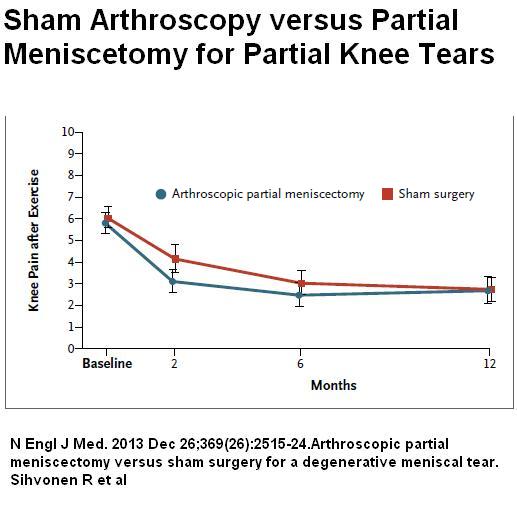
Quite some years ago, NEJM published an article saying flushing of the knee did not help knee pains, putting an end to that procedure. Now an article has been published by same journal says that partial arthroscopic meniscetomy does not work because flushing with sham surgery alone will decrease pain by 50% in two months. Sorry, NEJM, you can’t say both…
N Engl J Med. 2013 Dec 26;369(26):2515-24.
Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear.
Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, Kalske J, Järvinen TL
http://www.ncbi.nlm.nih.gov/pubmed/24369076
- 146 cases – 35-65 yrs old with partial meniscus tears knee
- cases had minimal OA in knee and were expected to benefit from surgery.
- One group had arthroscopy; one group had arthroscopy and menisectomy
Results:
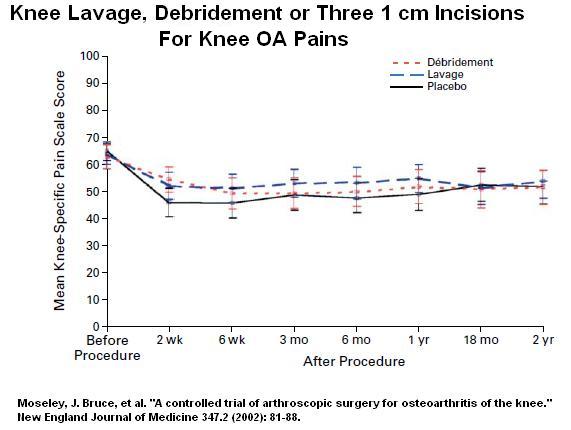
Prior Knee flushing article:
Moseley, J. Bruce, Kimberly O’Malley, Nancy J. Petersen, Terri J. Menke, Baruch A. Brody, David H. Kuykendall, John C. Hollingsworth, Carol M. Ashton, and Nelda P. Wray.
A controlled trial of arthroscopic surgery for osteoarthritis of the knee.
New England Journal of Medicine 347, no. 2 (2002): 81-88.
http://faculty.fortlewis.edu/burke_b/Criticalthinking/Readings/Moseley%20et%20al%20-%20placebo%20surgery.pdf
Comment:
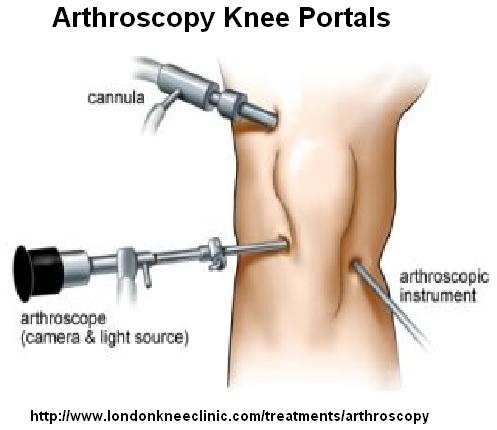
For some reason or other, arthroscopy is considered an inert process. They do state the “use of standard anterolateral and anteromedial portals and a 4-mm arthroscope”. They do not state is a trocar was introduced superiorly to flush or inspect as well though that wouls have been standard.
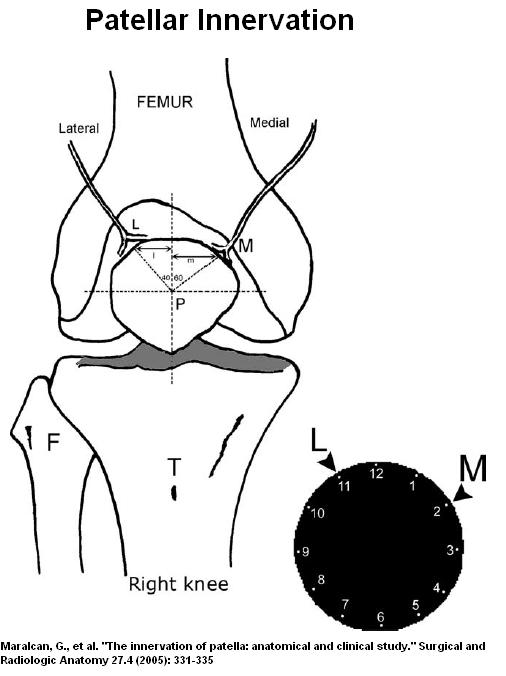
In both present study and the knee flushing study, the superior site would have had a direct effect of patellar innervation. Trocars are often 4 mm in size and could easily cut one of the nerve leading to patella:
 Beyond that, one is left with the distinct feeling that flushing the knee during arthroscopy must have had a therapeutic effect. This brings into question a previous NEJM article stating it does not. Make up your mind NEJM! – you can’t have both… I noticed they did not touch the issue of benefits with surgery except to consider “placebo effect” – something I doubt is the full story. Could be the degree of OA in lavage study prevented it from showing benefit…
Beyond that, one is left with the distinct feeling that flushing the knee during arthroscopy must have had a therapeutic effect. This brings into question a previous NEJM article stating it does not. Make up your mind NEJM! – you can’t have both… I noticed they did not touch the issue of benefits with surgery except to consider “placebo effect” – something I doubt is the full story. Could be the degree of OA in lavage study prevented it from showing benefit…
Addendum:
Article published does put this in some perspective:
Curr Opin Rheumatol. 2013 Dec 26. [Epub ahead of print]
Knee osteoarthritis and role for surgical intervention: lessons learned from
randomized clinical trials and population-based cohorts.
Buchbinder R, Richards B, Harris I.
http://www.ncbi.nlm.nih.gov/pubmed/24378932
“large randomized controlled trial has demonstrated that arthroscopic partial meniscectomy followed by a standardized physical therapy program results in similar improvements in pain and function at 6 and 12 months in comparison to physical therapy alone in patients with knee osteoarthritis and a symptomatic meniscal tear, confirming the findings of two previous trials.”
Having said that, people don’t have access to much physiotherapy as much as coverage is sparse….
A warning is sounded:
“A majority of studies have indicated that for people with obesity the positive results of total knee arthroplasty may be compromised by postoperative complications, particularly infection.”
Any comments?

Thank you for bringing some sound clinically applicable logic to this process. The 4 mm trocar would impact the cutaneous distribution of nocioception and would no doubt impact that sensation.
We all know the primary function of sensory nerves is to detect and transmit mechanical information from the joint to the central nervous system. Large diameter myelinated nerve fibres encode and transmit proprioceptive signals, which can be interpreted as being either dynamic (movement sensations) or static (position sense). Pain-sensing nerve fibres are typically less than 5 μm in diameter and are either unmyelinated (type IV) or myelinated with an unmyelinated ‘free’ nerve ending (type III). These slowly conducting fibres typically have a high threshold and only respond to noxious mechanical stimuli, and as such are referred to as nociceptors. Could the insult and injury to these fibers with the “sham” procedure be the cause for decreased pain?
Given that peripheral nerves will regenerate very slowly (how many female patients after a knee scope complain they can’t feel their skin when they chave?), and that likewise their deeper counterparts are equally slow in healing this will no doubt impact nocioceptive sensation and perception in the knee.
I think another key point being missed is the use of NSAIDS and other pharmaceutical agents to control pain in these patients and what impact this had on the outcomes. If the patient had a healthy dose of NSAIDS, or a recent injection and then fill out the Lysholm or WOMET (the WOMET is a woefully horrible outcomes based measure only exceeded in its funcitonal use by the lysholm) then those scores will be skewed.
So if I exercise, get injections, live on NSAIDS I can put off a TKA for a year. Now in that year the intra-articular injections will conitnue to retard my muscle function and inhibit its return, as will the pain, the intra-articular swelling and its effect on first order neurons and in a year or two the patient is back in our office for their TKA.
Now because we have filled the joint with everything under the sun will the remaining bone be acceptable to the prosthesis as well? Will the healing be any better because a lot of acceptable treatments supress the healing process? I think we all know the answer to this one.
The study leaves me wondering how they choose and excluded participants as well. The methods in the abstract said 146 (after narrowing down from 205) patients were selected who had knee symptoms consistant with a degeneritive tear of the medial meniscus but no osteoarthritis. Where in the universe does this type of knee exist? You have a degeneritive processs in one aspect of the intra-articular structures and nothing else . . .no osteochondral lesions? bone bruises? chrodromalacia in the patella?
It is a poorly designed study using questionable outcomes measures ( I am a physical therapist and do not find either scale to be a true measure of function; I mean who measured the WOMET). It is a visual analog scale meaning it is measured with a metric ruler and 1 or 2 mm indicates improvement. The Lysholm, we have better tools for measuring outcomes.
The most telling comment in this very controlled study was in the closing paragraph of the discussion. “However’ increased evidence suggests that a degeneritive meniscal tear may be an early sign of knee osteo-arthritis rather than a separate problem requiring meniscal intervention”. If you have a degneration of the shock absorbing cartilage in any knee, the result of abnormal biomechanics on a comprimised structure will lead to unbalanced loading of the knee and cause/exacerbate intra-articular knee compartment issues. So that is why I question these pristine knees with degeneritive meniscal injuries with no other signs of OA or OCD’s.
EMG studies before, immeadiatley after, and at 3,6,9, and 12 month intervals would have yielded some tangible evidence with subjective based outcomes scores.
Great, now we will have to do double sommersaults to get our patients the care they need