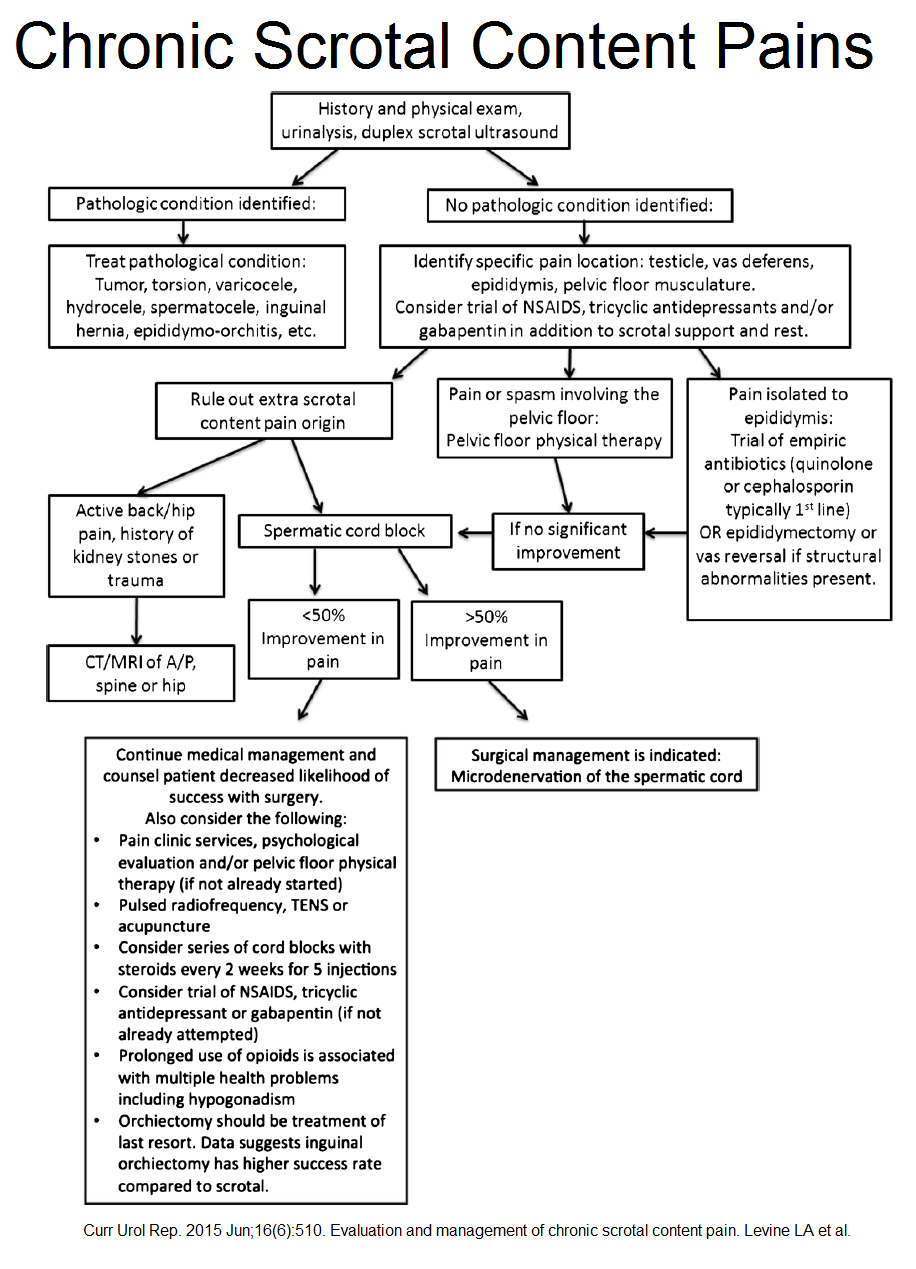
Chronic scrotal pain can be an enigma – this new article gives detailed options for investigation and treatment. I have spent a great deal of time trying to give a clear view for people – let me know if you find it helpful…
Curr Urol Rep. 2015 Jun;16(6):510. doi: 10.1007/s11934-015-0510-1.
Evaluation and management of chronic scrotal content pain.
Levine LA(1), Hoeh MP
http://www.ncbi.nlm.nih.gov/pubmed/25903802
Plans go as follows:
- Classical case mid-late 30’s who has seen 4.5 urologists
- 1/2 no cause
- “The pain can be unilateral or bilateral, constant or intermittent, and spontaneous or exacerbated by physical activities and pressure. It can remain localized in the scrotum or radiate to the groin, lower abdomen, perineum, or back of the legs.”
- Orchiectomy ” significantly decrease pain in 40–75 %”
- Nerve origins from “genital branch of the genitofemoral nerve and the ilioinguinal nerve; autonomic branches from the parasympathetic ganglia of T10–L1 for the epididymis and vas deferens”
- hydrocele, spermatocele, or varicocele removal helps 75-90% of time
- Markedly high Wallerian degeneration of spermatic cord nerve fibers
- Referred DD includes ureteral stones, inguinal hernia, pelvic floor spasm/myalgia , intervertebral disk , rare retroperitoneal tumor, polyarteritis nodosa, aortic aneurysm
- Post vasectomy would include sperm granulomas
- study of mild orchitis of 6 week duration all responded to antibiotics -this has been my experience – where Levaquin has been effective. They tried cephalosporin or quinolone first- if no improvement in 1 week – try doxycycline and azithromycin; I also think Clavulin might be an option.
Lai Y, Yu Z, Shi B, Ni L, Liu Y, Yang S. Chronic scrotal pain caused by mild epididymitis: report of a series of 44 cases. Pak J Med Sci. 2014;30(3):638–41
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4048522/pdf/pjms-30-638.pdf - chronic prostatitis/chronic pelvic pain syndrome with pelvic floor spasms may have constipation, pain with defecation, urinary frequency or dysuria, painful ejaculation, or pain with intercourse – and 1/2 have orchitis pains. Painful muscle bands exist.
- diagnostic spermatic cord block- 20 mL of 0.25 % plain bupivacaine into the spermatic cord at the pubic tubercle level – may need repeating even with just saline to confirm
Re chronic prostatitis:
- They make mention of a study using Quercetin 500 mg bid for chronic prostatis pains:
Shoskes, D. A., Zeitlin, S. I., Shahed, A., & Rajfer, J. (1999).
Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial. Urology, 54(6), 960-963. 1999
http://www.researchgate.net/profile/Asha_Shahed2/publication/12696165_Quercetin_in_men_with_category_III_chronic_prostatitis_a_preliminary_prospective_double-blind_placebo-controlled_trial/links/00b4951a4d6cae42d9000000.pdf
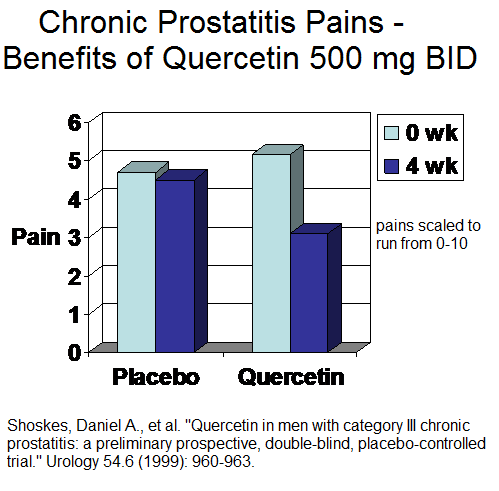 Study also demonstrated significantly reduced Isoprostate levels (indication of oxidative stress) in prostatic secretions after Quercetin.
Study also demonstrated significantly reduced Isoprostate levels (indication of oxidative stress) in prostatic secretions after Quercetin.
For chronic prostatism, they suggest amitriptyline 10–25 mg qhs or nortriptyline 10–
150 mg daily.
Treating Orchitis as Neuropathic Pain
Medication
Sinclair, Andrew M., Barry Miller, and Ling K. Lee.
Chronic orchialgia: consider gabapentin or nortriptyline before considering surgery. International journal of urology 14.7 (2007): 622-625.
http://www.ncbi.nlm.nih.gov/pubmed/17645606
- 1800 mg gabapentin/day or up to 150 mg nortriptyline /day
- “61.5% of patients commenced on gabapentin and 66.6% of patients commenced on nortriptyline had a greater than 50% improvement in pain”
- did not work much in post-vasectomy cases
Nerve blocks:
“local anesthetic and steroid may provide short-term and occasionally long-term relief, which may be repeated at varying intervals.”
Botulinum:
Khambati A, Lau S, Gordo A, Jarvi KA.
OnabotulinumtoxinA (botox) nerve blocks provide durable pain relief for men with chronic scrotal pain: a pilot open-label trial.
J Sex Med. 2014;11(12):3072 – 7
http://pvps.s3.amazonaws.com/202c4aabb87d8358d37abdd1412dcbeacdb267b3ad0.pdf
- 18 cases injected with 100 u Botox as cord block.”One hundred units of Botox was reconstituted in 10 cc of normal saline, and injected into the upper scrotum
approximately 1–2 cm distal to the external ring, infiltrating the branches of the genitofemoral and the ilioinguinal nerves”
Relief:
- Complete — 44% (8/18) in 1 month; 28% (5/18) in 3 months; 0% at 6 months
- Partial – 34%(6/18) at 1 month; 28% (5/18) in 3 month; 28% (5/18) at 6 months
Comments – I have injected a subject with occipital neuralgia for approx 15 years – 100-200 unit a time. The shot doesn’t rid the subject of pain but sensitizes the nerves to injections with semienurolytic 5-6% liodocaine ( I now add 3% glycerin as well and use up to 2 mls at a sitting) though it can take 1-3 sets of injections to get a good take – then he is good for maybe extent of botox which is 10-12 weeks. Expecting the Botox to do all the work is just silly.
Pelvic Floor treatments
That is a topic poorly covered and the reference they give is not available to me. Includes:
- biofeedback
- manual muscle testing
- pelvic floor massage
- medical management of constipation
- relaxation techniques
- development of an individualized home exercise program
Surgery
- Epididymectomy – 10 to 92 % success
better if palpable sore epididymis and tender cystic lesions in Epididymis that should be seen on US. If adjecent areas sore – less likely to work.
- in post-vasectomy pain syndrome, vasectomy reversal (open-ended procedure or with vasovasostomy)results in “50 to 69 % complete pain relief and up to 100 % having improvement of pain”
- If spermatic cord block successful, Microdenervation of spermatic cord (MDSC) gives 71-100% complete pain relief – suggested as best procedure.
- If prior epididymectomy, varicocelectomy, vasovasostomy, or herniorrhaphy – MDSC – as long as spermatic block successful, 50% do well
Pulsed radiofrequency
- of the spermatic cord and genital branch of the genitofemoral nerve
Terkawi, A. S., & Romdhane, K. (2014).
Ultrasound-guided pulsed radiofrequency ablation of the genital branch of the genitofemoral nerve for treatment of intractable orchalgia.
Saudi journal of anaesthesia, 8(2), 29
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4024696/
- 17 year old with bilateral pains
- “A confirmatory and diagnostic local anesthetic injection was performed between the internal and the cremaster fasciae using a 22-gauge insulated needle (in-plane technique), using 20 mg of methyl prednisolone and 5 mL of 2.5% bupivacaine bilaterally. The patient reported immediate pain relief that lasted for 6 weeks.”
- PRF of 42°C was applied for 120 sec
- still 0/10 – 7 months after
Misra, S., Ward, S., & Coker, C.
Pulsed radiofrequency for chronic testicular pain—a preliminary report.
Pain Medicine, 10(4), 673-678. 2009
http://www.ncbi.nlm.nih.gov/pubmed/19302438
- four 120-second cycles of 20-millisecond pulses at 2 Hz
- “Of the nine patients evaluated, four had complete resolution of pain, while one had partial pain relief. Three patients experienced no change and one reported that his pain was worse. All patients who experienced complete and partial pain relief continued to do so at a mean long-term follow-up of 9.6 months (range 3-14 months).”
Comment – I have found any chronic pain in area becomes “regionalized” – the skin will be tender on rolling all way to spine, there will be paraspinous spasm and facet levels will be tender. In the tender skin will be tender Thoracolumbar cutaneous nerves – I will inject every cm of them with 3% glycerin in D5W (call neural prolotherapy)- bleb more intradermal all the way round to back until no longer tender. I will inject superficially any paraspinous spasms laterally with 5% lidocaine and work out the spasms and then use manipulation (often an activator) to release facets. I will inject distally the affected nerves with 5% lidocaine until numb (limit 2 mls 5% lidocaine per sitting- less if old/infirm) This will need to be done repeatedly. Not enough experience to do a study but have seen success. From what I have seen , I would do the botox first and then follow with the semi-neurolytic lidocaine/glycerin
.