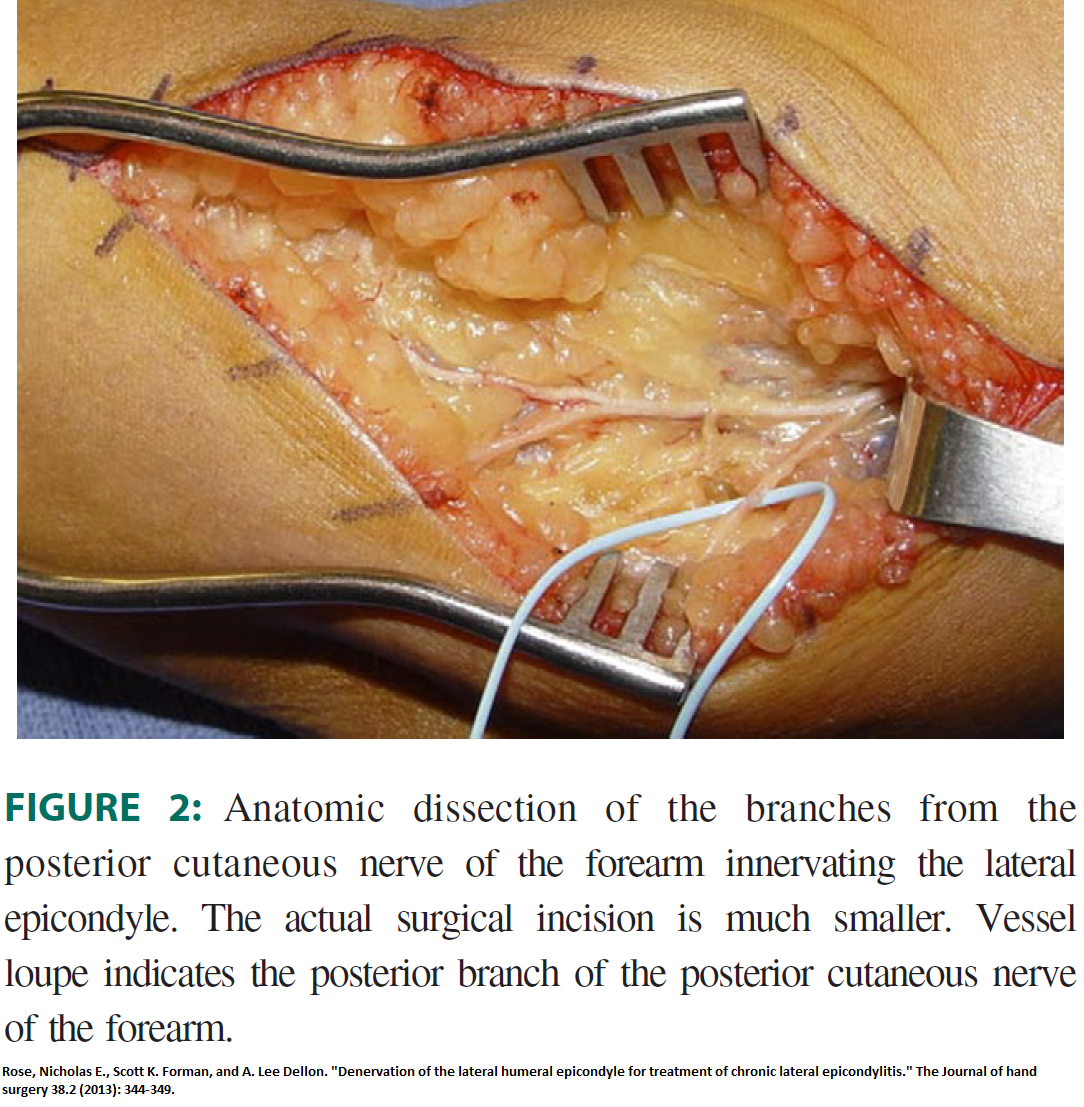
It is also becoming clear that sensitized nerve in area can impact tennis elbow and denervation of “the posterior branch or branches of the posterior cutaneous nerve of the forearm” can relieve 80% of those relieved by prior block.
Rose, Nicholas E., Scott K. Forman, and A. Lee Dellon.
Denervation of the lateral humeral epicondyle for treatment of chronic lateral epicondylitis.
The Journal of hand surgery 38.2 (2013): 344-349.
http://www.sciencedirect.com/science/article/pii/S0363502312015535
- used a “positive response to a 5-mL 1% lidocaine/ 0.5% bupivacaine block of the PBPCNF at a point 4 cm proximal to the lateral humeral epicondyle.” – ” using a 25-gauge, 4-cm needle. We placed 5 mL 1% lidocaine/0.5% bupivacaine mixture into the subcutaneous tissues without injecting near the radial nerve.” – “nerves tend to be superficial. The size and number of branches of the PBPCNF can vary”
- “A positive response was defined as a decrease in 5 or more points on the visual analog scale (VAS),defined as the patient’s average daily pain, and an increase in grip strength”
- Nerve was microdissected , transected, and “buried within the
lateral head of the triceps musculature posteriorly.”
- VAS pain 7.9/10 before and 1.9/10 after surgery.
- 80% good to excellent results and followup was at least 6 months.
There were 5 failures – 4 were identified as radial tunnel compression and 3/4 responded well to radial tunnel decompression.
Radial tunnel compression occurs when the deep interosseus radial branch goes under the supinator muscle.
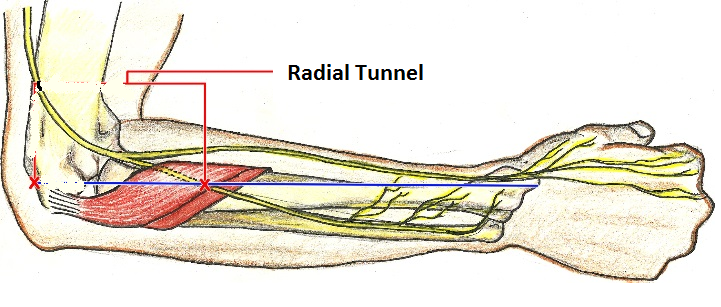 You feel it just down from where you palpate the radial head anteriorly. Injecting the tenderest point can give some relief and pain is reduced from 6.7 to 3.7 one year later with the worst offenders having decompression surgery
You feel it just down from where you palpate the radial head anteriorly. Injecting the tenderest point can give some relief and pain is reduced from 6.7 to 3.7 one year later with the worst offenders having decompression surgery
Marchese, Joseph, et al.
Prospective Evaluation of Single Corticosteroid Injection in Radial Tunnel Syndrome: Level 4 Evidence.
Journal of Hand Surgery 42.9 (2017): S51.
http://www.jhandsurg.org/article/S0363-5023(17)31095-X/pdf
I will inject it at same time as tennis elbow if tender using only 20 mg kenalog if using 40 mg on lateral epicondyle.
It has to be mentioned that some cases the radio-humeral joint is tender and injected as well with 10-20 mg steroid. This tenderness could represent instability which triggers the tennis elbow and is better dealt with with with prolotheapy:
Chronic Tennis Elbow Might Be an Instability Issue
http://painmuse.org/?p=5432
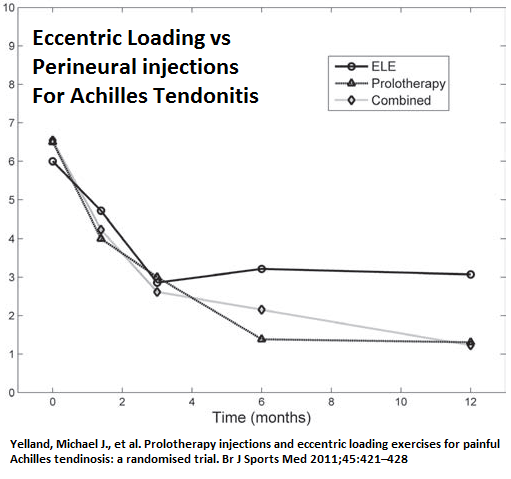
Comment – I inject the lateral epicondyle with 40 mg triamciolone in 5-10% lidocaine with particulate methylene blue – that has neurolytic properties and I have rarely seen recurrence though I have not enough for a study. I suspect this nerve could be felt and semi-neurolytic injection without steroid could be used. This is similar to what I am finding with trochanteric bursitis – some of the cluneal nerve course across the area and any buristis flares them up. I deal with them after steroid relief of inflammation by injecting perinerally, D5W along skin tracts – repeatedly. I wonder if D5W repeated injections could be of any use for tennis elbow as they were found useful in achilles tendonitis though took some time. (called it prolotherapy in skin at time but later realized 5% dexrose worked as well)
Yelland, Michael J., et al.
Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial.
Br J Sports Med 2011;45:421–428.
doi:422 10.1136/bjsm.2009.057968
https://research-repository.griffith.edu.au/bitstream/handle/10072/35744/66460_1.pdf?sequence=1
“A doctor injected tender points in the subcutaneous tissues adjacent to the affected tendon with a solution consisting of 20% glucose/0.1% lignocaine/0.1% ropivacaine weekly for four to 12 treatments, using the technique described by Lyftogt.18 The tender points were most commonly the anterolateral and anteromedial margins of the tendon and on the most posterior aspect of the tendon 2–7 cm from the calcaneus
attachment. At each point, 0.5–1 ml of solution was used to a maximum total of 5 ml.”
On average took near 10 treatments.