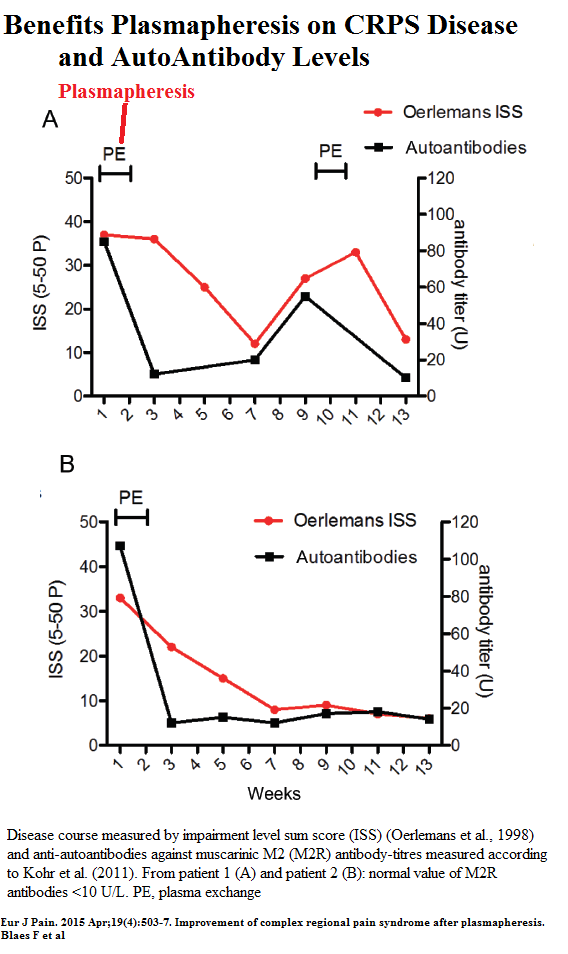
Finding high levels of beta2 adrenergic receptor autoantibodies in CRPS cases might explain why steroids, tumour necrosis factor (TNF)-alpha antagonist
Adalimumab, IV Immmunoglobulins, and in present article Plasmapheresis can help in selected cases. In present study, these antibody titres fell with treatment at same time as pain levels fell.
Eur J Pain. 2015 Apr;19(4):503-7. doi: 10.1002/ejp.572
Improvement of complex regional pain syndrome after plasmapheresis.
Blaes F(1), Dharmalingam B, Tschernatsch M, Feustel A, Fritz T, Kohr D, Singh P, Kaps M, Szalay G.
http://www.ncbi.nlm.nih.gov/pubmed/25115658
- 2 cases – on after fall on arm, second post carpal tunnel surgery
- Failure steroids, Physiotherapy, NSAIDs, gabapentin, and opioids.
- “five consecutive sympathetic blockades over 3 weeks” in one case
- Plasmapheresis was “four times on an alternate day protocol”.
 Mechanisms of CRPS were summarized as
Mechanisms of CRPS were summarized as
- neurogenic inflammation – backward spilling of irritating neurotranmitters (Substance P and CGRP) by afferent neurons ;
- a disturbance of the sympathetic nervous system including reduction
of small-diameter axons in the affected area - profound cortical reorganization
- Immunogenic – autoantibodies directed against surface sites on autonomic neurons [NEW]- β2 receptor autoantibodies and cytokine effects.
Comments
- Exciting new additions to treating a horrible disease.
- The ” β2 adrenergic receptor autoantibodies” tests was one they developed in 2009 and I am not sure how available it is. Phasmapheresis is expensive and I doubt I could convince an hematologist to spring for it unless obviously a desperate case or could demonstrate these anitbodies – anyone know if available?
I know it is easy to offer suggestions in hindsight but could use comments on whether they would be helpful:
Ketamine
- My first experience with ketamine was after I saw the poster:
KETAMINE FOR REFRACTORY CRPS: A CASE SERIES REPORT
written here:
Simplest Ketamine Technique Ever for CRPS – Low Dose 10 mg Ketamine Subcut Weekly
http://painmuse.org/?p=695
They used 10 mg subcut weekly as described a 50% reduction in CRPS pain. I then got more excited about its use after a IV- like – repeated Q15 min deltoid IM x technique for neuropathic pain was published:
INTRAMUSCULAR (IM) KETAMINE FOR TREATING MIGRAINE
AND NEUROPATHIC PAIN IN THE CLINIC
http://www.anodyneheadachepain.com/Research/APS4.pdf - I settled on 10 mg Ketamine Q15 min in Deltoid x 2 -well tolerated but I cannot claim to get any lasting results in my patients – but it give some relief for 3 days – at which time they come back to office for another shot. It has remarkable effects on mood that again only lasts a few days. Never any interstitial cystitis at that dose and frequency. I suspect it would trim down severe pains over time.
Continuous blocks
- Most benefits from regional therapies in my mind, take 3-7 days – example is a 5 day paraspinous continuous blocks for post mastectomy pains:
Possible Curative Treatment For Post Mastectomy Pain
http://painmuse.org/?p=570 - Axillary blocks can be relatively easy – I just inject on either side of brachial artery in axilla. There are “golden cases” that respond to one shot -so try it in axilla.
Fallatah, S. M. (2014).
Successful management of complex regional pain syndrome type 1 using single injection interscalene brachial plexus block.
Saudi journal of anaesthesia, 8(4), 559. - Most studies did catheters.
one of first mentions was a case study:
Wang, Li-Kai, Han-Ping Chen, Pei-Jung Chang, Fu-Chi Kang, and Yu-Chuan Tsai.
Axillary brachial plexus block with patient controlled analgesia for complex regional pain syndrome type I: a case report.
Regional anesthesia and pain medicine 26, no. 1 (2001): 68-71.
http://journals.lww.com/rapm/Abstract/2001/01000/Axillary_Brachial_Plexus_Block_With_Patient.15.aspx - This was followed by a series:
Margić, K., & Pirc, J.
The treatment of complex regional pain syndrome (CRPS) involving upper extremity with continuous sensory analgesia.
European Journal of Pain, 7(1), 43-47 (2003)
http://www.ncbi.nlm.nih.gov/pubmed/12527316“Brachial plexus block was established with a bolus of 15 ml of 0.25% bupivacaine, and then, depending on the degree of motor blockade, the concentration and volume of the anesthetic were reduced. A continuous analgesia was provided by intermittent injections of 10–15 ml of 0.25–0.125% bupivacaine every 6 h. The aim was to achieve good sensory analgesia without motor blockade. ”
-infusion for 7 days though catheter remained for 10 days in case needed.Among their 16 uncomplicated cases ( complex = fractures , post trauma OA and nerve damaged) they all uniformly had either satisfactory of excellent results. Why is that not used more???
One example of a block was this poster abstract that found continuous Infraclavicular block better than axillary:
Continuous block of the brachial plexus through infraclavicular approach in CRPS type II of the upper extremity
The Journal of Pain, Volume 9, Issue 4, Supplement 2, April 2008, Page 26
M. Maroof, O. Ahmed, H. Usmani, R. Khan, M. Ahmed, S. Maroof
(201)
Chronic regional pain syndrome is a complex neurological disease that often follows trauma or surgery. There are various treatment modalities for this disorder. Continuous infraclavicular brachial plexus block along with catheter placement is a technique that can produce dramatic relief in patients suffering from chronic regional pain syndrome (CRPS). A 30 years old male patient presented in the pain clinic of the Department of Anaesthesiology, with the complaints of pain in the left upper limb following a gunshot injury 2 months back. Pain was very severe, burning and continuous in nature with a score of 1 on a rupee scale (0 – no pain, 1–maximum pain)and used to get aggravated on movement,superficial touch and was not relieved by pain killers . Initially the pain was local- ized to the left arm but gradually it involved whole of the left upper limb. His left upper limb was cold, livid, swollen, range of motion was severely impaired and trophic changes of skin were clearly visible. As a treatment modality , initially a stelliate ganglion block was given, twice on alternate days using 10 ml of 0.25% bupivacaine. The patient re- ported reduction in the intensity and severity of pain and after 3 days the patient was given a continuous infraclavicular brachial plexus block using 0.25% bupivacaine at the rate of 5 ml/ hr and was advised a combination of oral tramadol and paracetamol on SOS basis ,with the advice that the dose should not exceed more than 4 tab / 24 hrs. The patient was reviewed after four weeks in the pain clinic, there was a marked reduction in the intensity of pain with a VAS score of 4/10 scale
- Nowadays, disposable catheter/pumps are used after shoulder surgery to deal with outpatient done surgery.
 So one of these disposable pumps with nerve catheter could theoretically be left in 3 days then replaced with a new one. I asked an anesthetist about chances of inpatient continuous and was told “not going to happen” but that was some years ago. The exception seems to be children and there are reports using it there.
So one of these disposable pumps with nerve catheter could theoretically be left in 3 days then replaced with a new one. I asked an anesthetist about chances of inpatient continuous and was told “not going to happen” but that was some years ago. The exception seems to be children and there are reports using it there.
Tolba, R., Badr, R., Guirguis, M., & Soliman, L. M. (2015).
Pediatric Continuous Brachial Plexus Catheter for a Case of Complex Regional Pain Syndrome (CRPS).
Open Journal of Anesthesiology, 5(01), 1.
http://www.scirp.org/journal/PaperDownload.aspx?paperID=53071
Point is made that nerve blocks are considerably safer than sympathetic blocks though they were talking about catheter infusionsTolba, R., Badr, R., Guirguis, M., & Soliman, L. M. (2015).
Pediatric Continuous Brachial Plexus Catheter for a Case of Complex Regional Pain Syndrome (CRPS).
Open Journal of Anesthesiology, 5(01), 1.
http://www.scirp.org/journal/PaperDownload.aspx?paperID=53071
“catheter infusion of local anesthetic is a valuable method of reducing
pain in severe cases of upper extremity pediatric CRPS and may be safer and more effective than other invasive measures, such as sympathetic blocks and epidural catheterization.“
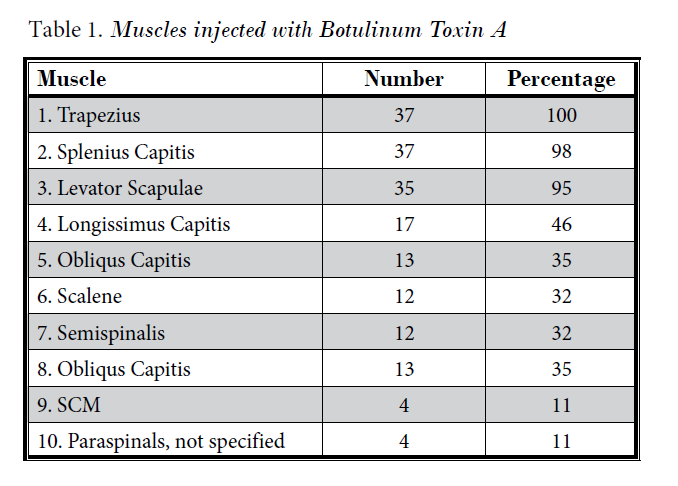
Botulinum
- Injecting Botox into muscles of affected CRPS areas resulted 43% decrease in pain at 4 weeks. Issue is that Botox wears off after 10 weeks and shot would need to be repeated. Hopefully the botox would loosen up the muscles enough so they could be kept stretched out though.
Kharkar, S., Ambady, P., Yedatore, V., & Schwartzman, R. J. (2011). Intramuscular botulinum toxin A (BtxA) in complex regional pain syndrome. Pain physician, 14, 311-316.
http://thblack.com/links/RSD/PainPhys2011_14_419_IM-BotulismToxin4Dystonia.pdf
“Based on the size of the muscle, 10-20 units of BtxA were then injected through the needle. This procedure was repeated for all muscles injected. The total mount of BtxA used per participant was 100 units”
- Injecting Botox intradermally over allodynic areas failed to be helpful:To Bad..
Safarpour, D., Salardini, A., Richardson, D., & Jabbari, B. (2010). Botulinum toxin A for treatment of allodynia of complex regional pain syndrome: a pilot study. Pain Medicine, 11(9), 1411-1414.
http://www.ncbi.nlm.nih.gov/pubmed/20609130
An excellent review of treatment options comes from a recent article written by a Toronto doctor who went thru CRPS. One regret seemed to be not taking sympathetic blocks earlier. One of the successes was ketamine given at bedtime orally – something I has not gotten into. the king of options is to get IV prolonged IV ketamine treatments available through ? Dr. Robert J. Schwartzman
https://www.drexelmed.edu/Home/AboutOurFaculty/RobertSchwartzman.aspx
Drexel Neurology
219 N. Broad Street
The Arnold T. Berman, MD Building, 7th Floor
Philadelphia, PA 19107
Phone: 215-762-6915
Fax: 215-762-6914
but suggested IV treatments in US could amount to $30,000.00
Binkley, K. E. (2013).
Improving the diagnosis and treatment of CRPS: insights from a clinical immunologist’s personal experience with an underrecognized neuroinflammatory disorder. Journal of Neuroimmune Pharmacology, 8(3), 477-488. 2013
http://www.thblack.com/links/RSD/JNeuroimmunePharmacol2013_8_477_PersonalExperOfMDw-CRPS.pdf
Controversial new treatment option include
Bone Marrow
Aspirate Stem Cell Harvesting from the posterior Iliac Crest (uses same equipment as used for Platelet Rich Plasma after harvest)
injected into most affected area seemed beneficial:
Schwartz, R. G. (2015). Stem Cells For The Treatment of Complex Regional Pain Syndrome (CRPS)/Reflex Sympathetic Dystrophy (RSD): a case study.
Pan American Journal of Medical Thermology, 1(2), 89-92.2015
http://www.abraterm.com.br/revista/index.php/PAJTM/article/download/17/pdf_12
Immunoglobulin infusion has been found helpful in selected cases and attempts to revert to a simple subcut program resulted in this poster in Journal of Pain 2010
Managing pain in CRPS: a case series examining the effects of repeated dose subcutaneous immunoglobulin
H Poole, B Frank, K Maciver, L Haynes, L Wyatt, S Misba, J Burton, and A Goebel; The Walton Centre NHS Foundation Trust, Liverpool, Merseyside, United Kingdom
Pain is one of the primary features of CRPS. The optimal treatment regime is not yet established for CRPS and many patients have no effective method of relieving ongoing pain. Single low dose (0.5g/kg) intravenous immunoglobulin (IVIG) has been shown to be effective in some patients. 1 We aimed to investigate the effects of repeated home administration of immunoglobulin (SCIG) on pain, QoL and function. Three patients (2 female) who responded to single-dose IVIG 4-5 years ago 1 participated in a prospective open case series. Duration of CRPS ranged from5-6 years. Pain intensity (0-10NRS) during screening was between 6 and 7. Initially, each received a single dose of IVIG (1g/kg in patient 1 and 0.5g/kg in patients 2 & 3). Patient 2 did not achieve >45% pain reduction following IVIG and was discharged as per protocol. Patients 1 & 3 experienced >45% pain reduction and continued in the study, self administering SCIG weekly at home. The initial SCIG dose for patient 1 was 1g/kg/month, reduced to 0.5g/kg/month at 6 months and to 0.25g/kg/month at 9 months un- til 12 months. Patient 3 administered 0.5g/kg/month for 3.5 months. Both re- corded pain and sleep daily and QoL and functioning monthly. Clinical and psychosocial assessments were conducted bi-monthly. Patients 1 & 3 reported sustained and stable pain reduction of >70% over their study periods. QoL and daily functioning improved (0.4 & .35 Quali gain on the EQ5D, and reductions on the Brief Pain Inventory reductions 7.7 and 6.1 at baseline to 1.4 and 0 at 12/3.5 months respectively). In two patients, SCIG treatment dramatically reduced symptoms of longstanding CRPS, improved QoL and function, without apparent development of tolerance. Low-dose SCIG home-application may be viable option for current IVIG responders.The lowest effective dose has yet to be established. (1. Goebel et al., Ann Int Med, 2010.)
Pulse radiofrequency has been tried to dorasl root ganglion in case of post polio with success:
Apiliogullari, Seza, et al.
“Pulsed Radiofrequency of Dorsal Root Ganglia for the Treatment of Complex Regional Pain Syndrome in an Adolescent with Poliomyelitis Sequel: A Case Report.”
Pain Medicine (2015).
http://onlinelibrary.wiley.com/doi/10.1111/pme.12710/abstract?deniedAccessCustomisedMessage=&userIsAuthenticated=false
Comment – once established, CRPS is horrible to treat and requires multidisciplinary approaches. The best way is to prevent it.
1) Case 1 – elderly lady with hairline fracture 2 metatarsals Right foot. Pain escalated over 2 days. Started on prednisone, and within 24 hours pain melted away. Got on Vitamin C – recovered
2) Lady in 20’s with suspected scaphoid fracture. Despite cast not being too tight, complaints of excessive arm and medial hand pain. Injected local on either side axillary artery and pain melted away. Hasn’t returned so suspect got better. – started on Vitamin C 500 mg twice daily
Spinal stimulation is also a measure for CRPS. One of the early users was Dr. Kumar in Regina. He maintained that he got best results when implanted early (<6 month I think). Talked to another neurosurgeon speaker about that and he did not know that – probably because he doesn’t see many that early. Thought is, that it maybe should be a first resort, not a last one

I have had 10 back surgeries to rebuild levels L2-S1 that were degenerative. I have cage and PEEK implants, and resulting severe CRPS down my left side, leg, foot, and have gotten no relief from the all usual neurallytic oral meds, injections, blocks, accupuncture/dry needling, physical therapies. I have called Dr. Schwartzman’s office and his associates to try to get an appointment, but cannot get past the receptionist who is rude and says no new patients call back. I would appreciate even a recommendation of another practice for treatment of this terrible condition – not just a slammed door. Please help me.
——————
I’m so sorry.
Maybe see if you can enroll in the IV Neridronate trial:
https://clinicaltrials.gov/ct2/show/NCT02402530?term=Neridronate&rank=3
You need decent teeth for that – if you have a poor dental condition, you are more prone to osteonecrosis of your jaw, so they won’t take you