A study found falls in FM related to reduced dorsiflexion (bringing toes and foot up). The question is how does one fix that. Clin Biomech (Bristol, Avon). 2015 Apr 2. pii: S0268-0033(15)00102-3. doi: 10.1016/j.clinbiomech.2015.03.026. [Epub ahead of print] Ankle dorsiflexion may play an important role in falls in women with fibromyalgia. Góes SM(1), Leite N(2), Stefanello JM(3), Homann D(4), Lynn SK(5), Rodacki AL(6). http://www.ncbi.nlm.nih.gov/pubmed/25866321 FM cases analysis showed:
- higher plantar flexion during toe-off (P<0.05)
- reduced dorsiflexion during stance phase (P<0.05) associated with higher number of falls
- They give no ideas on what to do but I have written them…
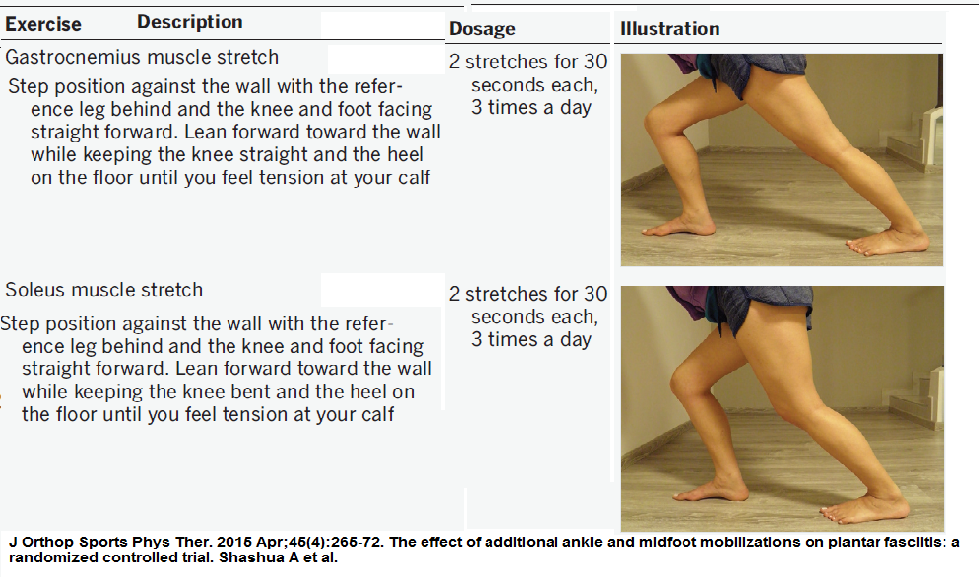
The problem could be one of ankle stiffness or one of contracture (tightening) of calf muscles. Here is one suggestion for injection gastrocnemius calf muscles: 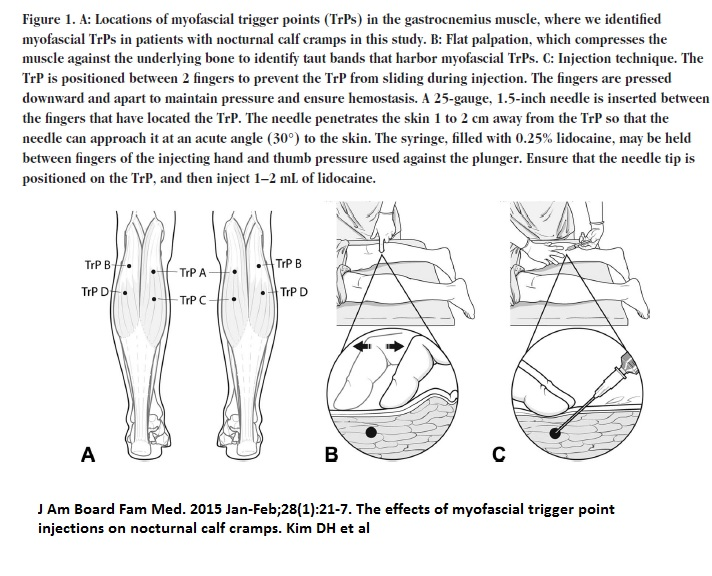 Sometimes there is a trigger a bit higher than that in muscle. After injection I push the muscle knots sideways until I can feel it loosening up. Then I knuckle it – strumming over it until it releases some as well. There, however is the Soleus muscle underneath that is wide as thick cardboard and very rigid. When pushing on it, there is no give at all. I inject it laterally – going horizontal to the posterior skin with a 2″ 25 gauge needle and fanning back and forth through the muscle. Stretching requires two techniques: 1) For gastrocnemius calf – put hands on wall, put leg to be treated behind other, and stretch as per pic and hold. Repeat times 3 and do 3 times daily. Maybe rub muscle after as any knotty-ness will smooth out some.
Sometimes there is a trigger a bit higher than that in muscle. After injection I push the muscle knots sideways until I can feel it loosening up. Then I knuckle it – strumming over it until it releases some as well. There, however is the Soleus muscle underneath that is wide as thick cardboard and very rigid. When pushing on it, there is no give at all. I inject it laterally – going horizontal to the posterior skin with a 2″ 25 gauge needle and fanning back and forth through the muscle. Stretching requires two techniques: 1) For gastrocnemius calf – put hands on wall, put leg to be treated behind other, and stretch as per pic and hold. Repeat times 3 and do 3 times daily. Maybe rub muscle after as any knotty-ness will smooth out some. 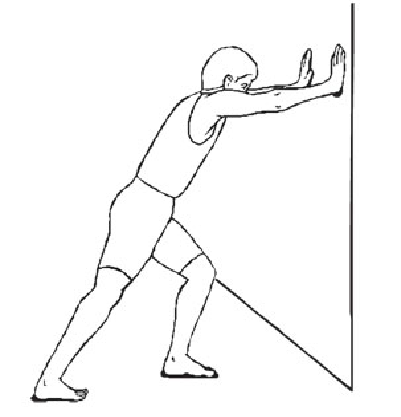
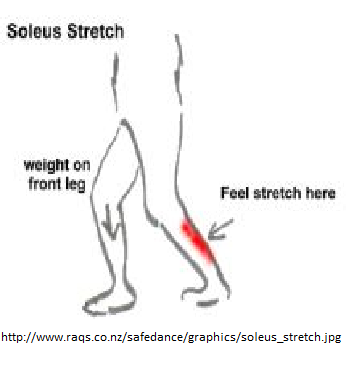
2) For Soleus: – put leg to be treated back and stretch forward with knee bent some Two techniques will facilitate the stretch:
- Push down with toes on treated leg for 10 – 15 seconds first – this will confuse the muscle and allow for a better stretch
- Go to sleep while stretching – OK not sleep but relax right down – you will be amazed how much give can be achieved that way.
In:
J Orthop Sports Phys Ther. 2015 Apr;45(4):265-72. doi: 10.2519/jospt.2015.5155.
The effect of additional ankle and midfoot mobilizations on plantar fasciitis: a randomized controlled trial.
Shashua A(1), Flechter S, Avidan L, Ofir D, Melayev A, Kalichman L
http://www.ncbi.nlm.nih.gov/pubmed/25739844
Better pic stretches (modified)
Some issues in FM that need attention:
1) Restless leg syndrome (RLS) – pain and urge to keep moving legs at night – common in FM and can be associated with small fiber neuropathy. I use Carbidopa-Levodopa (Sinemet) in a long acting formulation (Sinemet CR for example). I use Clonazepam in those who can’t sleep as well. Anti-Parkinson drugs have been shown to help FM some but are poorly tolerated.
Some of those with restlesss legs have potentially neuropathic levels of pain:
Clin J Pain. 2015 May;31(5):459-66. doi: 10.1097/AJP.0000000000000133.
Painful restless legs syndrome: a severe, burning form of the disease.
Karroum EG(1), Golmard JL, Leu-Semenescu S, Arnulf I.
http://www.ncbi.nlm.nih.gov/pubmed/25167326
little over 1/2 of RLS will be painful:
- burning” the most frequent ~40% description
- 1/3 found it “exasperating,” “exhausting,” and “unbearable.
Frequent B12 shots or B12 500 ug PO. (orally) tid for 3 months + has anti-neuropathic properties and found to help diabetic neuropathy
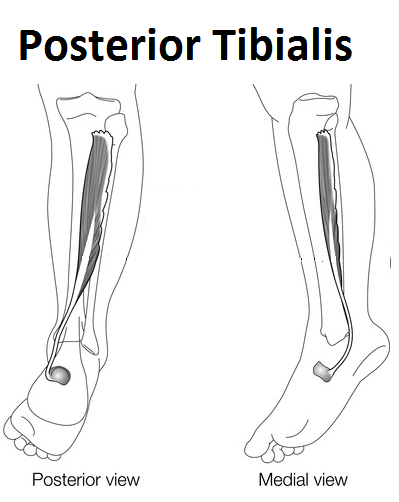
2)Pes planus (flat feet)and tibialis posterior spasm
This is called posterior shin splints and very common in people with sore legs. I needle anteriorly often at 2 levels found tender posteriorly – pulse with a pointer plus for 2-3 minutes each. Then I rub out any residual soreness. Amazing relief surprises a sore leg patient. Why go anterior? – safer as blood vessels and nerves from other direction. 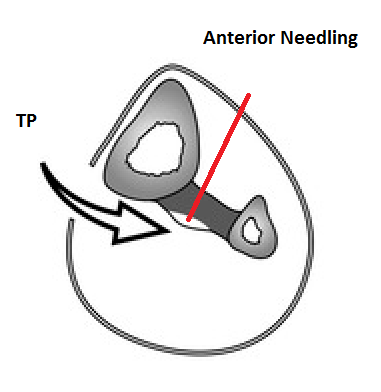 Night splints – as with treatment of plantar fasciitis, I suspect calf muscles tighten up at night (helps to have a pillow or a board at foot of bed lifting sheets off feet). Maybe just do one at a time as tolerance is an issue.
Night splints – as with treatment of plantar fasciitis, I suspect calf muscles tighten up at night (helps to have a pillow or a board at foot of bed lifting sheets off feet). Maybe just do one at a time as tolerance is an issue.
Plantar fasciitis night splint.
Ankle mobs: -plantar dorsiflexion should reach 20 degrees and if not able then mobilizations to ankle might help Talocrural Joint Glides: grab foot and heel – move one one direction while moving other opposite – back and forth -having it over edge of bed might help to hold it down.
Addendum:
InJ Orthop Sports Phys Ther. 2015 Apr;45(4):265-72. doi: 10.2519/jospt.2015.5155.
The effect of additional ankle and midfoot mobilizations on plantar fasciitis: a randomized controlled trial.
Shashua A(1), Flechter S, Avidan L, Ofir D, Melayev A, Kalichman L
http://www.ncbi.nlm.nih.gov/pubmed/25739844
- Did not find ankle mobilizations increased plantar dorsiflexion ubt stretches did – in plantar fasciitis cases
Pic ankle mobs (modified):

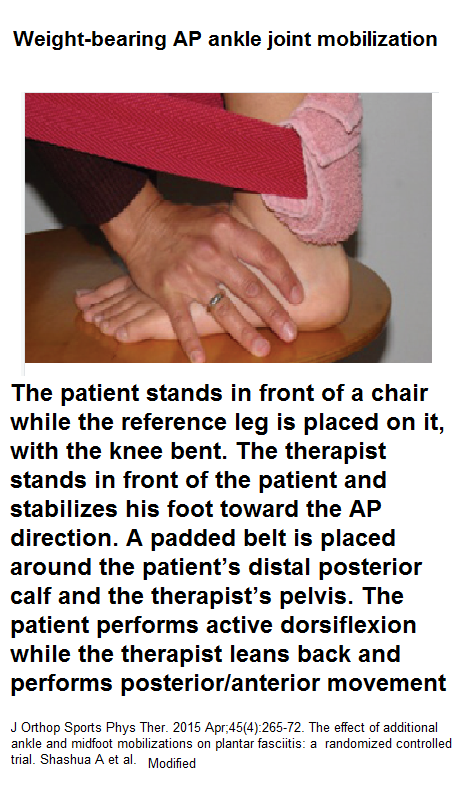
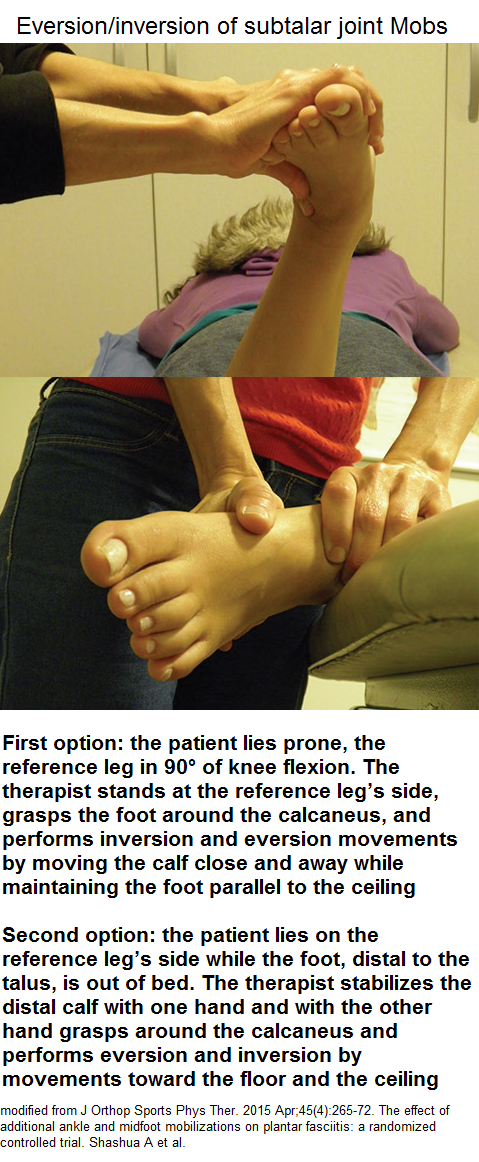
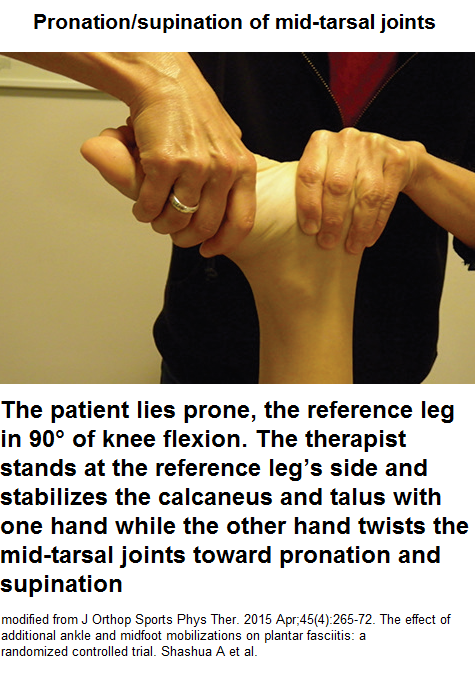 Though mobs did not help plantar fasciitis – still might help FM…
Though mobs did not help plantar fasciitis – still might help FM…
Any suggestions?


I did kindly receive an answer from author and it is enclosed here:
I read your blog and agree with all interventions you suggested.
The data from this paper is based on kinematics, so we could not confirm the forces and the muscle activation during gait. Here some thoughts about interventions:
I agree that ankle mobilizations would help with the joint stiffness that might be present considering our findings, specifically working on increasing the dorsiflexion ROM.
Massage would help on pain, since pain may lead to co-activation of antagonist muscles (plantar flexors), in order to protect the (painful) muscle during contraction, with muscular adaptation to limit joint ROM. Individuals with FM might have distal ankle plantar flexor muscles over worked, producing muscle shortness and tightening, which leads to dorsiflexion restriction.
About exercises I think not only focus on the ankle but also on the hip, we did not see in our results, but the literature shows that decreased ankle dorsiflexion is likely to increase the amount of hip flexion necessary to achieve toe clearance (Perry and Burnfield, 2010). In addition, changes in ankle kinematics are secondarily related to hip flexion contracture impairment in the elderly.
Ankle problems can probably be affected by inefficient pelvic and/or hip stabilization. The literature in mechanics of the ankle, specifically in ankle injury shows that a relationship has been shown between the mechanics at the ankle and the mechanics of more proximal joints (hip). It seems that control at the hip is vital for maintaining control at the ankle (Friel et al., 2006; Sadeghi et al., 2001). So, stretching exercise no the hip flexors and muscle strength exercise on gluteus muscles and hip abductors would increase the hip ROM and possibly help on ankle ROM.
References:
Perry J, et al. Gait Analysis: Normal and Pathological Function. Thorofare: Slack; 2010.
Friel , K, McLean N, Myers C, Caceres M. Ipsilateral Hip Abductor Weakness After Inversion Ankle Sprain. Journal of Athletic Training 2006;41(1):74–78.
Sadeghi H, Sadeghi S, Prince F, Allard P, Labelle H, Vaughan C. Functional roles of ankle and hip sagittal muscle moments in able-bodied gait. Clin Biomech (Bristol, Avon) 2001;16:688–695.
I hope this suggestion could clear your concerns.
Please do not hesitate to contact me if you want to discuss more about this topic.
Best regards,
Suelen M. Góes
—————————–
Suelen Meira Góes, PhD
Postdoctoral Fellow
Faculty of Health Professions
Dalhousie University
Halifax, NS
“Some people are afraid of change. I am afraid things never change.” Chico Buarque?
————
Thank you Dr. Suelen Góes
-admin
Michael Montbriand MD CCFP
admin@painmuse.org