DHEA and androgen levels are higher in PCO yet FM rates are 32.5% in PCO versus 7.7 in the general population.
The Frequency of Fibromyalgia Syndrome in Patients with Polycystic Ovary Syndrome.
Journal of Musculoskeletal Pain June 2010, Vol. 18, No. 2 , Pages 120-126
Feray Soyupek, MD Sedat Yildiz, MD Selami Akkus, MD Mehmet Guney, MD Muhittin Tamer Mungan, MD Sevilay Eris, MD abstract here
- 40 cases PCO; 39 controls
- FM rates 32.5% in PCO versus only 7.7% in controls
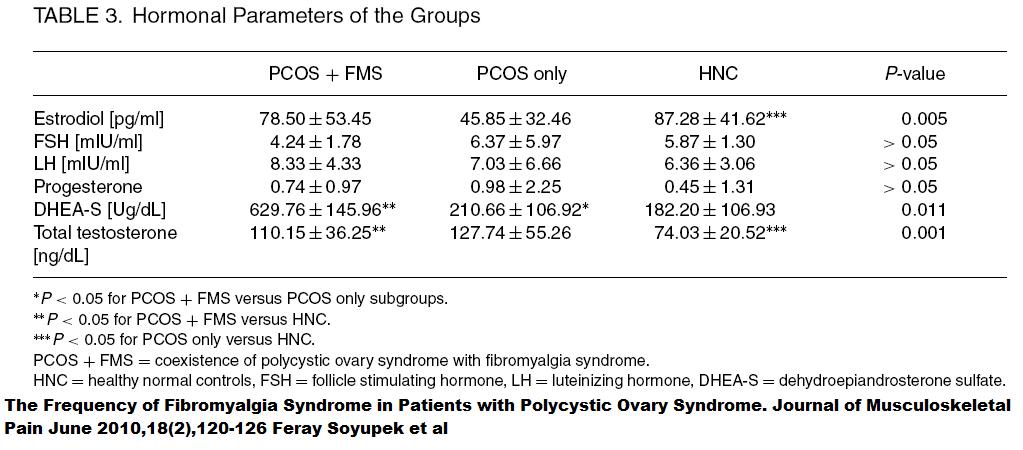
Hromonal Differences:
- To be fair, those with PCO and FM had lower androgen levels than those with PCO and NO FM – so androgens might have been some protective.
- High DHEA and low estrogen levels stand out in PCO plus FM group – suggesting high DHEA could be too much of a good thing…
- Much higher diffues pain, sleep disturbance, headaches, and fatigue were found in PCO plus FM versus PCO by self – as one would expect.
Addendum: Recent article on PCO finds it is a high cytokine disease:
The role of cytokines in polycystic ovarian syndrome
Krystle Ebejer, Jean Calleja-Agius
Gynecol Endocrinol, 2013; 29(6): 536–540
http://www.ncbi.nlm.nih.gov/pubmed/23368758
- Pro-inflammatory cytokines especially IL-18 are significantly higher in women with PCOS. Anti-inflammatory lipokine, adiponectin, is significantly reduced in PCO.
Contends that PCO is a cytokine disease fueled by:
-
- an altered immune response to microbial and inflammatory stimuli
obesity (60-70%) (though non-obese PCO cases still elevated IL-18 cytokines) – “significant increase in hs-CRP, IL-6 and TNF-a is mostly attributed to obesity”
- insulin resistance (50% -70%) – Higher levels IL-6 which is produced by adipose tissue and stimulates CRP production by the liver
- hypothalamic-pituitary ovarian dysfunction and anovulation – progestereone is an immune regulator; no ovulation – no progesterone
- High testosterone – Contends that hyperandrogenism increases mononuclear cell senstivity to glucose and hence causes glucose-induced inflammation which in turn leads to increased androgen production by ovarian theca cells – leading to viscous cycle. – most is pure science conjecture rather than relating inflammation to testosterone levels.
Comment -I am not buying idea high testosterone fuels cytokine inflammation. I still feel DHEA supplementation in FM could help mood if levels are low, and androgen supplementation could help pains, if levels are low. There can, however, be too much of a good thing, and this might suggest such.