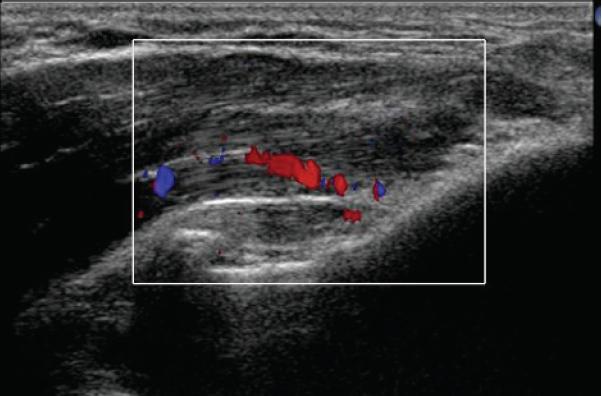
Studies on Achilles, Patellar and Lateral epicondylar (tennis elbow)tendonitis have demonstrated the ultrasound demonstrable appearance of a “vasculo-neural growth” that corresponds to the site of pain. In long-term resistant cases, treating these lesions with sclerosing agent, polidocanol, under ultrasound guidance; led to “clinically good results” in most cases. Disappearance of the “vasculo-neural growth” corresponded to the improvement.
(This in not the first time pain has grown its own “nerve supply”. In endometriosis, the lesions grow highly innervated pain fibers. )
Knee Surg Sports Traumatol Arthrosc. 2006 Sep 8; [Epub ahead of print]
Sclerosing polidocanol injections in chronic painful tennis elbow-promising results in a pilot study.
Zeisig E, Ohberg L, Alfredson H
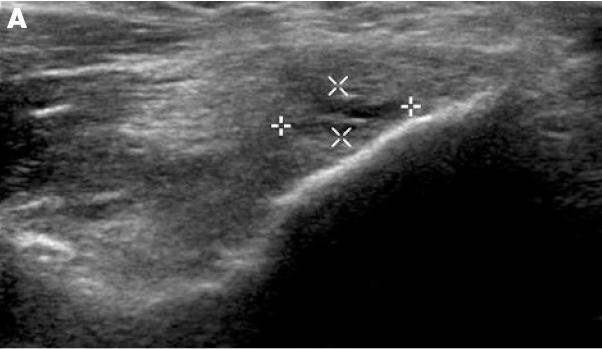
Mean pain duration was 23 months; US showed “showed structural tendon changes with hypo-echoic areas, and a vascularity, corresponding to the painful area”. It was in the extensor carpi radialis brevis origin.
Technique:
Polidocanol 10 mg/ml (Aethoxyskerol 1%)– a cursory look on the net found a Canadian supplier at:
http://www.omegalaboratory.com/eng/order_form.asp
0.7 X50 mm2 needle – well, 20 gauge has an inner diameter of 0.64mm so the stuff must be pretty thick..
2 cc syringe – I might have to settle for a 3cc – do not try this without a leur lock or you may be more than just red faced…
sitting with arm resting at shoulder height on a table
elbow 70-80 degrees flexed resting pronated
Site US from top to find hypervascularity; needle by necessity entering from side parallel to surface of bone.
Injections in increments until all blood vessels were closed – took between 0.4-1 ml total.

This is my pathetic drawing of their US color view of the “vasculo-neural growth”. The view is the lateral epicondyle – where does one inject? Could be all over it – but remember the affected areas are tender so if you have dilute local in, you might be able to tell if you got it all if it goes numb (would be interested in what the authors think)
At 8 months, Visual Analog Pain scale went from 75 to 34/100, grip improved and patient satisfaction was 83%.
In a study, you cannot contaminate it by doing other measures, but I suspect more improvement could have been realized by treating other issues:
1) Supinator “radial tunnel” syndrome – extension of middle finger and resisted supination might be painful. Unlike what people are taught, the most susceptible radial nerve bifurcation can occur lower than the 1.3 cm below anterior radial head and could be up to 3 cm below the radial head.
YC Loh, Journal of Orthopaedic Surgery 2004;12(1):83–86 A new clinical test for radial tunnel syndrome—the Rule-of-Nine test: A cadaveric study
One German author went as far as to say :
Handchir Mikrochir Plast Chir. 2004 Aug;36(4):241-5
[About the problem of radial tunnel syndrome or “where does the tennis elbow end and where does the radial tunnel syndrome begin?”]
Smola C. Praxis fur ambulante Handchirurgie, Oldenburg.
Tennis elbow or epicondylitis lateralis humeri is a commonly seen pain-syndrome. Radial tunnel syndrome is generally assumed to be a rare nerve compression syndrome. This study intents to demonstrate that tennis elbow is the most common manifestation of radial tunnel syndrome or in other words, tennis elbow is nothing else but radial tunnel syndrome. In patients with tennis elbow one will always find the ramus profundus n. radialis compressed by the arcade of Frohse. The author is convinced that following the carpal tunnel syndrome, the radial tunnel syndrome is the second most common nerve compression in upper extremity.
I have not always found that, but the supinator does become spastic/trigger activated in some cases and if left untreated will develop a life of its own with superficial radial nerve irritation.
2) Spinal level problem – doesn’t take much to find they are tender over the lower neck on the effected side and in other triggers on the way up corresponding to a particular nerve root. Dr. C. Gunn originally called this “Pre -Spondylosis” but with the severity of pain, distribution of triggers and in some cases edema and tropic changes ( and now the vasculo-neural changes), it is also likely a form of Neurogenic Inflammation. In neurogenic inflammation, nerve damage cause the usually inputting sensory nerves to upchuck irritating compounds backwards into the damaged tissues – glutamate, Substance P, and calcitonin gene-related peptide particularly with tennis elbow.
Dr. Gunn found the paraspinous dorsal rami fed muscles become spastic and need treatment in addition to the triggers that the neurogenic inflammation creates down the arm. He did the impossible – he took WCB patients with tennis elbow and with work to paraspinous and distal trigger areas was able to obtain improvement:Can Med Assoc J. 1976 May 8;114(9):803-9.
Tennis elbow and the cervical spine.
Gunn CC, Milbrandt WE.
The exact cause of tennis elbow, a common condition, is still obscure. While the condition may well be entirely due to a local disorder at the elbow, the results of a study of 50 patients whose condition was resistant to 4 weeks of treatment directed to the elbow suggest that the underlying condition may have been (at least in these patients) a reflex localization of pain from radiculopathy at the cervical spine. Clinical, radiologic and electromyographic findings supported this suggestion. The pain was demonstrated to be muscular tenderness, which was maximal and specific at motor points. Treatment directed to the cervical spine appeared to give relief in the majority of patients. The more resistant the condition, the more severe were the radiologic and electromyographic findings in the cervical spine.
I consider him a father of neurogenic inflammation. He understood that segmental trophic changes, edema (he uses a match to make impressions) and specific nerve distributed triggers were a subtle form of nerve damage and was not afraid to call it neuropathy in the face of much scorn at the time. He has received the Order of Canada for his work. I have had the privilege of training with him and find it is very much like watching Sherlock Holmes at work. Keen observation and knowing palpation can delineate a problem specifically and quickly and it is “awesome” to watch.
His research can be accessed at:
http://www.istop.org/mainresearch.htm
Re neck – One can at least use cervical traction, ultrasound to facets and massage to the triggers if nothing else is available.
ADDENDUM – a recent article found spinal manipulation reduced pain on lateral epicondyle at least immediately post manipulation:
Manipulative Physiol Ther. 2008 Nov-Dec;31(9):675-81.
Immediate hypoalgesic and motor effects after a single cervical spine manipulation in subjects with lateral epicondylalgia. Fernández-Carnero J, Fernández-de-las-Peñas C, Cleland JA
—-
In regard to achilles tendonitis, the sclerosing authors found :
Knee Surg Sports Traumatol Arthrosc (2003) 11 : 339–343
Lars Öhberg Håkan Alfredson
Sclerosing therapy in chronic Achilles tendon insertional pain-results of a pilot study
In this case, the Polidocanol was diluted to 5 mg/ml and 2-4 mls were injected so you will need a 5 ml syringe.
They mention the patients were pain free from the anesthesia so they must have mixed 1% 1:1 with local. They were allowed to go back to vigourous training 1 week after.
The blood vessels entered the achilles tendon anteriorly from a fat pad area. While monitoring form back, the needle is inserted medially ventrally to achilles where the retrocalcaneal buras adheres (side facing bones). They have had some mid-tendon abnormalities on the dorsal side (facing skin) that was painful and also injected. This would fit with Dr. Cyriax finding that the inflammation was mostly under the achilles tendon where it is hard to reach and deep friction.
In regards to patellar:
Knee Surg Sports Traumatol Arthrosc (2005) 13: 74–80
Hakan Alfredson Lars Oberg
Neovascularisation in chronic painful patellar tendinosis—promising results after sclerosing neovessels outside the tendon challenge the need for surgery
resistant cases –
12/15 satisfactory results – 3 failures still had vasculo-neuro densities
responders went from VAS 80/100 to 10/100
Polidocanol diluted to 5 mg/ml. 1-2 mls injected.
Injected on dorsal side (underneath side) while on ultrasound control
back to full workout after 2 weeks
Comment – now it becomes clear why Botox by itself cannot rid the problem:
Botulinum Toxin Injection in the Treatment of Tennis Elbow A Double-Blind, Randomized, Controlled, Pilot Study
M.J. Hayton
The Journal of Bone and Joint Surgery (American). 2005;87:503-507
found no effect but injected it 5 cm from the lateral epicondyle – too far for it to stop the neurogenic inflammation /neurovascularization locally. And maybe not the best drug for neurogenic inflammation anyway.
Early on, I feel that corticosteroid injection is key to success but will take out any supinator problems before dealing with lateral epicondyle. Another issue deals with whether there is any residual pains after a week – it is easy to miss a little spot of problem near the “rim” of the area – as seen from the drawing, it goes all over the lateral epicondyle – if not taken completely out then I presume the budding “vasculo-neural growths” grow back into the whole epicondyle. It has been Cyriax’s contention that if any residual is not re-injected that it has been a waste of time – and now that makes sense. Obviously, one has to look for related muscle triggers and neck problems to.
Another interesting finding is the reduction of pain with certain mobilizations:
Man Ther. 2001 Nov;6(4):205-12.
Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Vicenzino B, Paungmali A, Buratowski S, Wright A.
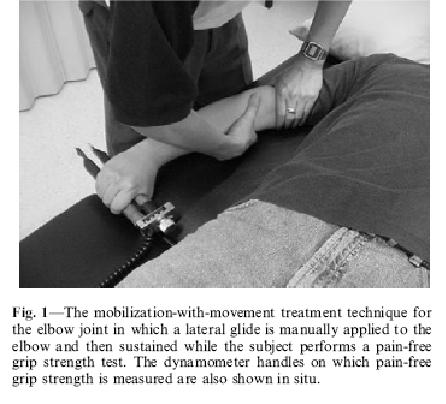
“using one hand to glide the proximal forearm laterally while the other hand fixed the distal end of the humerus (Fig. 1). The glide was applied and sustained while the subject performed the pain-free gripping action. The lateral glide was released after the subject had completed the pain- free grip exercise. Six repetitions were performed with a 15 second rest interval between repetitions”
It is facilitated by patient tightly gripping something in hand at time.
This resulted in rapid pain relief and increased grip strength. Done wrong, however, the maneuver can make things worse.
Addendums:
1) Sclerosant not superior to Lidocaine with epineprine if either injected in the tennis elbow vein plexus under ultrasound control:
Br J Sports Med. 2008 Apr;42(4):267-71. Epub 2008 Jan 23.
Pain relief after intratendinous injections in patients with tennis elbow: results of a randomised study. Zeisig E, Fahlström M, Ohberg L, Alfredson H
- polidocanol (10 mg/ml) or lidocaine hydrochloride (10 mg/ml) plus epinephrine (5 mg/ml) 0.5 ml
- 0.7650 mm needle connected to a 2-ml syringe
- position in area of blood flow as seen by Ultrasound and inject – blood flow should disappear
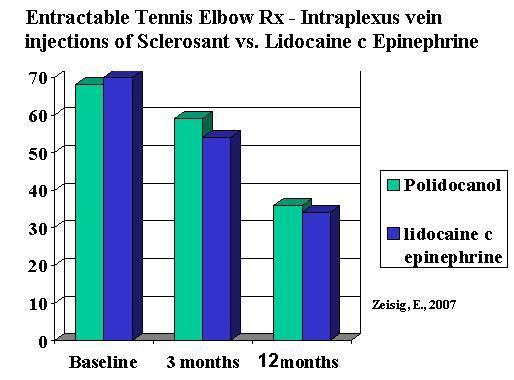
50 – 62% satisfied after 3 months. Those in the lidocaine with epinephrine group that were not satisfied, received sclerosant with benefit with 80% satisfaction.
Comment – another one shot wonder!! If additional injection helped failures why not give additional injections well before 3 months? If all you are targeting is the venous plexus, then maybe consider using small needles like those used in varicose veins cosmetic work. The lidocaine with epinephrine could go through a 32 gauge needle and hurt much less. I injected a case under Ultrasound ‘control” and found the veins automatically cleared; I am not convinced Ultrasound is needed.
2) Blood injection. This one was done for refractory (12 months) MEDIAL epicondylitis (golfer’s elbow). I find these difficult to treat and more likely to have been referred from neck (lower triceps will also be very sore).
[BTW re medial eipcondylitis, steroid injection works for 3 weeks only in one study using 40 mg methylprednisone (They do not mention ANYWHERE if this was Depo-medrol or not but I’m assuming it is.The Journal of Bone and Joint Surgery 79:1648-52 (1997)The Efficacy of an Injection of Steroids for Medial Epicondylitis. A Prospective Study of Sixty Elbows*SHALOM STAHL, M.D. and TEDDY KAUFMAN, M.D., HAIFA, ISRAEL. Dr. Cyriax, one of the fathers of orthopaedic medicine, made it clear that in tennis elbow, if the pain was not all better in a week, it needed repetition. ANOTHER ONE SHOT WONDER!!!]
- Area focal tendinosis or tear seen on ultrasound:
 Interestingly, the neovascularization was there too:
Interestingly, the neovascularization was there too:
Technique: “2 ml of autologous blood was withdrawn from the contralateral antecubital fossa of the patient and 2 ml of bupivacaine was infiltrated along the surface of the tendon using a 23G needle. After a
few minutes to allow the anaesthetic to work, the needle tip was then positioned into the site of the maximum tendon injury and the tendon was dry needled to create fenestrations and so cause fibril disruption and internal bleeding. The autologous blood was then slowly injected into the site of tendinosis and fibril discontinuity.”
Results:
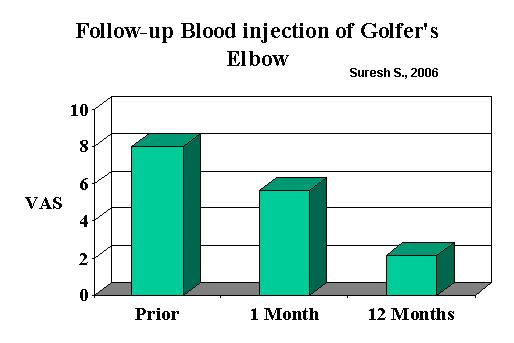
They felt it was the combination of the dry needling and blood injection that helped.
3) Injection of Platelet rich plasma:
Am J Sports Med. 2006 Nov;34(11):1774-8. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Mishra A, Pavelko T.
- “Fifty-five milliliters whole blood was collected from the uninvolved arm into a 60-mL syringe that contained 5 mL sodium citrate. “
- Centifuged – 5 mls platelet rich plasma obtained
- “The PRP was then buffered to physiologic pH using 8.4% sodium bicarbonate.”
- half was used for platelet counting; 2-3 mls was actually injected
- “Initially, bupivacaine with epinephrine was infiltrated into the skin and subcutaneous tissue of both groups as a
local field block. Approximately 0.5 mL was also injected directly into the area of maximum tenderness. Then, either 2 to 3 mL PRP or 2 to 3 mL bupivacaine with epinephrine was injected using a 22-g needle into the common extensor or flexor tendon using a peppering technique. This technique involved a single skin portal and then 5 penetrations of the tendon.”
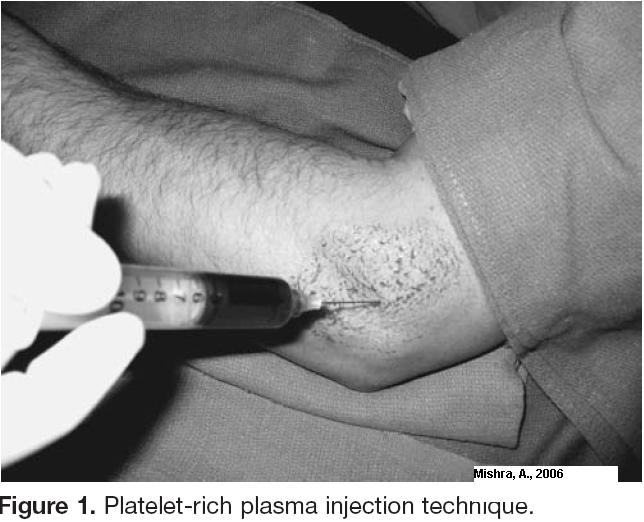
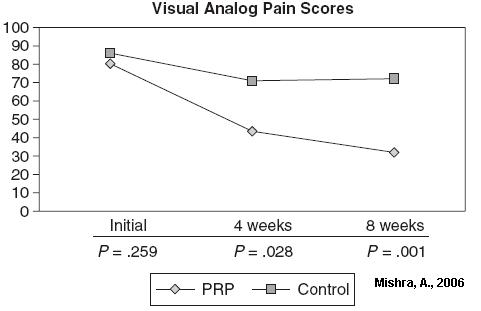
Comment – this is more like it – 50% relief in a month. Just how would one do this? The machine they used was not commercially available.
I would be interested in any pearls or comments on treating tennis elbow.

I found your blog via Google while searching for Back Neck Pain Pain and your post regarding Does Pain “Grow” at Tendon injury sites? looks very interesting to me. I always enjoy coming to this site because you offer great tips and advice for people like me who can always use a few good pointers. I will be getting my friends to pop around fairly soon.
Thanks for your feedback.
Disc Rim Lesions
It seems to me, neurovascular growth seems to be the key to discogenic pain as well. With disc damage, tears that occur in the annulus (outer rim). This outer rim can become inflamed because the disc center is actually foreign to the body and if it leaks out to the edge a brisk inflammatory reaction can ensue. If this rim faces the spine cord side, chronic back pain develops, much like a chronic tennis elbow. There is intense neurovascular growth there too – called a rim lesion. If the tear/ rim lesion faces one side near the spinal cord, then you can have typical sciatica (even reflex, strength and EMG changes) without any disc bulging/protrusion. This has now been dubbed “Chemical Radiculitis” and I feel occurs very often. This area of cracked rim can be seen one MRI but lots of people have this “Hyperintense Zone” without the accompaning inflammation so again MRI’s are more or less useless.
My 1/2 Red Neck Patient:
I had a patient with considerable pain unilaterally in the subcutaneous (skin fatty tissue) tissues of the neck. Picking up the tissues between my fingers was very tender. The most tender spots were areas the superficial dorsal nerves of the neck penetrated – upper cervical near midline at top and C3 somewhat lower 1-2 cm from middle. When I ran the same ultrasound imager the tennis elbow imaging study used, the blood vessels showed the same sort of pattern! Using a dumbed down sclerosant (concentrated dextrose) into these superficial tissues cleared those vessels on imaging, like in the tennis elbow study, and later afforded some relief. This skin relief was blunted by the fact he has significant other neck issues not so skin deep. What was interesting, was the red neck was unilateral on the side of his problems, so the thought of these neurovascular growths will always remind me of this red neck syndrome…
Micro nerve entrapments
Some of the pain in the red neck skin version represents in my mind, nerve microentrapments. I believe they are common contributor to low back pain in the form of cluneal nerve entrapments often seen above the iliac crest. Injecting them will help the pain for a while and can drop back pain by 2/10 for several weeks; but does not deal with the central issue that causes this neurogenic inflammation process. I find doing that helpful in post-laminectomy cases where the spinal sensitization and scar are things that are not fixed easily.
This is getting to be a hot topic as
– discs are being fried (IDET) and more recently injected with methylene blue in attempt to disable this rim lesion.
– Some skin microentrapments (trapezius tip, supraorbital) are now being surgically released – a group in Nebraska with Dr. Nystrom
– It is now clear why bulging disc and rim lesions are NOT accurate estimation of pain – they need to be inflammed. I have one lady with numbness mid fingers hand with a very postive Spurling sign – pressing on sidebend neck increases numbness = 92 – 100% accurate re radiculitis in neck. She has NO pain – so the disc can press but it takes the inflammation to make it hurt. She’s Irish – makes me wonder if some of the increased pain tolerance in Irish is due to lack of inflammatory response…
There is lots to talk about here – any discussion?
I found your blog via Google while searching for Treatment For Chronic Low Back Pain and your post regarding Does Pain “Grow” at Tendon injury sites? looks very interesting to me. I could not believe the amount of quality material on this site. The site is extremely eyecatching and pulls the reader straight it, the articles are great quality and are very professionally written. I have seen too many of these sites where it looks like they pay an 8 year old to do the writing – Not this one. Your site is easily the best that I have seen in a long while.
I found your blog via Google while searching for sciatica back pain and your post regarding Does Pain “Grow” at Tendon injury sites? looks very interesting to me.I just just wanted to drop you a note telling you how impressed I was with the information you have posted here. I also have websites & blogs so I know what I am talking about when I say your site is top-notch! Keep up the great work, you are providing a great resource on the Internet here!
Nice blog post discussing Does Pain “Grow” at Tendon injury sites?! I love this blog.
Notable view point in respect to Does Pain “Grow” at Tendon injury sites?. Your write ups is the reason I always drop by your blog.
Update on Neurovascular Lesion on tendons:
Knee Surg Sports Traumatol Arthrosc. 2008 Apr 17 [Epub ahead of print]
Marked sympathetic component in the perivascular innervation of the dorsal
paratendinous tissue of the patellar tendon in arthroscopically treated
tendinosis patients.
Danielson P, Andersson G, Alfredson H, Forsgren S.
The nerve component of this neurovascular pain fuzz is of Sympathetic nervous system origin – ie. This is the part of the nervous system activated in Complex Regional Pain Syndrome (CRPS aka RSD). Involvement of this part of the nervous system creates extreme allodynia (pain) and so it is not surprizing these areas are persistenatly painful.
Pingback: Pain Medical Musing » Blog Archive » Resistant Shoulder Tendonitis Treatments
I came across this article in my vague google search trying to
find any information that could describe my problem. After 5 months
of treatment, my general practitioner doctor and the physical
therapist are at a loss. I’m on worker’s compensation and they
are putting pressure on my doctor to send me back to work. I
change tires so he is hesitant. I’m afraid the insurance company
will eventually force him to release me and things will get worse.
I’ve been told I have lateral epicondylitis. After 8 wks of therapy, I was
given a cortisone shot. I stll have pain in both median and lateral area
of my forearm, an ache up the tricep area and the worst being in my
shouder at the base of my neck. The research discussed here seems
to describe most of my problem. I’ve got an appointment with my
doctor in 2 weeks and will either be sent back to work or to a hand
specialist. I plan on showing this article to him. Maybe it will help.
Thank you.
I also have websites & blogs so I know what I am talking about when I say your site is top-notch! Keep up the great work, you are providing a great resource on the Internet here!
Pingback: Pain Medical Musing » Blog Archive » Prolotherapy to Mid Tendon Achilles Tendonopathy - Only Mildly Better Results When Compared to Eccentric Loading Exercises - How Could That Be Better?
Pingback: Tissues Around Knee Contribute to Pains | Pain Medical Musing