Recent findings that mast cells may trigger migraines has significant implications on cause and treatment. Mast cells play a key role in Peripheral Sensitization – Neurogenic Inflammation where tissues become overly tender and swollen. They are, however, a cornerstone of allergies as well; which complicates their role and complicates therapy.
Two recent articles:
Pain. 2007 Jul;130(1-2):166-76 Levy D et al.
Mast cell degranulation activates a pain pathway underlying migraine headache.
abstract here article here
J Pharmacol Exp Ther. 2007 Aug;322(2):806-12; Zhang XC et al.
Sensitization and activation of intracranial meningeal nociceptors by mast cell mediators.
abstract here article here
Hence mast cells might:
- trigger the migraine
- Induce the peripheral sensitization/neurogenic imflammation – this is when the skin becomes overly tender. Tryptans like Imetrix fail to work when the outside tissues have reached this state so it has been advised that if people use tryptans they must use them before the tissues become too sore. (What happens is the headache will no longer pound but it will still hurt if taken too late).
There is also evidence mast cells effect the renin-angiotensin system which is thought to potentiate the migraines.
Mast Cells Activate the Renin Angiotensin System and Contribute to Migraine: A Hypothesis
Hisham Ba’albaki, MD; Alan Rapoport, MD; Headache advance online
Migraine is a chronic disease with episodic attacks, which, when frequent or severe, can be associated with poor quality of life, increased health resource utilization, lost productivity, and significant disability. Preventive therapy can therefore have a significant beneficial clinical and economic impact. However, many migraineurs are treated suboptimally. There is increasing evidence that activation and degranulation of meningeal mast cells result in meningeal irritation, vascular dilation, and stimulation of nearby nociceptive nerve endings of the trigeminal nerve, thus potentially contributing to the pathogenesis of migraine headache. The renin angiotensin system and its peptides are well represented in the mammalian central nervous system and can also promote neurogenic inflammation. Interestingly, mast cells are capable of releasing renin and increasing local production of Angiotensin II. We therefore hypothesize that mast cells contribute to migraine headache through activation of the renin angiotensin system. This hypothesis may help explain the association between migraine and cardiovascular disease as well as observations that medications that modulate the renin angiotensin system can reduce migraine-related morbidity in patients with frequently recurring migraine attacks.
A review of its association here:
J Hypertens Suppl. 2006 Mar;24(1):S139-43. Involvement of the renin-angiotensin system in migraine. Tronvik E, Stovner LJ, Schrader H, Bovim G. abstract here
A “competitor” activator – Calcitonin gene-related peptide (CGRP) has not been shown to do that.
Ann Neurol. 2005 Nov;58(5):698-705. Calcitonin gene-related peptide does not excite or sensitize meningeal nociceptors: implications for the pathophysiology of migraine. Levy D, Burstein
Prostaglandin system appears involved as Parenteral Naproxen or Ketorolac appears to reduce neurogenic imflammation changes directly in the Brain center in the trigeminal dorsal horn
Neuroscience. 2007 Aug 24;148(2):573-83. Epub 2007 Jul 25. Sensitization of central trigeminovascular neurons: Blockade by intravenous naproxen infusion. Jakubowski M, Levy D, Kainz V, Zhang XC, Kosaras B, Burstein R. abstract here
Comments and Implications:
1) Identifying the “allodynic” = skin becomes sensitized group is important:
Improved identification of allodynic migraine patients using a questionnaire
A Ashkenazi et al;Cephalalgia, 2007, 27, 325–329
They found 8 questions –
Do you experience pain or unpleasant sensation on your skin during a migraine attack when you engage in any of the following activities:
- “Ponytailing”
- Wearing Tight cloths anywhere
- Combing
- Resting headache side on Pillow
- Heat (cooking or heating pads) or Cold (cold day or cold pads)
- Wearing glasses.
- Tight head/neck gear. (hat or scarf)
If two or more symptoms, 97% in the allodynic catagory.
If allodynic, then Tryptan use must be early in an attack, and use of an NSAID during an attack(if tolerated) would be useful. I would say, deactivating muscle triggers would be important as well; there is a recent study showing significant benefits there.
The Journal of Pain, Vol 8, No 11 (November), 2007: pp 869-878
Contribution of Myofascial Trigger Points to Migraine Symptoms
Maria Adele Giamberardino et al
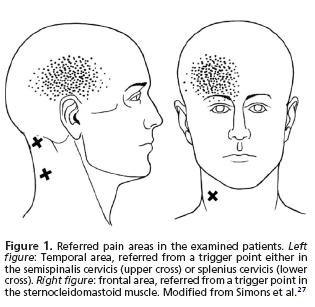
In:
- sternocleidomastoid
- semispinalis cervicis
- splenius cervicis
“TrP infiltration with local anaesthetic [0.5 mL of bupivacaine (5 mg/mL)]. The infiltration was repeated on the 3rd, 10th, 30th, and 60th day after the initial evaluation.” Our College frowns on use of local in the neck; saline may be equally effective. Compared to a sham injection group (needle inserted and removed) there was about 50% reduction in migraine headaches by day 60.
2) Blocking the renin-angiotensin system is helpful in migraines.
Ba’albaki et al state: “More recently, the angiotensin converting enzyme (ACE) inhibitor lisinopril 20 mg/day and the angiotensin receptor blocker (ARB) candesartan 16 mg/day have demonstrated some effectiveness in the prevention of migraine”.
I have used lisinopril mostly in hypertensives with migraines and found it very effective (1/2 by reducing BP and 1/2 by R-A inhibition I think).
3) Deal with the mast cells with drugs. Unfortunately, leukotreine inhibitors(Singulair) by themselves don’t do well.
Montelukast for migraine prophylaxis: a randomized, double-blind, placebo-controlled study.
Headache. 2004 Jun;44(6):581-6.
Brandes JL, Visser WH, Farmer MV, Schuhl AL, Malbecq W, Vrijens F, Lines CR, Reines SA
The association on migraines to histamine, however, was noted years ago and a patent even filed. He used Hydroxyzine 50 mg. in a few cases of patients with prolonged aura and demonstrated its ability to block subsequent migraine. The problem here is that hydroxyzine has tranquilizer properties which in themselves might have reduced stress, a factor in migraine – so is its effect really mast cell related? patent here article here
4) Deal with mast cells re allergies. What may be forgotten is that the mast cell is the allergy cell as well as orchestrating peripheral neurogenic inflammation.
Several good studies were done near the early 1980’s in Lancet:
Lancet. 1979 May 5;1(8123):966-9.
Food allergies and migraine.
Grant EC.
60 migraine patients completed elimination diets after a 5-day period of withdrawal from their normal diet. 52 (87%) of these patients had been using oral contraceptive steroids, tobacco, and/or ergotamine for an average of 3 years, 22 years, and 7.4 years respectively. The commonest foods causing reactions were wheat (78%), orange (65%), eggs (45%), tea and coffee (40% each), chocolate and milk (37%) each), beef (35%), and corn, cane sugar, and yeast (33% each). When an average of ten common foods were avoided there was a dramatic fall in the number of headaches per month, 85% of patients becoming headache-free. The 25% of patients with hypertension became normotensive. Chemicals in the home environment can make this testing difficult for outpatients. Both immunological and non-immunological mechanisms may play a part in the pathogenesis of migraine caused by food intolerance.
What is not mentioned in the abstract, but discussed in the article was that just avoiding these foods without elimination diet testing was limited in value. It was likely to result in over-exposure to some lesser-involved food – for instance rice had a 15% reaction rate. It was also found that those who were currently abusing painkillers or ergot, or still on OCP’s composed the 15% who did not respond. Subsequent articles were often based on
- allergy tests – many reactions are not clearly RAST or skin allergy test positive
- patient’s observations of reactions – are poor at best: One of the key features of a reaction is the mental fog it creates which prevents much recollection of what hit them. Some headache reactions are delayed and hence missed as well. Food reactions only occur in the setting of someone already tired and stressed; so a clear picture will never be evident without elimination diet testing. I do suggest people keep a diary but that does not seem to get done.
- one time exposure – headache is not going to happen unless tired and stressed too. It is the old example of the ship in the ocean – you need several rocks in the boat to sink – stress, sleep loss and then food reaction.
- tertiary center studies – these cases are severe – there will be so much rebound and other complicating factors that will prevent any association with food. I have treated some of these cases and it’s only after treating neck, TMJ, sleep issues, back pains, and comorbid depression that I finally consider looking for foods. Doing this ahead of time is not particularly valuable because of the ceiling effect – the other factors make patient hit ceiling so food etc. factors aren’t apparent.
Well, so where are you going to get easy access to foods as causes of migraines? – well, look at kids:
Lancet. 1983 Oct 15;2(8355):865-9. Is migraine food allergy? A double-blind controlled trial of oligoantigenic diet treatment.
Egger J, Carter CM, Wilson J, Turner MW, Soothill JF.
93% of 88 children with severe frequent migraine recovered on oligoantigenic diets; the causative foods were identified by sequential reintroduction, and the role of the foods provoking migraine was established by a double-blind controlled trial in 40 of the children. Most patients responded to several foods. Many foods were involved, suggesting an allergic rather than an idiosyncratic (metabolic) pathogenesis. Associated symptoms which improved in addition to headache included abdominal pain, behaviour disorder, fits, asthma, and eczema. In most of the patients in whom migraine was provoked by non-specific factors, such as blows to the head, exercise, and flashing lights, this provocation no longer occurred while they were on the diet.
This was an excellent study – I cannot believe the skill they had in putting these kids on a restricted diet and double blind testing their reaction with powders in soup – repeatedly comfirmed reactions. Their findings suggest nearly ALL children have food as the primary concern.
IN
The Diet Factor in Pediatric and Adolescent Migraine
J. Gordon Millichap, MD, and Michelle M. Yee, CPNP
Pediatr Neurol 2003;28:9-15
They write:
“In one large-scale double-blind trial of an elimination diet involving 88 patients treated with an oligoantigenic diet, a diet that eliminates all but a few sensitizing food antigens, 93% with severe frequent migraine responded and were free of headaches [24,25]. The diet consisted of lamb or chicken, rice or potato, banana or apple, Brassica, water, and vitamin supplements.
Of the 82 patients who improved on the diet, all but eight patients relapsed on the reintroduction of one or
more foods. A remarkable fondness for migraine-provoking foods was a common finding, some patients craving them and eating them in large amounts. Cow’s milk and cheese caused headaches in most of the patients in the study, but none of the patients complained of headaches after substituting goat’s milk cheese.
Notwithstanding the impressive response demonstrated in this double-blind investigation, in practice the relationship between food allergy or intolerance and migraine is difficult to prove, because the elimination diet is too demanding and skin tests and antibody titers demonstrate inconsistent results. The concept remains controversial, and many neurologists and allergists are skeptical of the use of restrictive diets in treatment.”
My Interpreation – These Doctors are too lazy to look for food triggers in children and so pretend they don’t exist. I once heard a pediatric neurologist talk on childhood migraines with barely a mention of foods. There was much discussion of other potential treatments. I mentioned something to the effect that 93% of the talk should have been more food related but it was obvious the doctor was not familiar with elimination diets. A very good reference here is an old book “Tracking Down Hidden Food Allergy” by Dr. W. Crook still available at Amazon
here
Otherwise, the treatments for children have been mentioned here:
Expert Opinion on Pharmacotherapy April 2007, Vol. 8, No. 6, Pages 731-744
Recommendations for the management of migraine in paediatric patients
Umberto Balottin1 & Cristiano Termine
They state:
“Ibuprofen (7.5 – 10.0 mg/kg) and acetaminophen (15 mg/kg) are safe and effective, and should be considered for symptomatic treatment. Sumatriptan nasal spray (5 and 20 mg) is also likely to be effective, but at the moment, should be considered for the treatment of adolescents only. With reference to prophylactic drug treatment, the available data suggest that flunarizine (5 mg/day) is likely to be effective and pizotifen and clonidine are likely to be ineffective.”
5) Deal with mast cells through relaxation training.
Stress has been demonstrate to induce mast cell degranulation and this is thought to be through stress activated Corticotrophin-releasing Hormone:
Pang X, Alexacos N, Letourneau R, et al. A neurotensin receptor antagonist inhibits acute immobilization
stress-induced cardiac mast cell degranulation, a corticotropin-releasing hormone-dependent process.
J Pharmacol Exp Ther. 1998;287:307-314.
The most interesting offshot of this effect was mast cell degranulation can be ameliorated by relaxation training:
Headache: The Journal of Head and Face Pain Volume 39 Issue 2 Page 101-107, February 1999
Mast Cell Activation in Children With Migraine Before and After Training in Self-regulation
Karen Olness et al. abstract here
So what is available to use here:
– Biofeedback – Not really available here though cheap biofeedback GSR old radioshack monitors can be gotten off ebay
– Hypnosis – I have two psychiatrists tell me in no uncertain terms that one should never do hypnosis in children even with a parent present because it could come back to bite you. There is a Dr. Bromley in my clinic who, though semi-retired, still does hypnosis and I am grateful for his help.
– Hypnosis tapes there was a recent article on its use described here:
Self-Hypnosis Training for Headaches in Children and Adolescents
KOHEN, DANIEL P. MD; ZAJAC, ROBERT MD
The Journal of Pediatrics Volume 150(6), June 2007, p 635–639
Induction was just imagining a favorite place.
Deepening was through making the favorite place a multisensory experience and through progressive muscular relaxation. (tell them to relax each area in turn)
Headache counteraction was thru several rechniques:
- Going to a place where never had headaches
- Watch the severity number on a ruler change or watch it in an elevator which is better because you can push a down button.
- “Imagine your HA is a certain shape and color and in another part of your mind is the color and shape of happy and comfortable … and you can watch the HA shape and color in your mind get smaller and smaller and smaller while the happy and comfort shape get bigger and bigger until it fills the screen in your imagination.”
- whatever works – I like warm hands on abdomen warming the tummy etc.
“The average frequency of HA decreased from 4.5 per week to 1.4 per week (P < .01).”
– What is left? At the Canadian Pain Society this year was mentioning of a study using yoga for adolescent Irritable bowel (another mast cell disease) with success.
I would be interested in comments on treating headaches and perhaps its relation to mast cell issues.

Your view on Mast Cells Implicated in Migraines is fabulous info for any visitor to be thankful for. My hats off for such remarkable information!
I found your blog via Google while searching for migraine headache treatment and your post regarding Mast Cells Implicated in Migraines looks very interesting to me. I am very impressed with your site. The quality of the design and content makes it a real winner! Thanks again for a great site and a great resource on the net.
Mast Cells Implicated in Migraines can be exceptional matter of the moment that you voice on fabulously; thank you much!
So glad I found this truly great site
Pingback: Pain Medical Musing » Blog Archive » Multiple Allergies, Hives and Abdominal Pain - Think Mastocytosis