http://ard.bmj.com/cgi/content/full/67/6/758
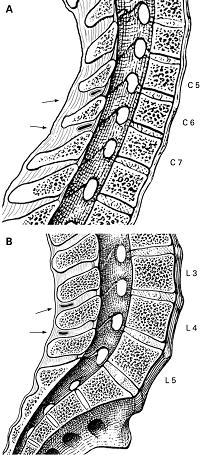
“Cervical interspinous bursae lie anteriorly in C6–C7 interspinous spaces (arrows). B. Median sagittal section through L3–L5 of the vertebral column. Lumbar interspinous bursae lie posteriorly in L3–L5 interspinous spaces (arrows).”
These are inflamed bursas between the posterior neck (and back) spines (the bumps on the spine you can feel. Not only will it heighten the suspicion of PMR, it should be treatable by local injection (in a hospital setting).
Ann Rheum Dis. 2008 Jun;67(6):758-61.
Cervical interspinous bursitis in active polymyalgia rheumatica. Salvarani C et al
It has been known for some time that various bursitis complaints can dog people with polymyalgia rheumatica. They state:
“Bilateral subacromial bursitis and trochanteric bursitis are the most frequent lesions and are present in most patients with PMR who have pain in the shoulder and pelvic girdles, respectively. ”
Hence this includes:
- Shoulder bursitis – sebdeltoid/subacromial and bicipital tenosynovitis (with or without joint involvement)
Salvarani C, Cantini F, Olivieri I, Barozzi L, MacchioniL, Niccoli L, et al. Proximal bursitis in active polymyalgia rheumatica. Ann Intern Med1997;127:27–31.Cantini F, Salvarani C, Olivieri I, Niccoli L, Padula A, Macchioni L, et al. Shoulder ultrasonography in the diagnosis of polymyalgia rheumatica: a case-control study. J Rheumatol 2001;28:1049–55. - Hip – trochanteric, iliopsoas and ischiogluteal bursitis
Cantini F, Niccoli L, Nannini C, Padula A, Olivieri I, Boiardi L, et al. Inflammatory changes of hip synovial
structures in polymyalgia rheumatica. Clin Exp Rheumatol 2005;23:462–8.
They suggest “PMR could be classified as an inflammatory process that primarily involves the extra-articular synovial structures.”
- In neck, often C6/7 but can occur at other levels except C1/2
- In back L4/5 is most affected though L3/4 can coexist. 85% of older people will have L4/5 one
- presence of calcifications would suggest psuedo-gout
- Causes episodic posterior neck pain,
- Worse by neck extension
- Diagnosed by its temporarily relief by injection of local anaesthetic.
Comment – sounds rare but worth considering in patients with localized pain on neck extension. Our college expects injections in neck to be done in a hospital setting. The addition of cortisone should shut that part of the PMR pain rapidly if prednisone did not do it. Its presence would heighten suspicion of polymyalgia rheumatica. 5-14% of cases can have a normal ESR
[quoted from:]
http://www.aafp.org/afp/20000815/789.htmlwhich means they will get NO respect from our rheumatologists. Bone scan could show the spots but how does one convince the rheumatologist steroids are an option?
I have lady in her 50’s that started with a peripheral neuropathy post chemotherapy then developed a steroid responsive component to her widespread pains (had steroids with couple episodes bronchitis – each time prednisone reduced pain 50%). Rheumatologist would not believe it was PMR but I could not wean her off prednisone. Managed to reduce it to 7.5 mg though 15 mg with flares. Is seeing a new rheumatologist out of town who will hopefully have ideas… Any suggestions?
