Since 2001, there have been case studies showing you can grow low grade anaerobes out of damaged discs; these ignored as contamination or incidental because some studies did not find any infection. Now it appears that those with positive cultures are 5.6 times more likely to subsequently develop “Modic” end plate changes. A separate article also in press found following 100 days of antibiotics, chronic Back pain cases, with modic degenerative changes in the backbone improve. They have 1/2 the pain level, a year later, versus no change in control group. They toted this as substantially better than any established conservative treatment.This represents a huge shift in thinking about discogenic neck and back pain.
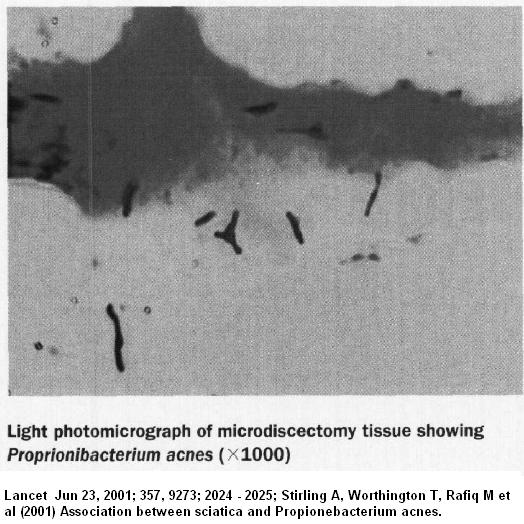
Several case studies grew low grade anareobic bacteria out of discs in 1/3 to 1/2 of cases ( like helicobacter pylori was before taken seriously). The initial study was published in Lancet in 2001. Lancet Jun 23, 2001; 357, 9273; 2024 – 2025;
Stirling A, Worthington T, Rafiq M et al
Association between sciatica and Propionebacterium acnes. no abstract.
They found 53% infected. They suggested the need to incubate these organism for 7 days might be the reason they were not previously recognized. They could however, see them even in sections of disc tissue (see below). In many cases they found two organisms – Propionebacterium acnes and Corynebacterium and occasionally Staphlococcus. There was no association of positive cultures and previous epidural injections.
Stirling Repeated his study on 62 microdiscectomy patients with sciatica using “stringent aseptic precautions”.
A.J. Stirling, M. Rafiq, K. Mathur, T.S.J. Elliott, T. Worthington and P.A. Lambert
Association between Sciatica and Skin Commensals.
Bone Joint Surg Br 2002 vol. 84-B no. SUPP II 147
http://www.bjjprocs.boneandjoint.org.uk/content/84-B/SUPP_II/147.2.short
He found 43% infected – again, P. acne being the most prominant organism. To corroborate his findings, he looked for elevations of Anti Lipid S antibody levels. They were elevated in 1/3 of the infection group but in only one of the “control” group.
Hanne (ref below and here) discussed another Stirling study
“Stirling et al. conducted another study with 207 patients with lumbar disc herniation and 27 patients with other spinal disorders such as scoliosis, fracture and tumors, all patients had nucleus material removed. In 37 % of the patients with lumbar disc herniation bacteria were indentified, mainly P. acnes. Conversely,no (0 %) bacteria were found in the extracted nuclear material in the group with other spinal disorders.”
A study using detection of baterial RNA by PCR was able to detect infection in 2/10 cases:
Eur Spine J. 2004 Dec;13(8):702-6.
Detection of bacterial DNA in painful degenerated spinal discs in patients without signs of clinical infection.
Fritzell P, Bergström T, Welinder-Olsson C.
Eur Spine J. 2004 Dec;13(8):702-6. Epub 2004 May 8.
A poster at a British Orthopedic meeting looked into this issue:
Corsia MF, Wack M, Denys G (2003)
Low vitulence Bacterial infections of intervertebral discs and the resultant spinal disease processes.
Abstract from Scoliosis Research Society (SRS) annual meeting
- 30 lumbar and 30 cervical discs
- 71% lumbar and 57% of cervical disc were infected
- mosly p.acnes and staphlococcus
A recent study during microdiscectomy found 13.5% infection rates – mostly P. acne though few Peptostreptococcus and Staphlococcus:
Journal of Spinal Disorders & Techniques: August 2011 – Volume 24 – Issue 6 – p 397–400
Bacteriologic Culture of Excised Intervertebral Disc From Immunocompetent Patients Undergoing Single Level Primary Lumbar Microdiscectomy
Agarwal, Vijay MD*; Golish, S. Raymond MD, PhD†; Alamin, Todd F.
http://journals.lww.com/jspinaldisorders/Abstract/2011/08000/Bacteriologic_Culture_of_Excised_Intervertebral.10.aspx
Yet another study was done by preoperative discography for disc surgery:
BACTERIOLOGY OF THE LUMBAR INTERVERTEBRAL DISC IN DEGENERATIVE DISC DISEASE
Joseph Arndt, Yann Charles, Ioan Bogorin and Jean Steib
J Bone Joint Surg Br 2012 vol. 94-B no. SUPP XXXVII 276
http://www.bjjprocs.boneandjoint.org.uk/content/94-B/SUPP_XXXVII/276.abstract
- 83 cases
- “Germs were found in 40 discs, 43 cultures were sterile. “
- again, p. acne and staph predominated
- “Histological examination of 31 discs found inflammatory cells in 33 % of the biopsies with positive bacterial culture, versus 5 % of the sterile biopsies (p=0.038)” – the inflammation confirming potential infection was present.
- Men were more affected; L4/5 was the most positive level;
- they did not find modic changes at the time were necessary (though another article suggested they come later).
These results were not taken seriously because they were thought to be skin contamination or incidental as some studies grew no such organisms. However, the fact that Striling above could not grow germs out of disc samples during surgery for spinal tumors, vertebral fractures and scoliosis surgery made contamination less likely.
These infections are thought associated with sclerotic changes to vertebral end plates and associated bone edema seen on MRIs as Modic changes. It is felt the anaerobic organisms thrive in the lower oxygen environment in these sclerotic areas.
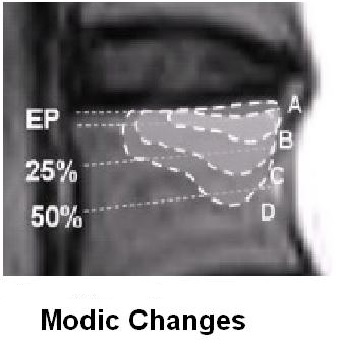 Modic changes occur in 46% of non-specific low back pains versus 6% of the general population. as per review:
Modic changes occur in 46% of non-specific low back pains versus 6% of the general population. as per review:
Eur Spine J. 2008 Nov;17(11):1407-22.Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain.
Jensen TS, Karppinen J, Sorensen JS, Niinimäki J, Leboeuf-Yde C. abstract here
As mentioned, the organisms involved include Proprionibacterium acnes (Yes – acne of the spine), Corynebacterium propinquum, and Staphlococcus. There was some concern at one point that certain Cornebacterium are just a flavor of Proprionibacterium serologically:
Corynebacterium parvum: a Synonym for Propionibacterium acnes?
C. S. Cummins and J. L. Johnson
Microbiology February 1974 vol. 80 no. 2 433-442 abstract here
An article in press found if organisms are grown, Modic changes are likely to develop later in 80% of cases (5.6 times as likely as those without organisms) leading authors to speculate infection fostered the modic changes/bone marrow edema. They found a 45% infection rate – mostly p.acne. To confirm their findings they did PCR amplification for bacterial RNA in disc tissue – they found it positive in all cases of culture positive but negative in all cases of culture negative.
European Spine Journal February 2013 in press
Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae?
Hanne B. Albert, Peter Lambert, Jess Rollason, Joan Solgaard Sorensen, Tony Worthington, Mogens Bach Pedersen, Hanne Schack Nørgaard, Ann Vernallis, Frederik Busch, Claus Manniche
http://link.springer.com/article/10.1007/s00586-013-2674-z
Taking it even further, is an article showing that 100 days of Clavulin 500 TID for 100 days can drop pain back pain scores from 6.7 to 5 in 100 days and to 3.7 in one year (versus 6.3 – 6.3 – 6.3 in the double blind control group): There were 90 in treatment and 72 in placebo. Clavulin was picked because of its lack of anti-inflammatory effects which could confuse the issue. Statistically, p= 0.0001. Leg pains did even better dropping from 5.3 to 1.4/10 while control group actually went up from 4 to 4.3/10.(p=0.0001). Clavulin was apparently used in order to avoid confusion over anti-inflammatory effects of certain antibiotics.
European Spine Journal February 2013 in press
Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy
Hanne B. Albert, Joan S. Sorensen, Berit Schiott Christensen, Claus Manniche
http://link.springer.com/article/10.1007/s00586-013-2675-y
They felt their results with known resistant cases “has been substantially greater than those described with all other established conservative treatments”. Results do speak for themselves…
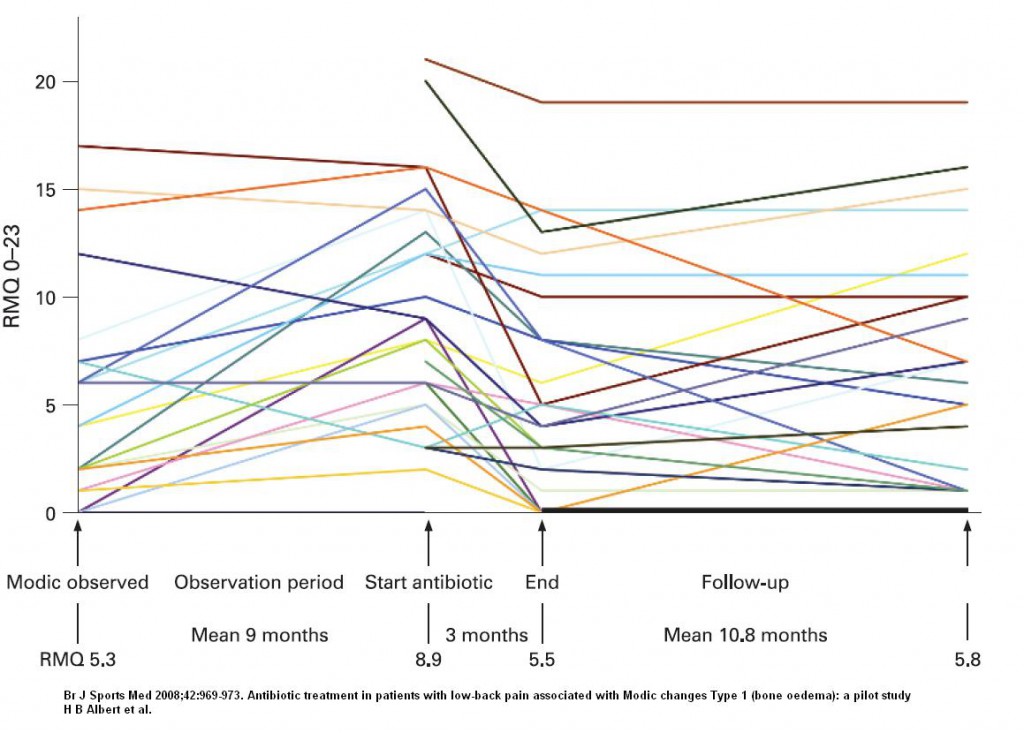
This study was done following the success of a pilot study:
Br J Sports Med 2008;42:969-973
Antibiotic treatment in patients with low-back pain associated with Modic changes Type 1 (bone oedema): a pilot study
H B Albert, C Manniche, J S Sorensen, B W Deleuran free full article:
http://bjsportmed.com/content/42/12/969.full.pdf+html
- They took cases that showed “modic changes” on mri
- They gave Clavulin 500 tid for 90 days
- 3 dropped out because of diarrhea leaving 29 subjects
- Results were: “Using the measure of global perceived health, at the end of treatment, 15 (52%) of the patients reported that they were much better or cured, seven (24%) were moderately better, and seven (24%) reported they were unchanged”.
- What however, is disturbing, is the increase in Disability levels seen in some cases after antibiotics were stopped:
| worsening after finishing in some —–>
—————————————-
There are articles that disagree infection exists:
Association Between Sciatica and Microbial Infection:
True Infection or Culture Contamination?
Peleg Ben-Galim, MD,* Nahshon Rand, MD,† Michael Giladi, MD,‡ David Schwartz, PhD,§
Ely Ashkenazi, MD,† Michael Millgram, MD,† Shmuel Dekel, MD, PhD,* and Yizhar Floman
SPINE Volume 31, Number 21, pp 2507–2509 free article here
http://library.tasmc.org.il/wwwnew/Staff_Publications/publications%202006/ben-galim1.pdf
They could have helped clear up the issue but did not have the courage of their convictions and put their subjects on preoperative antibiotics. The did not grow anything, but is well known you can’t grow bugs out of urine in bladder infections if on antibiotics so why should it be any different here? Cannot understand why they didn’t give intraoperative antibiotics after they got samples…
Another negative study:
No Evidence for Presence of Bacteria in Modic Type I Changes
Musculosketal Radiology 2009, Vol. 50, No. 1 , Pages 65-70
N. Wedderkopp1,4†, K. Thomsen1,4, C. Manniche3, H. J. Kolmos1,4, T. Secher Jensen4 and C. Leboeuf Yde
http://informahealthcare.com/doi/abs/10.1080/02841850802524485
They actually found 2/24 cases grew staph but they dismissed them as contamination despite “strict asepsis” used in collection. I do not have information on whether they used preop antibiotics as journal is not received by our university. There results, however, make the situation very confusing.
Another study grew p.acne in 3.7% of disc cases but were able to grow the organism from a variety of surfaces (including muscle) and concluded contamination was more likely:
Journal of Hospital Infection (2007) 66, 275-277
Propionibacterium acnes contamination in lumbar disc surgery
A. Carricajo,*, C. Nuti, E. Aubert, O. Hatem, N. Fonsale, F.O. Mallaval, A.C. Vautrin, J. Brunon, G. Aubert free article below:
http://www.ccih.med.br/m/aluno/mod/biblioteca_virtual/revistas_2007/jornal_of_hospital_infection/julho/275.pdf
———————–
Came across a study of frank disc infection from Proprionibacterium acnes:
Clin Microbiol Infect. 2010 Apr;16(4):353-8.
Spondylodiscitis due to Propionibacterium acnes: report of twenty-nine cases and a review of the literature.
Uçkay I, Dinh A, Vauthey L, Asseray N, Passuti N, Rottman M, Biziragusenyuka J, Riché A, Rohner P, Wendling D, Mammou S, Stern R, Hoffmeyer P, Bernard L.
free article here
29 cases
- fever rare; back pain with average 4.7 months delay in diagnosis
- Often post surgical cases but with delay of 34 months in between so wonder how relevant.
- thoracic in 14 cases, lumbar in 13 cases, and thoraco-lumbar in two cases
- Three patients had a peripheral neurological deficit, one a motor deficit, and two a sensory deficit.
- Six had an epidural abscess
- Only one had a positive blood culture
- 83% had surgical debridement
- Drugs used in various studies – Pen G, Clindamycin, clavulin, and floroquinolones; in some cases clindamycin and the other drugs combined. Also tried was combination of amoxicillin and clindamycin. Fluoroquinolones were preferred. This organism is apparently resistant to flagyl.
- minimum treatment time was 6 weeks; cures were not difficult to achieve.
——————————–
It has been known that pamidronate can benefit chronic back pain and maybe it works on this Modic change bone marrow edema:
Journal of Pain and Symptom Management Volume 26, Issue 1, July 2003, Pages 678–683
Treatment of chronic mechanical spinal pain with intravenous pamidronate: a review of medical records ☆
Marco Pappagallo, MD, Brenda Breuer, PhD, MPH, Aaron Schneider, NP, Kevin Sperber, MD
http://www.sciencedirect.com/science/article/pii/S088539240300201X
Given that modic changes represents bone marrow edema, the finding that IV Ibandronate works on bone marrow edema in legs, confirms its potential there:
Arch Orthop Trauma Surg. 2012 Dec;132(12):1781-8.
Treatment of bone marrow edema syndrome with intravenous Ibandronate.
Bartl C, Imhoff A, Bartl R. a abstract and first part
——————-
A study on exercise therapy for patients with modic changes found no benefits; maybe infection explains why.
BMC Med. 2012 Feb 29;10:22. doi: 10.1186/1741-7015-10-22.
Rest versus exercise as treatment for patients with low back pain and Modic changes. A randomized controlled clinical trial.
Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Manniche C.
free article here
————————-
This paradigm would explain why injection of ozone into discs has been found to be some effective in chronic discogenic back pain:
Ozone Therapy as a Treatment for Low Back Pain Secondary to Herniated Disc: A Systematic Review and Meta-analysis of Randomized Controlled Trials
Francisco N. De Oliveira Magalhaes, MD, Luciana Dotta, MD, Andre Sasse, PhD, Manoel J. Teixeira, MD, PhD, and Erich T. Fonoff, MD, PhD
Pain Physician 2012; 15:E115-E129 • ISSN 2150-1149 – free article below
http://www.painphysicianjournal.com/2012/march/2012;15;E115-E130.pdf
refers to studies:
“In the randomized series of 306 patients, Bonetti et al (14) reported that 57.5% of 80 patients in the disc disease group treated with steroid deemed the clinical outcome to be excellent, as did 62.8% of 70 patients in the group with no disc disease after steroid infiltration (Table 4). Whereas in the ozone therapy group, 74.4% of 86 patients with disc disease reported complete remission
of pain, as did 75.0% of 70 patients with no disc disease. In this study, differences in favor of O2-O3 treatment were statistically significant in patients with disc disease but not in those without disc disease.”
also:
“Zambello et al (15) randomized 351 patients with low back pain for treatment with either ozone or steroid (epidural) and planned a crossover during the followup to the other group in case of failure to respond to treatment after 4 weeks of therapy. The long-term outcome remained excellent or good in 47.3% of 171 patients treated by epidural steroid injections and in 77.1% of 180 patients treated with O2-O3.”
Key points from abstract:
Results: Eight observational studies were included in the systematic review and 4 randomized trials in the meta-analysis. The indicated level of evidence for long-term pain relief was II-3 for ozone therapy applied intradiscally and II-1 for ozone therapy applied paravertebrally. The grading of recommendation was 1C for intradiscal ozone therapy and 1B for paravertebral ozone therapy.Limitations: The main limitations of this review are the lack of precise diagnosis and the frequent use of mixed therapeutic agents. The meta-analysis included mainly active-control trials. No placebo-controlled trial was found.
Conclusions: Ozone therapy appears to yield positive results and low morbidity rates when applied percutaneously for the treatment of chronic low back pain.
———————————————
Comments – must admit after the XMRV – Fibromyalgia fiasco I am reluctant to believe in infections. However, I have two cases so far, that have more pain than they would think they should have, and want to try the antibiotics. Presence of irritable bowel/diarrhea issues limits selection using clavulin but looks like flouroquinolones could be used… I’ll let you know in 3-12 months… A annoying thought is whether the infection comes back after stopping antibiotics and this is why there is relapse of some after the 90 days of antibiotics – are we really going to need to keep some of these cases on antibiotics like acne cases? I’ve had trouble getting people to tolerate the 500 mg clavulin and suggest probiotics. – maybe consider using 250 mg after first week?
addendum – Warning has been sent out to avoid missing blatant disciitis/osteomyelitis in IV drug users: – case presented of patient with multiple emerg visits for back pain finally found to have disc infection:
Case Rep Infect Dis. 2013;2013:729812. doi: 10.1155/2013/729812. Epub 2013 Oct 2.
Unusual case of osteomyelitis and discitis in a drug user with a background of
chronic back pain: do not miss the serious etiologies.
Ali AM, Khan M, Kwatra SG, Barbaryan A, Hussain N, Saba R, Mirrakhimov AE.
http://www.ncbi.nlm.nih.gov/pubmed/24198986
“We present a case of a 50-year-old male with a past medical history of chronic back pain and IV drug abuse who presented with acute back pain and in whom a diagnosis of vertebral osteomyelitis was missed during multiple visits to the emergency room.”
———————————–
Followup Review 2015:
Spine (Phila Pa 1976). 2015 May 15;40(10):E587-E592.
Can Bacterial Infection by Low Virulent Organisms Be a Plausible Cause for Symptomatic Disc Degeneration? A Systematic Review.
Ganko R(1), Rao PJ, Phan K, Mobbs RJ.
RESULTS:
“Nine relevant studies involving 602 patients with degenerative disc disease or pain were identified. From 6 studies supporting the role of infection in the pathophysiology of disc degeneration, the pooled infection prevalence was 45.2% (34.5%-56.0%). Overall pooled prevalence in all studies was 36.2% (24.7%-47.7%). Proportion of disc infections was higher in patients with symptomatic disc disease than in patients without (37.4% vs. 5.9%; odds ratio, 6.1; 95% confidence intervals, 1.426-25.901). The majority of infections were due to Propionibacterium acnes in 59.6% (43.2%-76.1%).”
CONCLUSION:
“From the limited evidence available, the possibility that disc infection may be linked with disc degeneration should not be ruled out. There is a need to investigate this further through larger, adequately powered multi-institutional studies with contaminant arm to control for specimen contamination.”
Addendum: – recently clavulanic acid has been found to have anti-neuropathic pain properties:
The b-lactam clavulanic acid mediates glutamate transport-sensitive pain relief in a rat model of neuropathic pain
P.J. Kristensen et al
Eur J Pain 22 (2018) 282–294
http://onlinelibrary.wiley.com/doi/10.1002/ejp.1117/full
“Chronic dosing of clavulanic acid alleviates neuropathic pain in rats and up-regulates glutamate transporters both in vitro and in vivo. Crucially, a similar up-regulation of glutamate transporters in human spinal astrocytes by clavulanic acid supports the development of novel b-lactam-based analgesics, devoid of antibacterial activity, for the
clinical treatment of chronic pain.”
this cast doubt over fact 100 days of clavulin 500 tid relieves back pain due to infectious issues

From admin – recently saw a retired police officer in his late 50’s with severe chronic back pain – he has been on 3 months of a Flouroquinolone. I asked him how his back was and he said “what back pain?” – pain was gone and no longer even a thought for him…I have had trouble getting any of my cases on Clavulin to continue taking it because of diarrhea – would suggest all need to be on probiotics. Had one patient on flouroquinolones develop peripheral neuropathy – (lower 1/3 of legs numbish) which has been recently added as a complication of these drugs…He ended up having surgery for spondylolithesis so was probably not a good choice to start with. I still think flouroquinolones are best choice (I am used to Levaquin 500 mg od as used in chronic prostatitis for weeks – months without side effects except my recent case…). One doctor suggested azithromycin as shown to work in acne. The surprisingly good results of pamidronate in chronic back pain has hijacked my interests right now.
I have had severe back pain for almost 8 years, which after a couple of years began spreading throughout my body. I have now overall pain and my left arm is pretty much useless due to this pain. I feel my right arm going the same way. I have only ever had 3 periods pain free and that was when I was administered antibiotics for other medical reasons. My symptoms disappeared each time within 2 days and I felt like I had my life back. Unfortunately no Dr will admit to antibiotics being the answer, they dismiss it as a “coincidence”. Once or even twice could be considered coincidence but not three times. I am consistently refused antibiotics even though this would allow me to lead a near normal life. The NHS would much rather have me taking morphine at considerably expense to the tax payer. I am at my wits end and increasingly feel there is no other option open to me. If I was brave enough I would have ended it a long time ago. I am tired of being denied treatment which would change my life and allow me to be a useful member of society once again.
——————-
From Admin:
Your history sounds horrible.
Print out my article and take it to your doctor maybe. Came across an article in the 1920’s about chronic back pain being related to low grade chronic prostate infection (stayed chronic because they had no antibiotics in those days) – do you have any frequency (going to pee often)? – if so, put it to you doc that maybe you have a chronic prostate infection – these are often undiagnosable because the urine tests are often negative but most often they respond to an antibiotic called Levaquin (concentrates in prostate better than cipro). In order to eradicate prostate infection, one usually gives a 3 week course because the germ “cysts” are not killed until they germinate. For chronic repeat infections I have gone 6 weeks and rarely 3 month. Unfortunately, floxins can cause tendonitis (achilles tendonitis, tennis elbow etc.) and peripheral nerve damage (neuropathy causing numb feet); diabetic who are already numb feet would have numbness potentially extending up leg. Also in diabetics it can cause flucuations of their sugars. – Not necessarily a diabetic friendly drug. -Let me know if you have any luck..
I have had no luck using chronic 500 mg level Clavulin as the clavulanic acid in it, causes diarrhea (even in some of my opioid constipated patients).
Your IP appears to be in the UK; there is an advocate for infected disc treatment there -Dr. Peter Hamlyn, a private spinal surgeon and honorary consultant neurosurgeon at University College London Hospital. He has a webpage:
http://www.spinesurgerylondon.com/about-us/the-spine-surgery-team/medical/spinal-surgeons/peter-hamlyn#
(click on the left where it talks about disc infections)
Perhaps contacting his office (talk to the nurse who will either advise or will talk to the Dr. and then advise) – will help in your country. If they won’t talk to you let me know and I will try to email him…
Good luck
Admin