It was recently found that CRPS of leg might be obviated with attention to Superficial Peroneal nerve in shin by pulse radiofrequency. This is exciting news. I have a CRPS arm helped temporarily by nerve block to superfical antebrachial nerve in forearm. Question is, whether similar measures to Cutaneous Antebrachial Nerve (Thumb palmar side of forearm) would help arm.
Korean J Pain. 2016 Oct;29(4):266-269.
Reduction in mechanical allodynia in complex regional pain syndrome patients with ultrasound-guided pulsed radiofrequency treatment of the superficial peroneal nerve.
Chae WS et al
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5061644/
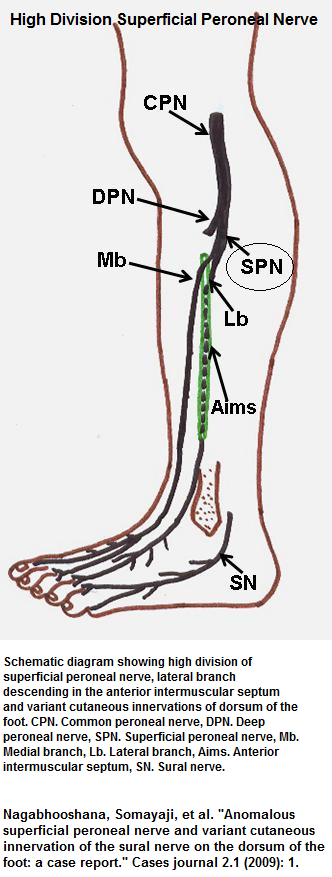
The superficial peroneal nerve comes down anterior shin and perforates fascia near ankle to feed sensory foot on top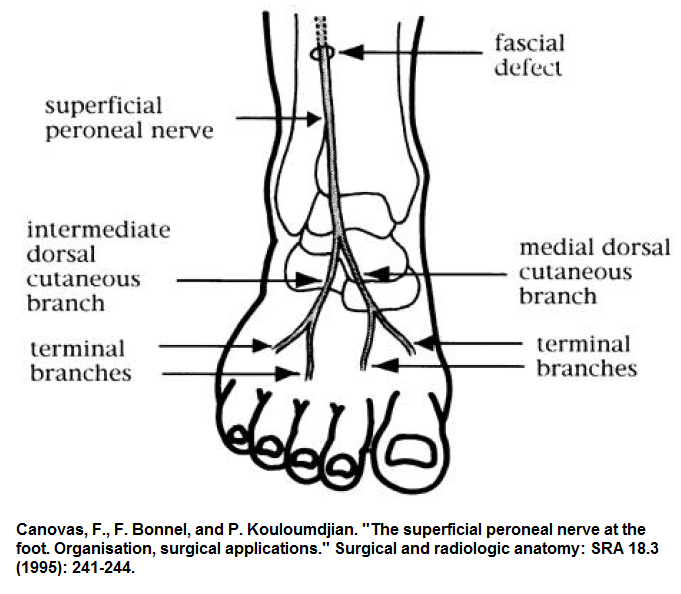 However, the fascial penetration can occur higher up in shin and is more likely to create problems there:
However, the fascial penetration can occur higher up in shin and is more likely to create problems there:
- CRPS type 2 for 1-2 years
- 2 leg cases with tactile allodynia (touch sensitivity) and coldness to dorsum foot and ankle – one with lightning jerk pains as well
- Pains running 7-8/10
- Mid calf US guided Superficial Peroneal Nerve block gave relief lasting few days so…
- Pulse radiofrequency technique”
“a TCU 410 TC-Electrode inside the 22G disposable cannula of 0.9 × 150 mm cannula with an active tip of 5 mm, and the electrode was connected to a radiofrequency lesion generator (Neuro N50, Stryker Leibinger GmbH, Freiburg, Germany). After applying local anesthesia to the skin, the needle was inserted under ultrasound guidance close to the SPN where paresthesia was reported at less than 0.3 mA. PRF was applied for 120 seconds at 45 V, with an electrode tip temperature not exceeding 42℃, and it was repeated three times.” - Pain was reduced down to 2-4/10 for 3-4 months
Comment – Peripheral treatments are being found valuable and may work even in later stages(I hope) and include topical ketamine, intradermal/subcut Botulinum toxin, lidocaine patches and now pulse radiofrequency. The latter, initially used on dorsal ganglion, but found to be helpful on peripheral nerves as well.
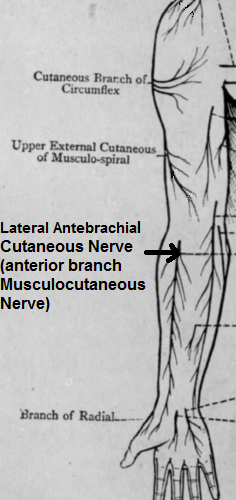
If one were to extrapolate to the upper limb, then for my case , treatment of the lateral antebrachial nerve might be useful. I have a case of arm CRPS ; temporarily blocking these skin nerves at the elbow allowed her to flex and near straighten her arm – something she would not have done otherwise.
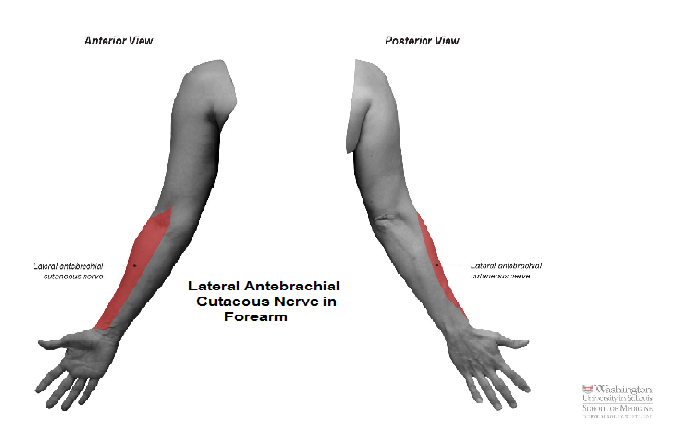 There are two lateral antebrachial nerves – about 1-2 thumbs breath apart; The posterior one is more related to tennis elbow case:
There are two lateral antebrachial nerves – about 1-2 thumbs breath apart; The posterior one is more related to tennis elbow case:
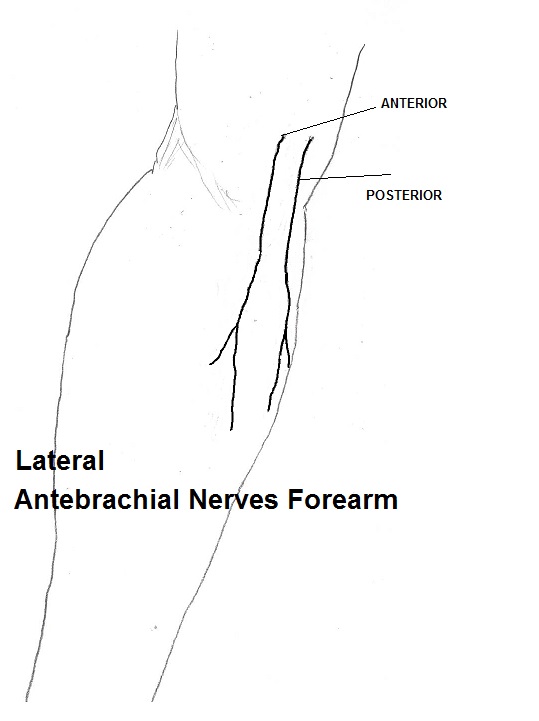 Anterior and posterior in one patient (blue circle lateral epicondyle):
Anterior and posterior in one patient (blue circle lateral epicondyle):
lateral cutaneous nerve forearm here:lateralCNforearm
The anterior one is more described in pictures:
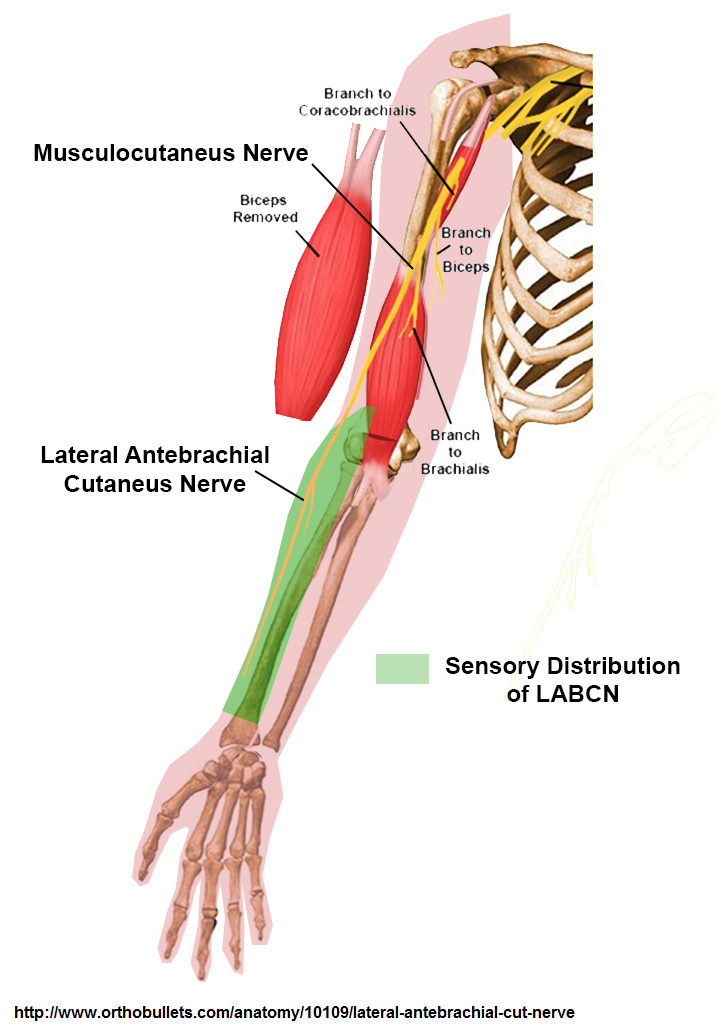
Originally this nerve comes off the Axillary nerve which in turn becomes the Musculocutaneous nerve then the Lateral Antebrachial which has an anterior and posterior branch.
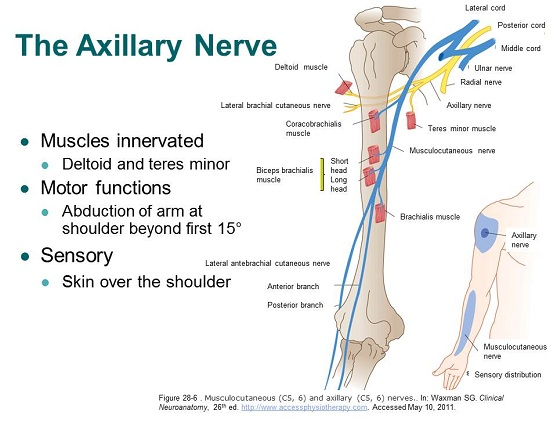 It originates of the Musculocutaneous nerve where it splits of just where Brachialis originates behind biceps mid upper arm:
It originates of the Musculocutaneous nerve where it splits of just where Brachialis originates behind biceps mid upper arm:
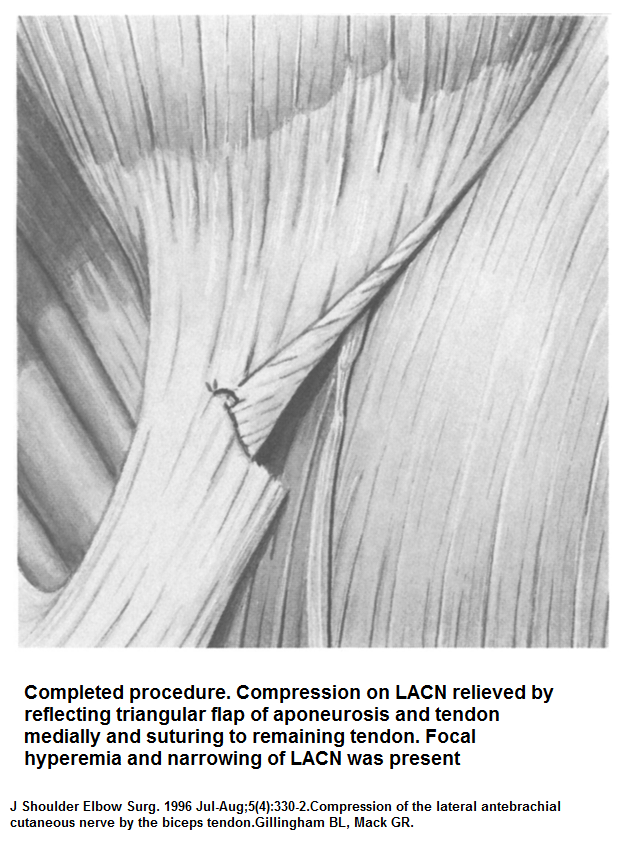
 This nerve has been noticed for its ability to be damaged by the lower tendon of the biceps muscle ( and release by cutting there slightly).
This nerve has been noticed for its ability to be damaged by the lower tendon of the biceps muscle ( and release by cutting there slightly).
Gillingham, Bruce L., and Gregory R. Mack.
Compression of the lateral antebrachial cutaneous nerve by the biceps tendon.
Journal of Shoulder and Elbow Surgery 5.4 (1996): 330-332.
https://www.ncbi.nlm.nih.gov/pubmed/8872933
(no abstract)
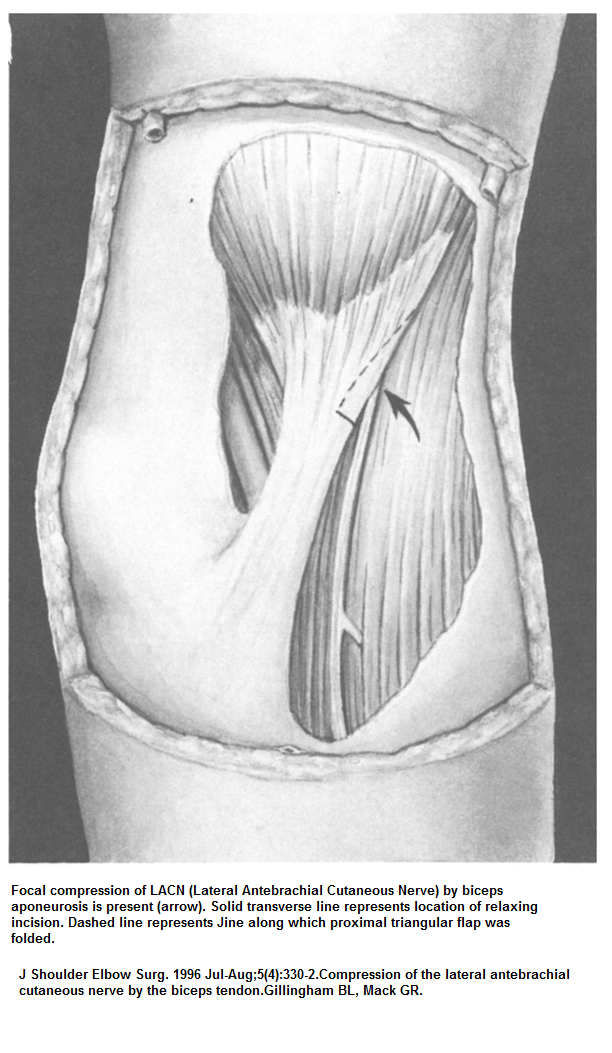
 Frank Neuropathy of the LACN at the elbow is characterized by:
Frank Neuropathy of the LACN at the elbow is characterized by:
- pain over the anterolateral aspect of elbow
- burning dysesthesia of lateral forearm
- worsening of symptoms by elbow extension and forearm pronation
- Physical examination may show tenderness and a positive
Tinel’s sign just lateral to the biceps tendon and
hypesthesia of the anterolateral aspect of the forearm. - Differential diagnosis includes
– lateral epicondylitis
– cervical radicuIopathy
– brachial plexapathy
– median neuropathy in the forearm. - their caveat: “A positive Tinel’s sign over the LACN and the characteristic sensory loss strongly suggest compression neurapathy; however, ENMG changes may be necessary to confirm the diagnosis. “
- 7/11 cases the above article had, did well with surgery.
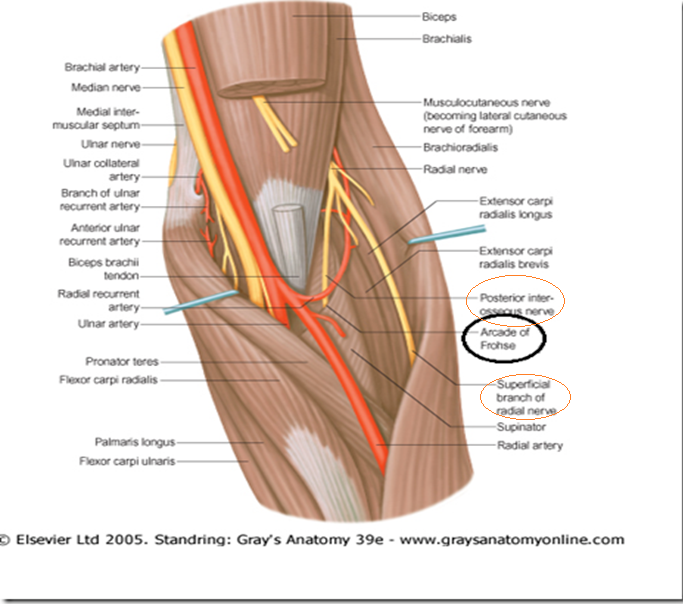
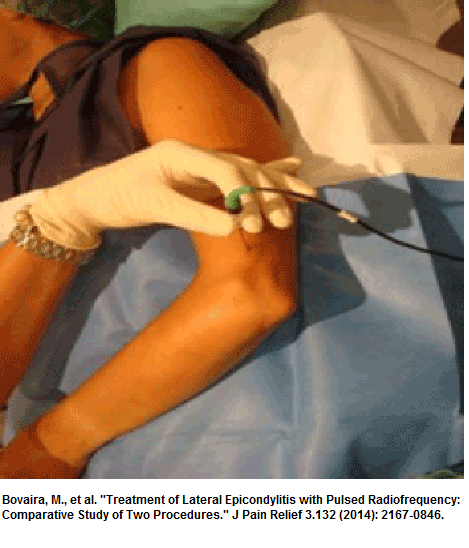
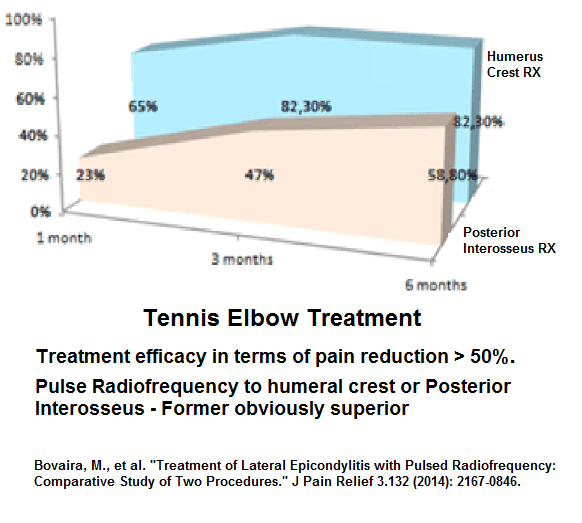
There has been an article using pulse radiofrequency for “cutaneous antebrachial dorsal nerve” for tennis elbow-and secondarily, in comparison, of the superficial radial posterior interosseus branch of radial. The radial nerve divides into 2 parts -the superficial radial nerve and the posterior interosseus nerve that goes under the supinator muscle. There is a fibrous arcade of Frohse at the entrance that can pinch this branch causing the posterior interosseus entrapment.
Bovaira, M., et al.
Treatment of Lateral Epicondylitis with Pulsed Radiofrequency: Comparative Study of Two Procedures.”
J Pain Relief 3.132 (2014): 2167-0846.
http://www.omicsgroup.org/journals/treatment-of-lateral-epicondylitis-with-pulsed-radiofrequency-comparative-study-of-two-procedures-2167-0846.1000132.php?aid=23195
Technique:
“Considering elbow innervation, PRF was applied to the cutaneous antebrachial dorsal nerve for two minutes, which is located on the humeral crest and constitutes the most extensive innervation of the epicondyle (Figure 3). If a trigger point was located at the level of the posterior interosseous, PRF was applied for two minutes.
PRF parameters were: 45 volts, 42ºC, two cycles per second, of 2 milliseconds each.”
humeral crest location: -PRF applied to the posterior antebrachial cutaneous nerve
posterior interosseus location
 Results – PFR to humeral crest far superior 82.3% still good results is 6 months
Results – PFR to humeral crest far superior 82.3% still good results is 6 months
Another situation in which forearm nerve were damaged was in Neuralgic Amyotrophy:
Abraham, Alon, et al.
Peripheral nerve ultrasound imaging shows enlargement of peripheral nerves outside the brachial plexus in neuralgic amyotrophy.
Journal of Clinical Neurophysiology 33.5 (2016): e31-e33
Neuralgic amyotrophy (NA), also known as Parsonage–Turner syndrome or idiopathic brachial plexitis. Rare.
- considered an immune reaction though there are genetic, infectious, and mechanical factors
- effects localized to the brachial plexus, although involvement of individual nerve branches (e.g., long thoracic, anterior interosseous, posterior interosseous nerves) seen
- symptoms -characterized by acute or subacute onset of shoulder and arm pain, followed by muscle atrophy and weakness, and variable sensory abnormalities.
TWO CASES:
#1 – – 32 yr old healthy woman
- subacute-onset severe left neck and shoulder pain. Shoulder pain switched in 24 hours by several days of severe left forearm pain graded 9/10 which gradually subsided over 2-3 week.
- Pain accompanied by the inability to extend the left thumb and fingers and intermittent paresthesias of the left forearm.
- Weakness persisted after pain gone; steroids helped pain but not weakness
- Findings – “radial deviation upon left wrist extension, accompanied by severe weakness of extensor pollicis longus, extensor indicis proprius, and extensor digitorum communis muscles. Sensation and deep tendon reflexes were normal.”
- Ultrasound study showed fusiform enlargement selectively affecting the left radial motor branch, in the proximal forearm,
#2 – 55yr old man with hx hypothyroidism
- subacute-onset severe right periscapular and shoulder pain, graded 8/10
- pain better after 2 weeks, but right hand weakness in addition to numbness in the distribution of the right C5 and C6 dermatomes
- “weakness in extensor digitorum communis, flexor pollicis longus, abductor pollicis brevis, and second flexor digitorum profundus.”
- Altered sensation at the radial aspect of his right forearm
- US – left median nerve fusiform enlargement in the antecubital fossa
On a similar note, A recent published did a continuous IV block of Superficial Radial Nerve:
J Pain Palliat Care Pharmacother. 2016 Jun;30(2):118-23. doi:10.3109/15360288.2016.1173755.
Ultrasound-Guided Continuous Superficial Radial Nerve Block for Complex Regional
Pain Syndrome.
Henshaw DS, Kittner SL, Jaffe JD.
https://www.ncbi.nlm.nih.gov/pubmed/27159548
- 42 year old lady
- CRPS type II after trauma from starting IV near superfi-
cial radial nerve - no response to treatments
- Pain described as “burning sensation primarily located in
the dorsum of the hand and in the forearm, with occa-
sional radiation to the upper arm along the track of
the radial nerve” - Pain primarily located in anatomic snuff box
- She had all the CRPS changes:
– modest muscle atrophy
– smooth skin
– decreased hair growth
– brittle nails
– finger pulp atrophy.
– hand cooler than other and cyanotic.
– Allodynia to light touch and clothing brushing
– radiography showed trophic bone changes. - ” a 9-cm, 17-gauge Tuohy needle was placed through the skin from the lat-
eral aspect of the forearm and advanced until it approximated the SRN. A 19-gauge, nonstimulating, open-end peripheral nerve catheter (Arrow FlexTip Plus; Reading, PA) was passed through the Tuohy needle and observed to thread in close proximity to the nerve” - Pump “infusing ropivacaine 0.4% with 0.5 μg/mL of clonidine at 6 mL/h. Intra-
venous ketamine was administered at 15 mg/h for the first two hospital days. On the morning of post block day 2, the dose was decreased to 7.5 mg/h and sub-
sequently stopped on the morning of postblock day 3 to allow for discharge home. Adjuvant medications included scheduled oral diazepam 5 mg every 6 hours, oral acetaminophen 1000 mg every 6 hours, oral tramadol 50 mg every 6 hours, oral pregabalin 75 mg twice daily, and oral celecoxib 200 mg twice daily. “ - on “postblock day 3, the SRN catheter was connected to an elastomeric (ON-Q; Halyard Health, Alpharetta, GA, USA) pump with 0.4% ropivacaine and 0.5
μg/mL of clonidine at 8 mL/h and the patient was discharged home.” On day 6 infusion stopped due to swelling. - pains were reduced to 4-5/10.
- “0.4% ropivacaine for the continuous infusion, as a dense sensory block was desired and excessive motor blockade was unlikely to be an issue. An infusion
rate of 6 cc/hour, increased to 8 cc/hour on postblock day 1, was again chosen based on clinical experience. Although a lower infusion rate may have been effec-
tive, we attempted to ensure complete nerve blockade while staying below a dose of 0.4 mg/kg/h, which is routine practice at our institution. Clonidine was added to the infusion mixture to improve block quality, which has been previously describe.”
————————–
I have been doing nerve blocks with 5-10% lidocaine which has semineurolytic effects which may make it last longer.
Using 5%:
Reg Anesth Pain Med. 1998 Jan-Feb;23(1):96-100.
The use of 5% lidocaine for prolonged analgesia in chronic pain patients: a new technique.
Choi YK, Liu J.
http://www.ncbi.nlm.nih.gov/pubmed/9552786
Using 10% Lidocaine:
Int J Clin Pract. 2008 Feb;62(2):248-54. Epub 2007 Nov 23.
Efficacy and safety of high concentration lidocaine for trigeminal nerve block in patients with trigeminal neuralgia.
Han KR, Kim C, Chae YJ, Kim DW.
http://www.ncbi.nlm.nih.gov/pubmed/18036166
I have combined this lidocaine with Pontocaine powder to make it 4% pontocaine in one ml solution. Pontocaine was found to have good semineurolytic as well properties:
Pontocaine was found to have good semineurolytic as well properties:
J Clin Anesth. 2002 Feb;14(1):39-41.
Intercostal nerve block with 5% tetracaine for chronic pain syndromes.
Doi K, Nikai T, Sakura S, Saito Y.
http://www.ncbi.nlm.nih.gov/pubmed/11880021
Another thing that I have done is to make a dumbed-down pulse radiofrequency:
- start a 20 gauge cathelon into nerve site
- insert a 2″ 25 gauge needle through cathelon.
- Inject the strong local to area
- using a pointer pulse acupuncture like device ( or an acupuncture stimulator if that what you have) hook up current from patient’s hand (hold a ground – can use a spoon with an alligator clip) and another alligator clip fastened to hub of metal 25 gauge 2″which it uniquely has.
- ramp up pointer pulse or acupuncture score to high level and run for 10 minutes – as tolerates ( if on approved machine for use in humans).
- I can get lasting relief lasting weeks or longer
Comment – hope this is of help in some cases – though for end stage, a spinal stimulator offers a good bet as well -though if localized to one nerve then maybe a peripheral nerve stimulator could be used.



Pingback: Hopeless Case Of Leg CRPS Helped by Pulsed Radiofrequency of Sciatic Nerve at Knee | Pain Medical Musing