Pain after hernia surgery is common. Transcutaneous nerve stimulation (TNS) seems to help post operatively and one wonders if it might have lasting effects. I was always taught that one should not do a procedure unless one can deal with the common complications. If a procedure has a “common” risk of pneumothorax, then one better be able to deal with it. It then follows that surgeons should not be doing hernia repairs because they do not know anything about dealing with the pain afterwards.
Pain Common Post Herniorrhaphy
Studies of post Inguinal Herniorrhaphy pains vary widely because drop out rates can be over 1/2 of patients (they might include mad ones who don’t want to deal with surgeon as well). One study with 80.8% retention found the following one year later:
“Pain in the groin area was reported by 28.7%, and 11.0% reported that pain was interfering with work or leisure activity.”
Postherniotomy pain is a neuropathy
Study in press analysis of postherniotomy pain found good evidence for it being a neuropathy:
Pain in press 2008
Neurophysiological characterization of postherniotomy pain
Eske Kvanner Aasvang, Birgitte Brandsborg, Bente Christensen,Troels Staehelin Jensen, Henrik Kehlet
Better Surgical Management may help Central Mechanisms of Persistent Pain
I have recently seen two cases of bilateral hernia repairs. Both developed moderately severe pain and were treated quite cursorily by their surgeons. One was done many years ago and the patient has been suffering all this time. The other was done recently where pre-emptive analgesia should have been done. During anesthetic induced sleep, the spinal cord and brain is still barraged with pain messages which induce permanent changes heightening sensitivity to pain in that segment. One can prevent this by certain maneuvers – simply injecting local into the tissues to prevent barrage, or by administering ketamine before and after surgery which blocks NMDA pain pathways some. Work has been done on this “syndrome” by Dr. Joel Katz at York University in Toronto; he has been particularly interested in phantom limb syndrome. Perhaps post-op TNS can do this:
J Pain. 2008 Apr 1 [Epub ahead of print] Hypoalgesic Effect of the Transcutaneous Electrical Nerve Stimulation Following Inguinal Herniorrhaphy: A Randomized, Controlled Trial. Santana JM, Filho VJ, Guerra DR, Sluka KA, Gurgel RQ, Silva WM Jr.
“In the group treated with active TENS, pain intensity was significantly lower 2 hours (P = .028), 4 hours (P = .022), 8 hours (P = .006), and 24 hours (P = .001) after the surgery when compared with the group that received placebo TENS.”Other Pain Mechanism
Other mechanism for persistent pains include local nerve entrapments and damage.
The nerves (genitofemeral and ilioinguinal) can be entraped in the hernia mesh and sometimes the mesh can form contracted plugs called Meshomas.
Scar Pains
Scar itself can generate persistent pain and there is a whole school of thought about how scar pain can cause widespread hypersensitivity (in Neural Therapy). Pure scar pain is an intradermal problem as most skin nerve are very close to the surface. Injection there requires the needle to be injected near parallel to the skin and blebbed up white as injection is moved up the scar. It helps to pre-bend the needle so it is easier to get parallel.
Nerve entrapment and Neuromas
Cut or entrapped nerves have point tenderness and perhaps refer pain or tingling. An aberrant nerve can form a bundle called a neuroma which is very tender. Steroid (Kenalog/triamcinolone) Injection is sort of neurolytic and can help dissolve neuromas. Steroids can also dissolve fat which would help free up the nerve as well. I inject Kenolog 40 mg. into these areas. More definitive approaches include cryotherapy (only temporary) or alcohol injection(permanent) into the offending nerves. One recent article used an implanted electrical nerve stimulator.
Myofascial & nerve tender areas
After scar work, one is often left with sensitive spots and surrounding soreness. I have been trying 5% lidocaine shots repeatedly to these areas; this strength is sort of neurolytic (nerve damaging) and can knock out the nerve for 3 wks – 6 month. I give them repeatedly (patients actually X the spots they want hit).
Posterior Segmental treatment
You, however, will not get the results you are looking with just that approach. I remember one clear cut case of purely post surgical unilateral inguinal neuropathic pain. I coud skin roll tender tissues all the way around to the back to the segments that feed the damaged nerve. There was muscle spasm paraspinously at that level as well and the segments were stiff. Subject had never had any back problems. When one thinks about it, it does not take much of a stretch to realize that if the anterior nerve is damaged, its companion dorsal nerve that feed the paraspinous muscles and tissues would also be effected. The reverse happens too. I recently saw one lady with anterior T7 rib pain. When the T7 paraspinous levels were needled free, the anterior rib no longer hurt (other reasons why that could have worked though).
This posterior paraspinous – anterior segment connection was noticed in the 1970’s and before by Dr. Chen Gunn from Vancouver. His successful research on WCB cases demonstrated that needling back and peripheral sites was imperative to successful treating back radiculopathy and arms pains (resistent tennis elbow included). I was so impressed by his work, I have spent time at his office twice in the last 25 years. Best needling spots were the rotatores over the facet joints. Some of them were very scerotic and hard. When needled and working out, caused significant benefit.
In the cases of inguinal nerve damage, it is easy to realize the nerve damage. Through keen observation, Dr. Gunn was able to demonstrate clearcut evidence of nerve damage in cases of paraspinous – peripheral pain. Paraspinously, there could be edema, now known as neurogenic inflammation from neuropathy – you can spot it by pressing a match head into segments. Still not impressed? Many times I have seen peripheral problems and checked around the back to see what it looked like. If you will look, in some cases you will find there is no hair at the involved segments – something Dr. Gunn taught but never ceases to amaze me. The hair will be in segments above and below and you know that has to be neurogenic. The facts the levels are spastic and tender helps too. The tender muscles in the arm or leg will often conform to certain spinal levels, another confirmatory sign. Dr. Gunn also reported that back pain subjects with tender muscles down the leg (again found to conform to certain spinal levels) will take almost as long to recover as frank radiculitis (sciatica).
Resetting Segmental Sensitivity
I have a recent case where I did the local injections with some results but didn’t get good results until I needled the tender segments in the back as well. Confirmation, I believe comes from an unlikely source -Pulsed Radiofrequency Lesioning of the Dorsal Root Ganglion. This is heating up the nerve center (ganglion) for peripheral nerve at its nerve central in the holes (foramen) leading out from the spinal vertebrae. The pulsed heat is often 60 degrees C which can disrupt the nerves some but not destroy them (there is no numbness or weakness resultant). This seems to “reset” the sensitivity of this nerve center. and give relief for months.
recent study:
Pain Physician. 2008 Mar;11(2):137-44.
Response to pulsed and continuous radiofrequency lesioning of the dorsal root ganglion and segmental nerves in patients with chronic lumbar radicular pain.
Simopoulos TT, Kraemer J, Nagda JV, Aner M, Bajwa ZH. abstract here
article here
I suspect repeated electrical segmental stimulation can also cause this resetting of sensitivity and is much less invasive. Knocking out peripheral muscle triggers by directly needling, can make it potentially more lasting as well.
Surgeons Should Do Better
The vicitms are treated poorly by insurers if they are unable to work because the insurer’s “book” says the patient should be better by now. Any rational person would realize that the situation must be more complicated then just post surgical soreness but I am expecting too much from insurers. I would have expected more for the surgeons who try to tell the patient they are fine (or I don’t know what the matter is so I will tell the insurance company nothing of benefit to them).
I have not gone over all the available treatments (eg – if pubic joint tender then have to consider SI joints). I would be interested in other people’s successes.
addendum:
I have had a request for treatment options.
- It has been recently suggested that surgeons remove the ilioinguinal nerve during surgery and be done with it:
Ilioinguinal nerve excision in open mesh repair of inguinal hernia—results of a randomized clinical trial: simple solution for a difficult problem?
The American Journal of Surgery, Volume 195, Issue 6, June 2008, Pages 735-740
Fatemeh Malekpour, Seyyed Hadi Mirhashemi, Esmaeil Hajinasrolah, Nourollah Salehi, Ali Khoshkar, Ali Asghar Kolahi – “Chronic postsurgical inguinodynia was seen in 6% of patients in the ilioinguinal nerve-excision and 21% of the patients in the ilioinguinal nerve-preservation group (P<0.033)”
Several thoughts on that:
- I’m not sure I would have a hernia repair knowing there was a 1/4 chance I would end up with chronic pain. [Their review of literature gave a 25% rate of chronic pain after – do surgeons tell people that???]
- Removal of the nerve obviously helps a great deal but would the ones who got it following removal be more difficult to treat
- I’m not sure I would have a hernia repair knowing there was a 1/4 chance I would end up with chronic pain. [Their review of literature gave a 25% rate of chronic pain after – do surgeons tell people that???]
- Hernia recurrence needs to be ruled out:
Chronic Pain after Inguinal Herniorrhaphy
Journal of the American College of Surgeons, Volume 205, Issue 2, August 2007, Pages 333-341
George S. Ferzli, Eric D. Edwards, George E. Khoury
They suggest: “Hernia recurrence may be a source of chronic pain and should be ruled out early in the evaluation. CT may be helpful for establishing a diagnosis in cases of recurrence
that is not evident on physical examination. Some authors have advocated ultrasonography in these patients. MRI has also been used to detect recurrence, delineate mesh position, and demonstrate nonherniarelated causes of pain. Herniography has likewise reemerged as a useful technique in some of these patients.”
I think the first would be for the surgeon to fix his problem – a neurectomy.
The American Journal of Surgery 189 (2005) 283–287
Inguinal neurectomy for inguinal nerve entrapment: an experience with 100 patients
James A. Madura, M.D.a,*, James A. Madura, II, M.D.a, Chad M. Copper, M.D.a, Robert M. Worth, M.D.b
- Incidence in literature from 1- over 30%
- “Fifty-nine percent had pain that radiated to the leg, thigh, genital areas, or flank, and an equal number complained of activity-related symptoms.”
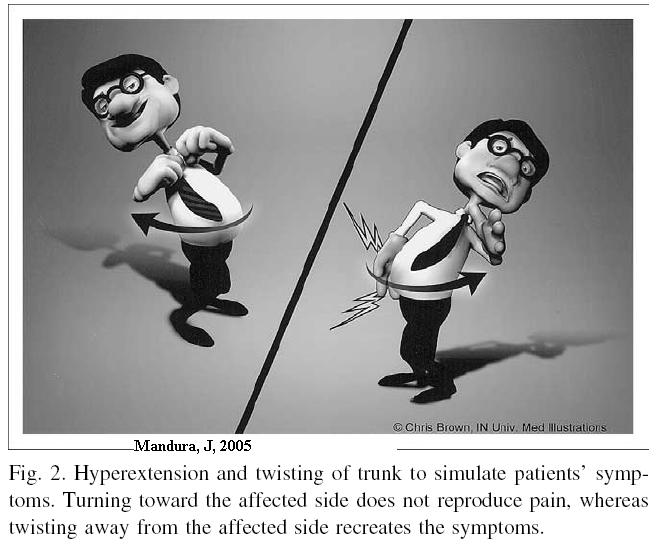
- Pain is elicited by twisting away from side sore (author has this cute pic)
- Diagnosis was confirmed by nerve block – most often it was the ilioinguinal nerve effected.
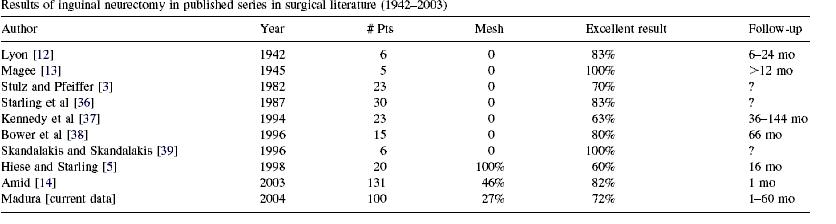
- Operation done was Neurectomy: “The operations were done under general (93%) or regional/ local (7%) anesthesia and consisted of identification of the nerves followed by proximal resection where they exited the internal oblique muscle near the anterior iliac spine or the internal ring in the case of the genital branch of the genitofemoral nerve. The proximal end of the nerves were crushed and ligated with fine braided polyester suture, followed by application of either absolute alcohol or 12% phenol solution to the nerve end to prevent neuroma formation.” They got :”Total pain relief was attained in 72% of patients, partial relief in 25%, and no relief in 3%.” The did a review of previous literature and came up with following:
- Concern they had was that the genitofemeral and ilioinguinal nerves can interconnect in some people so you have to know what you are doing and get adequate relief from local injections before surgery so know where to operate. Apparently only 20% of nerves in area are anatomical
Please Note. I realize this is a serious problem and have written a series of article about this condition which is available here:
Post-hernia Pains

my leg pain was there as soon as i came to told the doctor his answer was may have to open you up again a neuolagist came he said its just supperfisal few days it will be gone its 8 yrs now pain is mostly at left side of the knee i lost a lot of musele in the leg and the tingleinggoes down to the foot is there any hope of a cure
Ten weeks ago I underwent Bilateral Open Inguinal Hernioraphys. The left was a recurrent hernia from the initial repair in 1971 and the right a primary hernis. Both were done open vs laparoscopic and both were treated with the plug and patch method. plugs inserted in the inguinal ring and patch to close the abdominal defects. I had what I considered a normal post op course at the age of 61 years. The original preocedure in 1971 was done without mesh and plugs for that was the common approach then. I had no issues and recovered quickly. Seven weeks after surgery this time I began to develop shearing, sticking, stabbing, burning and acheing pain at the lower end of the incision on the recurrent repair in to and including just above the scrotal area and in to the groin and at times down the medial side of the upper part of my leg. Diagnosis made, Post Hernia Pain Syndrome that has been almost intolerable. Sometimes it’s positional so I can illicit the pain. I know it’s the ilioingiunal nerve entraped in either the mesh patch or scar tissue. It may be irritation of a suture knot or the plug irritating the spermatic cord. Recently beginning about five days ago when I thought the right primary repair was just about all better I began having a little of the same symptoms at the highest point of the incision and above but this has not bothered me all too much. I went for a second opinion yesterday with a very competent General Surgeon who does a lot of hernia repairs. He did an ultrasound and examination and determined that the blood flow to my left testicle is in tact which probably rules out strangulation of the spermatic cord. Both hernia repairs are intact and no recurrence noted. He believes that the the nerve is being irritated by a large lesion of scar tissue and he injected me with a mixture of marcaine and kenalog. He sted that the pain would be gone in about a half an hour but would return and the Kenalog would begin breaking down the scar tissue. He did state I might need another injection but he feels that his would solve the problem. He also stated that because the symptoms occurred seven weeks after the surgery the prognosis is actually better. The pain after injection did not go away to any extent and today I am slightly better not appreciably. I only hope that the kenalog will begin to break up the scar tissue because quite frankly I don’t know how much more of this I can take, Other’s I have spoken with inform me they would not reoperate for one year to either explore or replace the implants. The original oiperative surgeon wants me to return in two months if the pain does not get better for an alcohol injection to deinervate the nerve. Basically kill the nerve. I thought that this was going to be a “slam dunk”. This has turned out to be a problem that I cannot imagine having for very much longer. Trust me on this I am not waiting two months if the procedure I had yesterday doesn’t work.
Who wrote this article? Individual or group? Surgeon, pain specialist?
Fabulous, to the point and need I say….finally someone who is thinking!
As a caregiver to a loved one in this exact situation: inguinal hernia repair with mesh, mesh removal/tissue repair only, triple neurectomy…..the ‘Pain Medical Musing’ hit home! Fortunately or unfortunately every detail was assimilated and appreciated!
We are still…….researching, reading and absorbing to assist my patient in a possible resolution to the severe ongoing, totally, debilitating pain.
Please contact ASAP if you or yours are working with neuros/pain specialists focusing on this specific type of paitent. Where are you located? Speaking for another in pain who’s only wish is for their ‘life back’! Thankyou LAS
It’s official – patients are not being told about chronic pain being a complication:
Ann R Coll Surg Engl. 2008 Sep 15.
Consenting practice for open inguinal hernia repairs – are we failing to warn
patients of some serious complications? Hoosein MM, Towse H, Conn G, Stoker DL.
Chronic pain complications were entered into consent in only 16% of cases- shame on them…
I hope that it’s not just “open” inguinal repairs being focused on because I had a laparoscopic inguinal & spigelian repair done in June 2006. I have had chronic hip, groin, and thigh pain since 2006. As soon as the pain started, I was sent to a Physiatrist. After one successful pulsed RFA which lasted many month’s before the pain returned with a vengeance. I’ve since had pulsed RFA’s at L1/L2, and many in the abdomen by the iliac crest(targeting the specific nerves), TPI’s also targeting the nerves by the iliac crest, and an ESI at L1/L2/L3 which were all unsuccessful to treat the debilitating pain that I deal with. My surgeon never mentioned any possibilities of post hernia surgery pain. I was recently sent back to him after having had laparascopic oophorectomy surgery with adhesions entrapping the ovary and adhered to the abdominal wall. My OB/GYN surgeon sent me back to the (hernia) surgeon, with pictures in hand, because of large abdominal adhesions located at the hernia repair site. He recommended ahesion lysis surgery, along with a triple neurectomy. My Pain Mgmt. Specialist had already discussed a neurectomy as a possible treatment but advised against it because of the chances of neuroma formation. Once again, the (hernia) surgeon did not inform me of the risk of neuromas until I brought it up when he recommended the lysis surgery and triple neurectomy. Then, when I asked him what the success rate was with the triple neurectomy for relieving pain, he stated it was 33% chance of being successful, 33% chance of no change in pain, and 33% chance of being in worse pain. Unless the patient knows what complications can arise, and knows what questions to ask, we are going into surgery “uninformed” and “ignorant”. I think it’s a sin for doctors/surgeons to not tell patients, up-front, the pro’s and con’s of the procedure prior to surgery so that the patient can make an informed decision.
I am scheduled for bilateral inguinal hernia repair next Wednesday. It is not reassuring that the surgeon didn’t mention a word about post-operative pain. I was instead provided by the front desk with two pages of “patient information” and “risks involved in inguinal hernia repair”. The first describes nausea and pain and the need for catheterisation. Post op pain relief is suggested at three levels, Paracetamol, NSAIDs and Tramal. The second sheet lists (in order) bruising, urinary retention, persisting long term wound pain, nerve entrapment effects, infection of the mesh, hernia recurrence, damage to T artery and the vas. It concludes with “this is not a complete list”.
My response is memory of what a long-term hernia did to my grandfather, and how uncomforable I am now… my activities are severely constrained and my bowel behaviour restricts socialising. Lastly the same surgeon comes highly recommended, not just general comment, but because he did the same procedure on my 20 yo son 5 years ago and with it seems no long-lasting nasties. So I’m going ahead with my eyes open. That said, I’m now interested to ask whether he will use local as well as the planned general anaesthesia (I gather the item number suggests so), and what his position is on neurectomy… which doesn’t sound all that smart. I gather NSAIDs are highly recommended, but never take them otherwise for preference; they cause tinnitus big-time.
I’ve only had this condition for a month… at 63 I got involved in an aggressive fitness program, and the personal trainers who programmed my course with lots of weights and twisting (to improve my flexibility!), didn’t mention the risks of hernia, let alone a double-whammy !!! What a high price for trying to lose weight and get fit !
There’s lots of media attention about the multiple risks of obesity (my BMI is 30) but nobody mentions hernias as a VERY good reason !!
Do I want to trade my clear new diability now for 25% probability of long-term pain? Not particularly, but I guess I don’t have much choice. I even more like the idea of losing weight and getting fit, but have mixed feelings about the higher risks of recurrence if I do.
Thank you for the insights. I feel better prepared and I might be able to describe any effects with better precision.
Last query, I’m assured this procedure takes 35-40 minutes each side. It seems rushed…. like e.g. if it just needs more time to better “realise” the location of the nerve trunks; or better visualisation methods e.g. EMG field maps etc etc. I will watch for replies.
Postoperative pain musings…. a follow up
The Lichtenstein procedure for inguinal hernia repair seems to be very common, and given one is faced with a lifetime of discomfort most
patients would accept the terms of the repair. As a recent bilateral recipient, I observe that the ligitimacy of the procedure nevertheless
seems to depend entirely upon the effectiveness of post-operative pain relief and a variety of measures were suggested. These have the side-
effects of either causing irreparable damage to the liver, the kidneys, acute stomach distress, or in the case of opiates, massive effects of
nausea, which needs to be treated separately, all making for a cocktail of untoward effects and no perfect pain relief. This limits the likelihood that the patient may obtain full benefit from the repair. Several issues become salient: Patient pain threshold (and the number of days/weeks/months it takes for the pain to subside below the threshold). So paracetamol may be the primary pain relief choice, the lower the threshold the more likely the patient is to suffer irreparable liver damage. The nausea in turn may cause runaway effects of pain if the body flexes and pulls on the sutures accelerating the possibility of infection of the wounds. I can more clearly see why some patients report the cure far worse than the complaint. I have no idea whether the state of pre-existing liver damage was assessed in my case, but if it was, everything else suggests it would have been given scant attention. Perhaps the most distressing other symptom is the bloating of the abdomen to the extent of complete lack of motility for two days which still existed when I was sent home. Multiple suppositaries and enemas were tried in the simplistic belief that the rectum was the site of the blockage. Only at home after using multiple laxatives does it appear that the blockage has shifted. Overall, one has the impression that the surgical team were interested only in one thing in which they can take pride, and the nursing staff engaged to relieve the pain as much as possible until the patient opts to go home with his gigantic medical bill.
Beyond that, the patient is on his own or encouraged to consult his general practitioner for alternates to the obviously already exhausted list of medications. The severing the ilio-inguinal nerve is a pretty sure sign that this is a very expedient but necessary maneouvre (legitimising the procedure) to reduce post- operative pain and only after the procedure, does the patient learn that part of his body will never likely again feel part of his body. It is really cold comfort that the penile nerve remains intact.
The pre-surgery literature certainly warned this patient of pain, but the scale of pain was never mentioned. If the spectrum of pain spans 100 dB, then in my 64 years, I might have experienced 30 dB pain, but certainly not the 80 dB pain I have experienced on the third day after the
internal analgesics had worn off. One is inclined to think that these days are akin to the dim-dark days of surgery e.g. when another surgeon
as famous as Lichtenstein conducted tens of thousands of lobotomies…. What will replace it…? at least the offer of a pain pump one could hope
for localised analgesia. Better still, the general practitioner who was consulted about the individual about engaging in a strenuous exercise
program for such a patient, might caution him of the risks of hernia. We hear of multiple risks of obesity, but does any of these lists contain
the risk of hernia which is evidently so common?
It is now the 6th day following the bilateral procedure, and I reckon I’m through the worst phase of pain and uncertainty. I think in hindsight the trauma and panic attacks could have been substantially lessened if the surgeon had provided more information concerning key aspects of the surgery and recovery:
1) The information sheet talked of expecting pain, but not specifically the expected time history and the level of pain. The local analgesia wore off on the third day and I experienced considerably more pain (on a log scale) than ever before experienced. My experience was that the morphine injections worked, but the oxycodone didn’t really attack the sharp pain much, it more made one less bothered by it. The pain miraculously dropped on the fourth day, but everyone asked was completely evasive about when that stage might occur.
2) What I was not prepared for was the extent that the bowel motility would be affected. It essentially shut down for three days before the operation (I expect due to the herniae interfering with flow) to 5 days after the operation. This wasn’t painful so much as acutely distressing, particularly since I had residual feelings akin to the hernia itself, as if the operation had not been a success. One would have liked more information showing the likely causes, e.g. I’ve come to understand opiate use strongly kills peristaltic action and the strengths of the surgical technique. Evidently this is less likely to be at fault, since the procedure is so common. Only sketchy information about the procedure was provided so that one could easily build scenarios about why it might have failed, e.g. a hernia still exists accounting for my residual feelings and continuing to choke off the flow.
3) I wasn’t prepared for my blood pressure to be rising 170/100 for all day on the fifth day after surgery and lingering on today 6th day, accompanied by arrhythmias. My heart has always been as steady as a clock, and this is worrying. What was more worrying is that the key people and institutions for my private patient care were not available to even assess the extent of any problem. I would have to get myself to an emergency department in another hospital to be assessed. It was only my local pharmacy which informed me that NSAIDS raise blood pressure, so I decided I must get off the Celebrex. I wondered what could produce a reduction of inflammation, and I thought ICE. I have used an icepack for two days wrapped in linen and it has been absolutely as effective, without the nasty side effects. The severing of the ilio-inguinal nerve is disconcerting, but it had a secondary benefit that I was not bothered by undue chilling of the icepack. The blood pressure has dropped to 164/99 and still with arrhythmias so I am concentrating on relaxing as much as possible and doing my leg exercises.
After reading Kim G,s post I am 100% sure this is why I have been suffering since May of 2007. The doctor who did my open repair treated me so bad. He refused to believe I was in so much pain after the repair Mine was open. I since have had a surgery simaliar to Kims and the results were almost the same Exstensine adhesion,s on the side of repair. After reading this post I am now sure that most of my pain is due to the hernia repair with mesh and I will be seeing a new surgeon.
Can you refer me to an MD/surgeon who specializes in nerve damage from my inguinal hernia surgery on my right side? I have had 2 surgeries by the same general surgeon, one in 12/04 and one last month 3/09. I am still experiencing pain in my groin area that feels like nerve damage, numbness and dull aching down my right leg to my toes. I just started reading about the problems this week associated with hernia surgery, to try and figure this out. I live in Orange, Calif 92865
Any help you can give me would be so appreciated
I have had open bilateral inginial hernia with mesh surgery left in Sept.2006 right in Sept. 2007,I have burning or tearing or sharp pain from the right side in the area of the incision ever since the the right side was done ,I got pain in the testical and groin area on the left side and pelvic region of the incision in July 2008. I went back to the surgeon who performed both operations and he said it was the nerve,he never told me why the nerve was inflammed or irritated,it flared up again in March 2009 I found out why there is a problem that adhesions have developed.The surgoen and my PCP knew this and never told me the possible complications that could occur after letting him operate on me.
I would have liked to have made a more informed decision as to what proceedures to have done.All I was told by the surgeon was that he was going to make me stronger,I am NOT stronger I am in pain if I engage in too much physical activity.
very interesting read, i’m on 4days after left side inguinal hernia repair with incision and mesh. No full anesthesia. 2mornings after surgery, after waking up the 2nd time, the back of left knee was in pain, could not straighten or bend over 90 deg. Called in to doc in morning and went back to hospital for a venus doplar check for a blood clot. It was negative. Now 4 days later and this afternoon, pain persists, but additional pain above the left knee cap, extremely painful, tender to the touch, and a bit inflamed. Doc never mentioned any to these type pains, just take some extra aspirin. So next move?……dunno
I had 2 types of hernia surgeries done when I was younger. 2002 & 2003. Bother inguinal hernias. The other one I had where they make one big cut around the groin area in insert mesh. I had the one where they make 3 cuts in you then slide the mesh around. It has been many years now. 3 years after surgery I started developing muscle spasms in the groin area where the hernia was repaired. Now I have swelling and constant pain for the past 2 years. I have to go to the bathroom a lot now and I’m in extreme pain sometimes. I have a weak stream when i urinate now. I constantly have to go to the bathroom due to swelling in the bladder area. If you have any help on what I can do please e-mail me. Sometimes it gets very bad and I have to take a lot of ibuprofen until some of the swelling goes down so I can at least work. Please help if you have heard of this before or anything. Any kind of information would be nice. I’ve been to a few doctors in the past and they didn’t know what it was. I had 1 doctor give me motrin 800s made me take 2 the first day then 1 each day for a week which took down an immense amount of pain. I want to feel normal again. Any remedies, doctors, ideas, or if you’ve seen or heard anyone with this issue a few years of what ever after surgery would be great! gfgweedo@aim.com
Facing hernia op in about 1 month. I am interested in hearing more from Mr. Smith (and others) regarding the post-op pain and any nerve, or nerve damage, issues.
My husband, who is in his early twenties, had surgery for two inguinal hernias when he was in high school (caused from lifting too much weight). Now, several years after surgery, he still experiences severe pain, to the extent that he has to stop whatever he is doing at the time and try to find a position that decreases the level of pain. This makes many things difficult for us, when his pain interrupts his workday, our intimate moments, and every aspect of life. We find ourselves wondering whether surgery made things better or worse for him. . . Doctors need to better inform their patients about the possible results of hernia surgery. People have the right to know the facts and make a decision based on all the information, not just an empty promise that surgery will fix the problem.
I am shocked to discover all this information on post operative, long term pain. My mother 5wks ago had a quadrupal hernia repair. She spent just over a week in the hospital. Even though she was in unbearable pain and unable to eat, she was released. Obviously she ended up back in the hospital for dehydration and some fluid build up. She was released 2 days later. She is still in unimaginable pain. Myself I’ve suffered extreme leg surgeries leading to what will soon be an amputation. It kills me to see her suffer as I have for years. I cannot believe she wasn’t prepared for the possiblility of long term, constant and continual pain. She has already discussed the option of disability. She can’t believe the amount of pain caused by the surgery and is having a hard time with her doctor understanding the amount of paiin she is in. I think he believes her to be on the lower thresold of pain people, along with some other family members. How can you make an informed decision on surgery if you are not properly informed on the pros and cons of the results of hernia surgery. She 2yrs ago, suffered with colon cancer which is most likely caused the hernias. Had she known that this surgery would be this painful and considerably more painful than colon cancer surgery; I donot think she would have followed through with this surgery. So if her surgeon won’t consider other options to find out about the nerve pain consideration, won’t do an MRI or try the tens unit. Should she attempt other opinions from other surgeons? How long should she wait before she does? Any recommedations of surgeons who obviously are aware of these complications? It’s bad enough that one of us is living with the complications of horrible surgeries and unimaginable pain. She should be able to find some sort of relief.
I have had hernia surgeries very upset with the pain i have gone through, right side was done 3 times, after yrs of terrible pain, surgeon excised nerves, but did the surgery on the left side open cut and i am having terrible pain on that side, on ly this time the scar tissue is in the joint and is pulling on my groin. Would like some permanent relief.
i didnt have hernia operation. i had panniculectomy, which led to probably nerve entrapment. my surgeon also, did not believe me when i was telling him that i had severe pain. he kept telling me “the nerves were re connecting” or ” youre a slow healer” . finally, after a few months of my family doctor also doing other tests to rule out other causes of the pain, the surgeon guessed… that i had a trapped nerve. i asked to be referred to a neurologist. he basically washed his hands ofme at that point and said ” no neurologist would be willing to see you”… thank goodness my family doc, who was always very shocked at the surgeons bedside manner, prescribed neurontin for me. it helps a bit, but doesnt always take the pain away. some days, the medication does nothing. it also leaves me quite stoned most of the time. my condition has stolen my once very happy and active life away. it is all i can do to get myself to work. i am married for 33 years, have 3 adult children and a grand daughter. my family is my life! i was always thrilled to have our family together for dinners, barbeques etc. i used to love to ride on our motorcycle with my husband. i had many interests and was always enjoying one thing or another. all of this is almost non existant now. my fam doc referred me to a few docs who refused to see me, finally a plastic surgeon,who didnt want to deal with me himself, referred me to the pain clinic at the miserecordia hospital. they will start with trigger point injection next week and i am hoping and praying that this is the answer and that i will be able to start to get my life back. i have done alot of research on nerve issues caused by surgery, as well as the different ways to fix it. i am sooo upset that the surgeon was allowed to do this surgery even tho he was not prepared to deal with the possible problems that could happen.. and i am even more angry that he simply washed his hands of me, did not try and help me or refer me to other doctors for help. he basically said.. ” i cant help you anymore” . i have always been known as an extremely patient, kind , forgiving, understanding, funloving, happy go lucky woman….i truly felt like the surgeons trash, after this experience. the crazy thing is.. if he would have properly diagnosed me immediately thru proper testing, he then could have referred me to the pain clinic.. and i could have been living the last 2.5 years healthy and happy…. please, i wish to pass this on to other ppl dealing with unresolved nerve pain caused by surgery…. do research, demand help, ask questions, do not ever give up. peace to you.
p.s. i would like to hear from others who had nerve entrapment caused by surgery… tell me about the different treatments you had.. trigger point injection? other kinds of injections to kill the offending nerve? sugery to fix the problem? medications you were on? etc etc.. other ppl who had tummy tucks or panniculectomy? thanks…
had lap bi-lat surgery 3mnths ago rt side no problem left side ache just can,t pinpoint
source of ache.very depressed,does the problem sometimes heal on its own,god i hope so.don,t fancy anymore surgery.i don,t think i can cope with longterm pain.i feel such a mug for having the surgery
@ R marcussen: another mug!
I found this useful: http://emedicine.medscape.com/article/1234809-overview
The surgeon dismissed the possible complications in the ten minutes I had to decide and then he dismissed the very clear symptoms of nerve damage and pronounced himself satisfied (self-satisfied?) with the scar which I had said I was not concerned about.
I am in severe and extensive pain the result of nerve damage (which they kept jolly quiet about) and with a major route for nerves going through the femoral area, Id say that would have been worth mentioning.
Many many thanks for the article Anne Coll:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2727805/?tool=pubmed
Also a related one about post hernia repair pain from Denmark:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421158/
This is not the slam dunk surgeons appear to think that it is.
It’s a pity they dont have more respect for the lives of their patients.
I just had an inguinal and femoral hernia repair on the left side August 10, 2011. I knew what to expect after surgery as I had this same surgery in 1987 on the right side. The 1987 surgery and post-op was uneventful and I was up doing my normal activities within a week with no return of a hernia since on that side. This 2011 recovery has been the opposite and the only thing different in this surgery is mesh this time. The pain, all within the groin, hip and thigh area, I experience can be excruciating at times to where I can’t move until it passes. I am completely baffled by this, as this is not even close to my first rodeo in the arena of surgeries, and I don’t understand what has happened. My doctor states that I “do not have any padding,” meaning that I am thin and that is why I am experiencing the pain. He states that if I am still having pain at 6 weeks post-op that he will send me to a pain management specialist. Really? This is considered the most common, routine surgery performed. I fear there is a problem with the mesh used and I wish I had the option to do this without mesh. I don’t know what else to consider to be the difference other than the mesh used.
Though it have gotten a lot of obsolete article, but it actually compensated for my time. I am going to post a link to this page on my site. I am sure my visitors probaly show that very useful.
One of my big concerns was that there were so numerous things to larn.
I just wanted to develop a simple message to be able to express gratitude to you for all the pleasant advice you are writing on this website. My time consuming internet lookup has at the end of the day been recognized with incredibly good strategies to write about with my colleagues. I ‘d claim that most of us readers actually are unquestionably blessed to exist in a great website with many outstanding professionals with very beneficial ideas. I feel really lucky to have encountered the webpages and look forward to so many more amazing moments reading here. Thanks a lot once more for everything.
I had a right inguinal laproscopic surgery in April of 2010, aside from minor discomfort for the first few months I thought I was doing well until yesterday. I went on a 2 mile hike and came back to discover my right testicle was aching. I recognized the pain as the same as it was the weeks after the surgery. It feels like someone hits you in the testicle but you get this feeling just from moving it or touching it, like its super sensitive. There is no discomfort when using the restroom, but I’m 28 and I have read horror stories about guys losing their testicles to torsion issues or having permanent nerve damage for years. I just want this pain to go away. I could barely walk. I am taking anti-inflammatory hoping maybe that will solve the problem and that it is just scar tissue that was agitated. I wish you all the best of luck in figuring out whats going on with you.
Hi Mark,
I was just wondering what happened with your pain as I’m a similar age and worried what the future holds for me. Did it by any chance resolve on its own?
Best
I had bilateral inguinal hernia repair done Dec 27,2011. After being seen by multiple general surgeons before hand and being miss diagnosed with a sports hernia (rectus abdominal tear) I had a dynamic ultrasound done that showed 1 large direct hernia Nd 1 small indirect hernia on my left side and a small direct hernia on my right side. Dr Falvo out of Henry Ford Detroit performed my surgery. I feel no pain on my left side which kept me out of work for 3 months. However the right side I am having some dull pains everynow and then. The right side didn’t bother me at all but I figured id get it done now while I am young (26)
my hernia opration was successfully completed on june 2006. now i got marrige on 6 may 2012 plz tell me is hernia create any problem,s for my future …i am very well this time .
my hernia opration was successfully completed on february 2005. But now a days i feel very pain . I was consult to doctor (physician) ; they told me your operation taka has break so you face this problem & he suggest me you can reoperation . Is this decesion right ?
plz guide me bcz wright now I am suffering very Pain.
Thankyou
I had an umbillical hernia following a anterior spinal fushion in 06 ‘ . I am now on my 9th day removed from surgery . I spent 24 hours as in-patient and while there was on a PCA. I was sent home using the same pain meds I have been on for several years following the 3 spine surgeries…I am have the WORST nausea you could imagine accompanied with A LOT server pain. I almost feel like I am being a pest as I have called my surgeons office almost every other day since I was discharged but from having many previous surgeries and knowing my body I am very aware that something is not right here. I have been running a fever albeit low grade 100-100.5 for a week now. The pain is at the surgical site (lap surg. right of umbilical) and I am extremely bloated. The pain then goes up toward my liver and down into my rectum and right testicle , I am also experiencing pain on my penis. These are all new symptoms. Like I mentioned, I have called the surgeons office several times even making a trip to the ER 4 days ago where all the test came back normal…ie: labs , CT w/ contrast and dye…My surgeon is out of town and it is Friday morning . I do not want to spend another minute feeling like this , especially the acid reflux and nausea but when I call over there I feel like his nurse don’t believe me and is talking down to me…Please bear in mind that I was a board certified M.E prior to my accident in 06’ .
I don’t want to break professional protocal by breaking the “Chain of Command” and seeing another Dr. but when is enough , enough. If I knew that this would likely be the complications I would have pondered on it a bit longer…
Please anyone thinking about having this surgery arm yourself with as much knowledge as possible and ask as many questions as you can until you feel educated enough to make this decision for yourself…..It even gets by us “Pro’s”
——————-
IN 2010, at the International Association for Study of Pain (IASP) Congress in Montreal, there was a Japanese poster using repeated acupuncture like Intramuscular Stimulation of various sore points on abdomen for treatment of chronic nausea. I was impressed but noted it took perhaps 6 treatments of multiple sites bilaterally. Maybe you should consider that…
Good luck..
admin
I had open groinal surgery repair six weeks ago. I have been experiencing stabbing burning sensations. I am worried that my doctor will send me back to work and it will make it worse. Over the counter pain mess don’t work yet surgeon won’t prescribe pain meds. In fact made me feel like I was doing something wrong by asking for them. I also was not told of these possible complications. I hurt myself at work and thus far workman’s comp has paid for everything. Will they still be responsible for anything else that I need if I have nerve damage?
————
WCB is either poorly educated or it suits them to assume any pain will get better with time so they can automatically terminate your claim over a certain period of time. My feeling is that any caseworker who takes this stance should have all his/her work reassess as it is likely faulty… and his/her superior should be told so. One really needs a lawyer to ensure proper treatment, sad as that is. In Canada, lawyers are hampered by fact many “independent” assessors really work for WCB and give ruling in their favor. Canadians might need either a sympathetic specialist or an assessment from someone in the states – someone a lawyer might be able to find… A pain clinic would be the place to go though waiting periods can be atrocious…
good luck
-admin
I had the very same operation around the same time ago 6 weeks give or take and I’m still experiencing intermittent stabbing and pinching pains throughout the day, nothing seems to bring them on no particular movement I’m actually pretty mobile with no pain it’s just happens sitting or even lying down in bed no rime or reason and I’m still a little swollen under the scar and they used mesh. sometime it almost feels like it’s on the serface like its the scar healing but at 6 weeks??come on? I’m hoping because the pain is at a lower level it’s just going to go away at a very soon point?? Am I joking myself? Where are you now with everything?
had surgery yesterday and just about to take pain-killer for moderate suffering. I take so many other things for AF etc so I have avoided pain-killers and truthfully the only pain -not severe- is around the wound. However my main concern is urinating which is very weak
Both the anesthesia and pain meds can affect your ability to urinate, you mentioned AF which usually implies you are not a youngster anymore, in which case the afore mentioned comment would be even more probable if you still have your prostate gland,these medications tend to clamp your prostate , making it difficult to urinate.It should get better once the anesthesia wears off, however pain meds can clamp you up as well possibly leading to a catheter. Be thankful you can pee at all, but if you need pain medicine you may have to take it. Sometimes a low dose of oral valium like 2 mg will help you relax and making it easier to pee, good luck!
I too suffer from chronic groin and testicle pain following the Classic Bassini open no mesh right hernioraphy, under local and regional block.Prior to surgery I felt I had done my homework, although in retrospect the surgeons initial exam was in my opinion nothing short of brutal, but I thought maybe he HAD to SHOVE his finger up my inguinal canal to feel exactly how large of a hole was there. I should have followed my instincts, but sadly I didn’t! My philosophy in medicine, is that it doesn’t have to hurt you to work!! If anybody is the fool, that would be me, as I am a board certified Emergency Physician. I perform many procedures on patients anywhere from suturing, insertion of chest tubes to reducing fractures and dislocations, and none of my patients suffer! Babies will fall asleep while I sew them up, and all because I don’t force things.They don’t even feel me injecting them with local anesthesia because I take my time and infiltrate the tissue slowly.Many of my peers just fire away causing great pain and subsequently have to hold the Patient down.I often wonder where they trained.Getting back to the issue at hand,I wasn’t told and my cursory research never said that one in four would end up with chronic pain. I would have given my hernia a name and watched for incarceration, which is really the complication you want to avoid, that would be an Emegency. Short of that I would have lived with it. I had it repaired electively to avoid it getting larger and most of all to avoid it getting incarcerated, many of which though can be reduced in the ER. Time is key if your hernia incarcerates, I would know! Anyway. my course of action after going on 8 mos now of feeling that iv’e been repeatedly kicked in the nuts, pardon my French, is to get an ultrasound of my teticles to ensure good vascular flow which will also rule out spermatic cord entrapment, start TENS UNIT therapy on my paravertebral region on my back between lumbar 1-2 , find a competent pain management Doctor with a soft touch who will then under ultrasound or fluoroscopy isolate the nerve(s) in question, and then inject that area with marcaine and depomedrol. My intense research now, shows that is MY best option right now for ME. The depomedrol dissolves fat which COULD alleviate the entrapped nerve. Usually it is the ilioinguiinal nerve that is most commonly affected. This has been a nightmare for me so far as I can barely do anything, including my work. After reading your attestations of your own misery, I feel terrible for all of you! I personally have had quite a few surgeries in my life, 10 knee surgeries, removal of a kidney after a fall, and many more, including the same hernia repair on the left in 1958 with no subsequent problems! This by far I think has been the worst. I will pray for all of you and try to keep you posted on my progress.Good Luck and God speed……..Dr. Rick . I am going to aggressively pursue this treatment plan before even considering any further surgery. No one person is alike, and this may not be for you, but at least you have a Physicians opinion on the subject, and what I plan on doing for my own Misery! You should always try and start with the LEAST invasive way before considering the more drastic options. I am a big advocate of the KISS (keep it simple stupid ) Principle……:)…………I am not looking forward to being shot in the crotch but I will be trying it in one week.
I had a lateral hernia surgery more than 10 years ago. I deal with pain everyday from it. It constantly feels black and blue across my stomach. And sometimes I feel like I have something caught under my rib cage………as a woman would feel in her late term of her pregnancy when a baby’s foot gets under there. Not comfortable.
Worst surgery I have ever had in my life………….and I have had plenty.
—————————-
One if the skin nerves that crosses above your lateral hip crest and enters your low abdomen was damaged – ilioinguinal or iliohypogastric.
I wrote about my experience with a crushed iliohypogastric nerve:
http://painmuse.org/?p=2924
One of the new techniques that I’ve found helpful is – neural prolotherapy.
You can actually feel the course of these tender nerves. I would inject every cm a bleb of 5% dextrose (I put in 3% glycerin too) – every cm or so along nerve from front to back – you will also inject a whole region with blebs 1 cm from each other in front where intense. This will give you temporary relief that becomes more permanent with repeat injections…maybe.
I suspect muscles will be very contractured by now and they will need work as well.
Good luck to you
admin
Hi all
I had Open Inguinal Mesh on ny Hernia in April 2014 and Still in Constant Paqin I .E Dragging pulling Sensation , Sharp Stabbing Pains ,Unable to perform physical Activities Cant work due to pain Currently now been signed off for 16 months now …
had 3 Nerve Blocks and 6 Trigger Point Injections 3 days ago and Pain seems to have gone worse now anyone else had this and still in Constant PAIN ??
Ethel Brown (who now lives in Australia) reported that after using Cellskin Gel on the patches of her skin that had shingles, the situation disappeared.
Thanks for finally talking about >Post Hernia Surgery Helped by TENS and Should Surgeons be Doing Hernia Repairs if They do Not Know How to Deal with the Persistent Pain Afterwards? <Loved it!