Review on Bruxism Rx suggests splints, particularly mandibular advancement splints, clonidine or clonazepam, maybe botulinum, and nocturnal clenching biofeedback.
Management of sleep bruxism in adults: a qualitative systematic literature review
DANIELE MANFREDINI et al.
Journal of Oral Rehabilitation 2015 in press
http://onlinelibrary.wiley.com/doi/10.1111/joor.12322/abstract
- 5-10% adult population
- Criteria as mentioned in Int J Prosthodont. 2014 Jan-Feb;27(1):80-6. Suppression of sleep bruxism: effect of electrical stimulation of the masseter
muscle triggered by heart rate elevation. Sumiya M et al:
http://www.ncbi.nlm.nih.gov/pubmed/24392483(1) more than four bruxism episodes per hour(2)more than six bruxism bursts per episode and/or 25 bruxism bursts per hour of sleep,
and(3) at least two episodes with grinding sounds. - modest studies do not allow much in way of conclusions. ie “not enough evidence to define a standard of reference approach for SB [sleep bruxism] treatment except for the use of OA [oral appliance = night splint]
- Some suggestion that a mandibular advancement (MAA) splint might be better “MAA providing a 50–75% advancement significantly decreases the number of SB [sleep bruxism]episodes” – but then some splint dependency
- Diagnosis can be made with a special device you wear overnight called a bitestrip:
http://www.bitestrip.com/
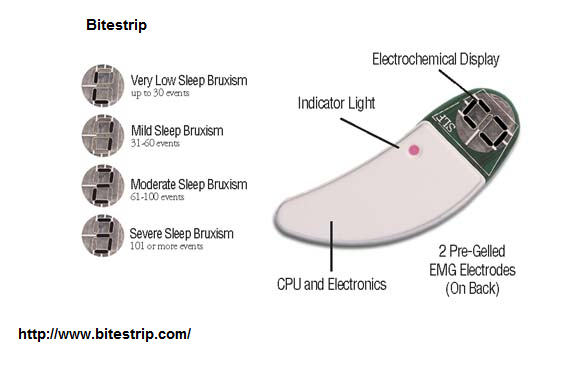
 Validation was acceptable:
Validation was acceptable:
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Sep;104(3):e32-9.
Validation of the BiteStrip screener for sleep bruxism.
Shochat T(1), Gavish A, Arons E, Hadas N, Molotsky A, Lavie P, Oksenberg A.
http://www.ncbi.nlm.nih.gov/pubmed/17618147It costs $45 US plus shipping.
Besides splints, the following treatments might help:
- Stop any antidepressants – I’ve had patients develop headaches at night with teeth clenching and the only way to get rid of headaches was to get rid of the antidepressants gradually…
- treat any sleep apnea – is associated with sleep disordered breathing (early obstruction with snoring)
Sjöholm, T. T., et al.
Sleep bruxism in patients with sleep-disordered breathing.
Archives of oral biology 45.10 (2000): 889-896.
http://www.researchgate.net/profile/John_Fleetham/publication/12347775_Sleep_bruxism_in_patients_with_sleep-disordered_breathing/links/5425ac300cf238c6ea757c7d.pdf
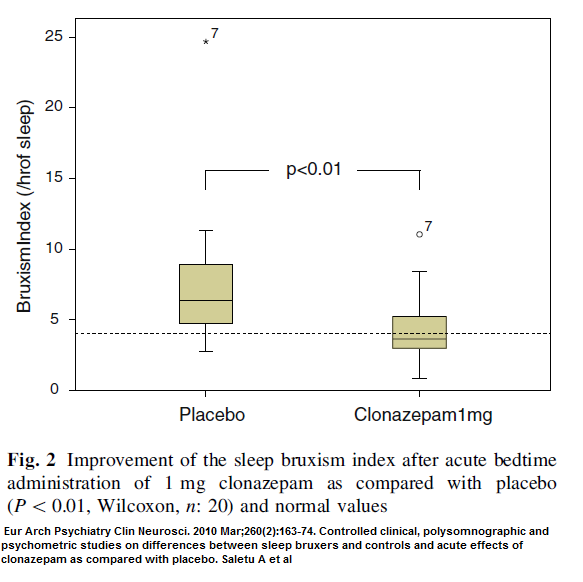
“it appears that sleep bruxism is rarely directly associated with apnoeic events, but is rather related to the disturbed sleep of OSA [obstructive sleep apnea] patients.” - Clonazepam 1 mg at bedtime – commonly used by sleepwalkers and people with restless legs long term with out much difficulty. Drops bruxism rates to normal.
Eur Arch Psychiatry Clin Neurosci. 2010 Mar;260(2):163-74.
doi:10.1007/s00406-009-0034-0.
Controlled clinical, polysomnographic and psychometric studies on differences
between sleep bruxers and controls and acute effects of clonazepam as compared
with placebo.
Saletu A(1), Parapatics S, Anderer P, Matejka M, Saletu B.
http://www.ncbi.nlm.nih.gov/pubmed/19603241
- Clonidine- 0.3 mg by mouth at bedtime – α2-adrenergic agonist – Blood pressure med – I use clonidine for ADHD sufferer to help sleep and ADHD at doses of 0.05 – 0.2 mg; also used for menopausal flushing at 0.05 mg
Carra MC et al. Clonidine has a paradoxical effect on cyclic arousal and sleep bruxism during NREM sleep.
Sleep 2010;33:1711–1716.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2982742/pdf/aasm.33.12.1711.pdf
Huynh N, Lavigne GJ, Lanfranchi PA, Montplaisir JY, de
Chaplain J (2006) The effect of 2 sympatholytic medications—
propranolol and clonidine—on sleep bruxism: experimental randomized
controlled studies. Sleep 29:307–316
http://www.ncbi.nlm.nih.gov/pubmed/16553016
– reduced sleep bruxism index by 61%
-19% were bit hypotensive in am – dizzy getting up - “sleep hygiene measures as well as muscle relation techniques is not effective” – That is unfortunate.
Valiente L et al.
Do sleep hygiene measures and progressive muscle relaxation influence sleep bruxism? Report of a randomised controlled trial.
J Oral Rehabil. 2015;42:259–265
http://www.ncbi.nlm.nih.gov/pubmed/25413839 - wake-time EMG-based biofeedback program aiming to reduce awake bruxism – yes – but no long term data to see if lasted
Sato M, Iizuka T, Watanabe A, Iwase N, Otsuka H, Terada N et al. Electromyogram biofeedback training for daytime clenching and its effect on sleep bruxism.
J Oral Rehabil. 2015;42:83–89.
http://www.ncbi.nlm.nih.gov/pubmed/25256380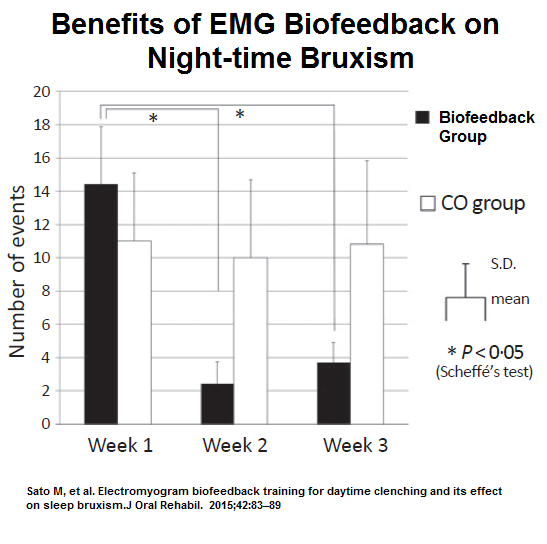
- Hypnotherapy – a case – 7 sessions while dealing with hostility issues – successful
Int J Clin Exp Hypn. 2013;61(2):205-18.
doi: 10.1080/00207144.2013.753832.
Nocturnal bruxism and hypnotherapy: a case study.
Dowd ET
” I tend to follow the model developed by Milton Erickson who advocated utilizing or bypassing resistance (e.g., Erickson & Rossi,1979, 1981), often by speaking to the “unconscious mind” (although that is a metaphor) and using metaphor itself and stories to avoid arousing resistance.” – More in his book on Cognitive Hypnotherapy - Botulinum –
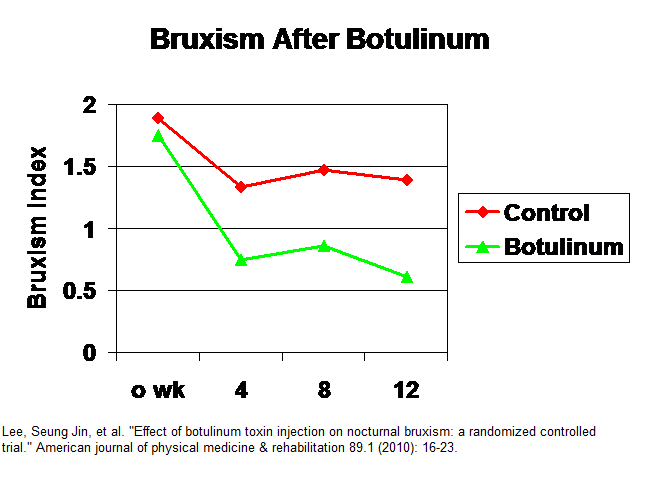
Lee, Seung Jin, et al.
Effect of botulinum toxin injection on nocturnal bruxism: a randomized controlled trial.
American journal of physical medicine & rehabilitation 89.1 (2010): 16-23.
http://www.nobruxismo.it/pdf/Lee%20bruxismo%20notturno%20effetto%20delle%20iniezioni%20di%20botox.pdf
Procedure – 80 mouse units of botulinum toxin A (Dysport, Ipsen,Wrexham, United Kingdom) [=about 27 u Botox] diluted in 0.8 mls saline. Dose split between 3 areas each masseter: “The first site was the inferior, prominent part of the masseter muscle observed when the subject was asked to clench, and the other two sites were 5 mm from the first point anteriorly and posteriorly.”
Saline control done same.
Results: (bruxism rating were not strictly nocturnal)
 In:
In:
Shim, Young Joo, et al.
Effects of botulinum toxin on jaw motor events during sleep in sleep bruxism patients: a polysomnographic evaluation.
Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine 10.3 (2014): 291.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3927435/pdf/jcsm.10.3.291.pdf— These subjects were already on splints so effects could have been blunted by that.
– Technique:BoNT-A (Neuronox, Medytox Inc., Seoul, Korea) [about same strength as Botox] 200 U mixed in 4 mL of sterile saline = 5 U/0.1 mL. A dose of 25 U of “BoNT-A was injected into each muscle using a 1-mL syringe with a 29-gauge, 0.5-inch needle.BoNT-A was injected into 3 sites of each subject’s masseter and/
or temporalis muscles depending on the experimental group. The BoNT-A injection sites are shown in Figure. In the masseter muscle, the first site was the inferior, prominent partof the masseter muscle that was observed when the subject was asked to clench, and the other 2 sites formed a triangle 10 mm
away from the first site (Figure 1A). In the temporalis muscle, the first site was the prominent part of the anterior temporalis muscle that was observed when the subject was asked to clench, which was parallel to eyebrow. The other 2 sites were 10 mm, 20 mm away from the first site posteriorly.”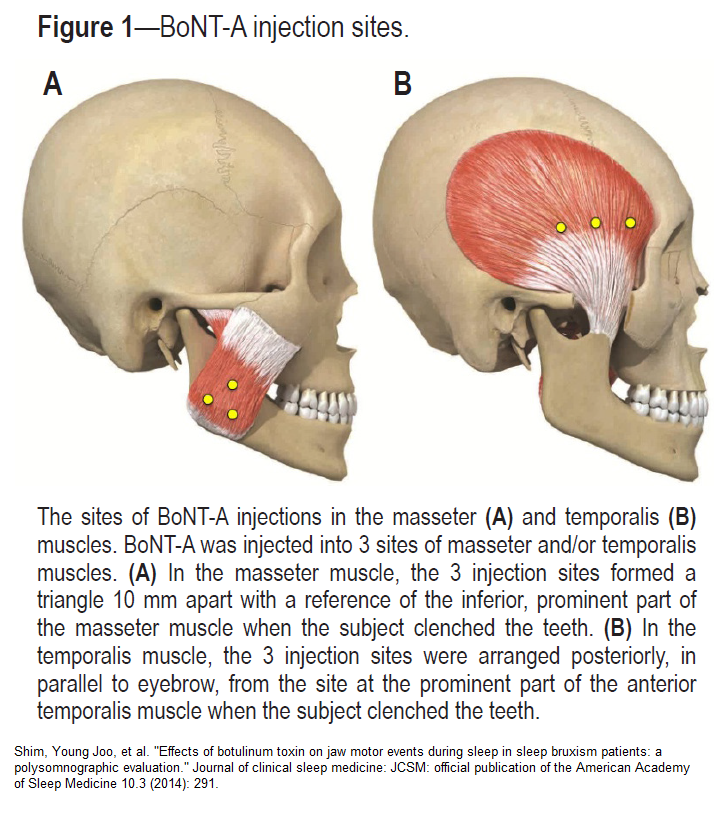
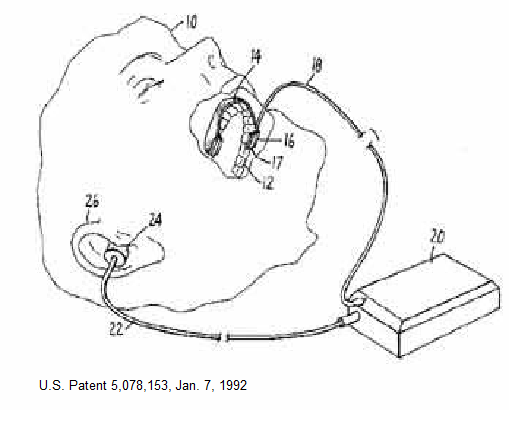
– Did not effect amount of bruxism as much as the strength of muscle contractions. This helped with perceived TMJ muscle fatigue in AM. However thye felt “an effective strategy for controlling SB [sleep bruxism] for at least a month” - Sound Alarms- pressure sensor put onto splints
– unfortunately after 2 weeks one gets used to alarm and it no longer helps
- Heart rate biofeedback
Int J Prosthodont. 2014 Jan-Feb;27(1):80-6. doi: 10.11607/ijp.3330.
Suppression of sleep bruxism: effect of electrical stimulation of the masseter
muscle triggered by heart rate elevation.
Sumiya M, Mizumori T, Kobayashi Y, Inano S, Yatani H.
http://www.ncbi.nlm.nih.gov/pubmed/24392483
-Works on principle that when heart rate elevates, bruxism occurs:
 – Brilliant approach where face muscle stimulated when nocturnal heart rate elevates
– Brilliant approach where face muscle stimulated when nocturnal heart rate elevates
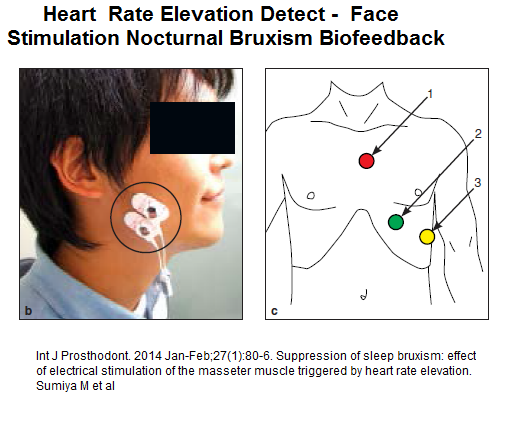 – cut bruxism up to 45% but like above biofeedback device not sure if it persisted.
– cut bruxism up to 45% but like above biofeedback device not sure if it persisted. - Cognitive behavioural with biofeedback
Ommerborn, M. A., et al.
Effects of an occlusal splint compared with cognitive-behavioral treatment on sleep bruxism activity.
European journal of oral sciences 115.1 (2007): 7.
http://www.ncbi.nlm.nih.gov/pubmed/17305711
-effects were not sustained
Comment –
- Clonidine, being an alpha blocker, would be good for men with prostatism and for women with menopausal flushing. ((NNT = 3.2 apparently)
- splints, particularly with mandibular advancement, would be ideal in subjects with TMJ and displaced menicus.
- Looking into sleep apnea and of course stopping particularly SSRI antidepressants important. Still happens with moclobemide though.
- Clonazepam would be perfect for those with restless legs
- EMG particularly biofeedback helpful.
- Botulinum injections could help some
- Wish I new more about the nocturnal biofeedback
- Need more info re hypnosis
Any suggestions or successes out there?

I have found that cutting Prozac and adding clonazepam at night has greatly improved
My nighttime AND daytime clenching greatly! TMJ is still an issue however. But the pain associated has gone down.
Thank you for the wonderful advice Dr.M :)
Hope this helps others as well!
Christina
Hi,I read your blog named “Bruxism – How do You Treat 2015 Besides Splints | Pain Medical Musing” regularly.Your story-telling style is witty, keep it up! And you can look our website about love spells.