Early last year I wrote about my experience chronic severe abdominal pain as it being from the abdominal wall:
Chronic Severe Abdominal Pain is a Skin Nerve Pain
http://painmuse.org/?p=4840
Now, someone has taken it a step further by doing a widespread abdominal nerve block called the transversus abdominis plane (TAP) block – bilaterally if need be – and finds it generate significant pain relief. This could be a major milestone for abdominal pain relief.
Brings up the question of why it took so long to understand bad chronic abdominal pain could be part abdominal wall and treatable…
Pain Pract. 2018 Jan;18(1):48-52.
doi: 10.1111/papr.12580.
Efficacy of Transversus Abdominis Plane Steroid Injection for Treating Chronic Abdominal Pain.
Abd-Elsayed A et al.
https://www.ncbi.nlm.nih.gov/pubmed/28371274
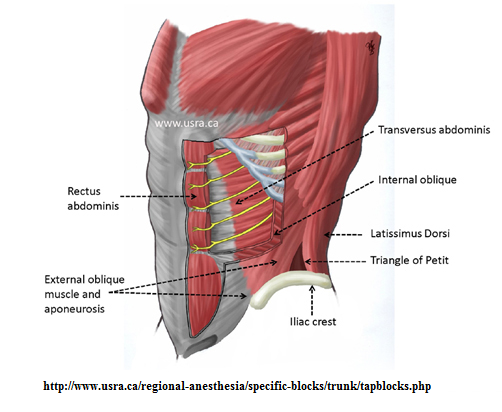
The block is relatively new to me so I included lots of pics:
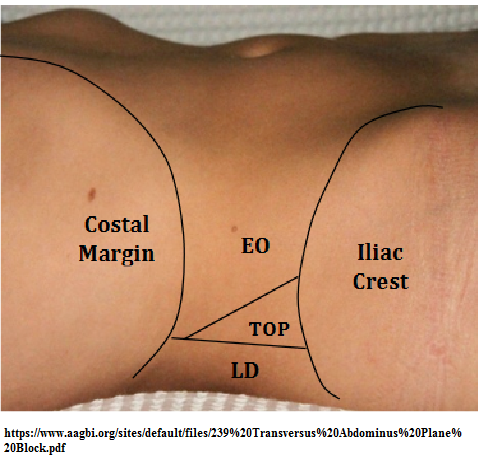
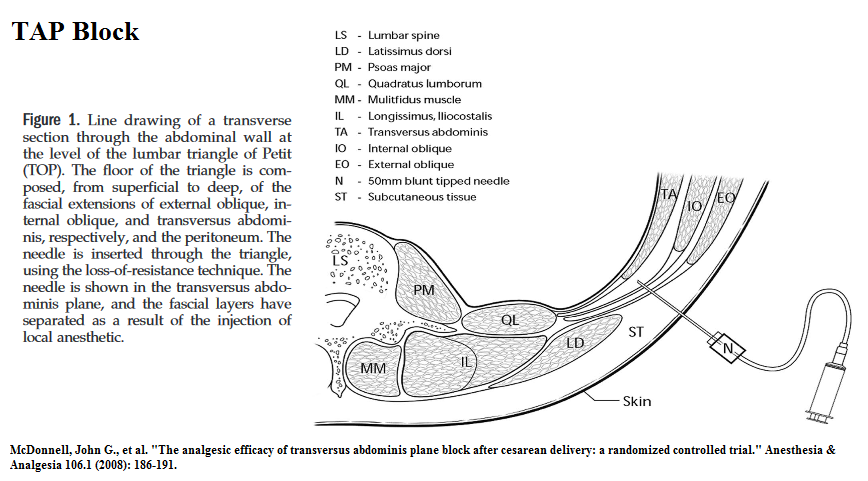
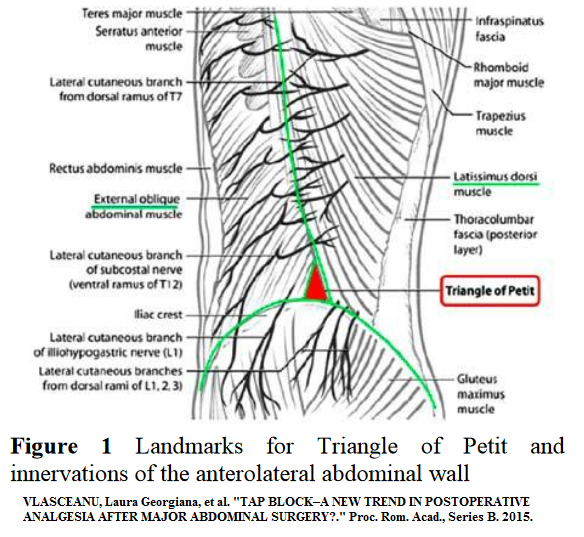
The block goes in at the “hole” over the iliac crest created by the end of the lattisimus dorsi and the beginning of the external oblique mid iliac crest
 palpate iliac crest
palpate iliac crest- behind the midaxillary line
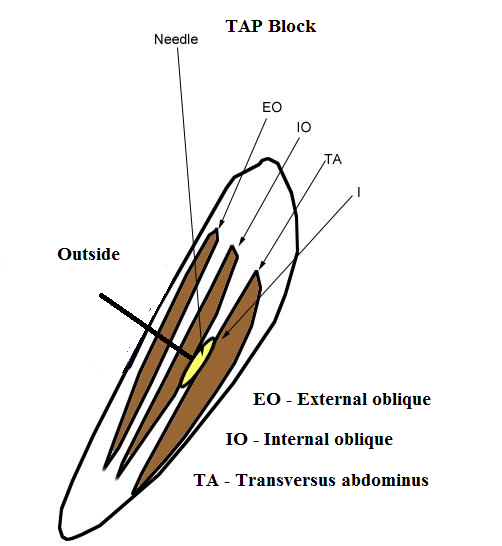
- using blunt regional needle – advanced at right angles – – pop sensation with external oblique then 2nd popthru internal oblique puts you in transversus abdominus plane
 A needle is inserted perpendicular to all planes, looking for a tactile endpoint of two pops. The first pop indicates penetration of the external oblique fascia and entry into the plane between external and internal oblique muscles; the second pop signifies entry into the TAP plane between internal oblique and transversus abdominis muscles.
A needle is inserted perpendicular to all planes, looking for a tactile endpoint of two pops. The first pop indicates penetration of the external oblique fascia and entry into the plane between external and internal oblique muscles; the second pop signifies entry into the TAP plane between internal oblique and transversus abdominis muscles.
 “The iliac crest was palpated from anterior to posterior until the latissimus dorsi muscle
“The iliac crest was palpated from anterior to posterior until the latissimus dorsi muscle
insertion was appreciated (Fig. 1). The triangle of Petit was palpated between the anterior border of latissimus dorsi, the posterior border of the external oblique, and the iliac crest. The skin over the triangle of Petit was pierced with the needle held at right angles to the coronal plane. The needle was stabilized and advanced at right angles to the skin in a coronal plane until resistance was encountered. This first resistance indicated that the needle tip was traversing the fascial extension of the external oblique muscle. Further
gentle advancement of the needle resulted in a loss of resistance, or “pop” sensation, as the needle entered the plane between the external and internal oblique fascial layers. Further gentle advancement resulted in the appreciation of a second increased resistance as the needle traversed the fascial extension of internal oblique. A second pop indicated entry into the transversus abdominis fascial plane. After careful aspiration to exclude vascular puncture, a test dose of 1 mL was injected. The presence of substantial resistance to this injection indicated that the needle was not between fascial planes, indicating the need to reposition the needle.”
 Nowadays done under ultrasound control.
Nowadays done under ultrasound control.
- 30 cases 2/3 female
- Abdominal; symptoms were low diarrhea – 5/30; constipation 2/30; nausea 7/30; vomiting 2/30
Procedure :
- freeze skin
- use bupivacaine 0.25% as not get motor block as with 0.5%
- unilateral blocks, 8 mL of bupivacaine 0.25% mixed with 80 mg of triamcinolone
- bilateral blocks, 9 mL of bupivacaine 0.25% and 40 mg of triamcinolone each side.
- used 22-gauge spinal needle on the syringe with US that could see spread
- The needle was flushed with lidocaine 1% and withdrawn. (nice touch)
- Spoiler issue: “Some blocks were performed at the subcostal level to treat high abdominal pain conditions.”
- 8 left; 12 right; 25 bilateral; some had more than 1 block
Results
- pain better in 79.5% of blocks but 20.5% were ineffective
- “improvement was 54.7% +/- 36.4% for a duration of 0 to 490 days”
- 2/44 got long lasting relief >450/days
- 1/5 got no response
- rest on average seem to have gotten about 2 months relief
Comment – last week at had a patient with only left sided abdominal pain. She had had dearly diverticultis at one point but had almost neuropathic pains left. I thought it might be a herpes zoster prodrome but treatment for that did not help. It looked like ilioinguinal neuralgia though a little high for it and I treated it with nerve block and perineural injections and it remitted temporarily. I saw her last week and it came back.
Having her lie with her bad side up, I could run 2 fingers down side of abdomen until reach level where sore and then inject between my 2 spread fingers needle pointing more medially than down. I could fan along course of nerve and hit it with 6 mls solution. Following, I found she still had some discomfort so I felt for the dorsal nerve root – they often come up right beside spinous process. Sure enough she was very tender as I pressed on side of spinous process and I injected local in the skin layers only. Following, she said she was “numb”.
I contend nerve block could be potentiated with 5-10% lidocaine if kept away from spine (a spinal block could cause hypotensive death).
I contend working the spinal level could help – superficial blocks of dorsal nerve root and I use a chiropractic activator on facet joints
I contend that the painful nerve tracts can be desensitized by repeat injection of D5W (perineural injection technique) every 2 cm or so along tract (easy to find tender tract by skin rolling) – if miss some of it just alternate space 2 cm outside where you injected until you get it all.
For bilateral cases, I suspect I would be lost if not for procedure developed here – Thank you Dr. Abd-Elsayed who by the way works at the:
Department of Anesthesiology, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin
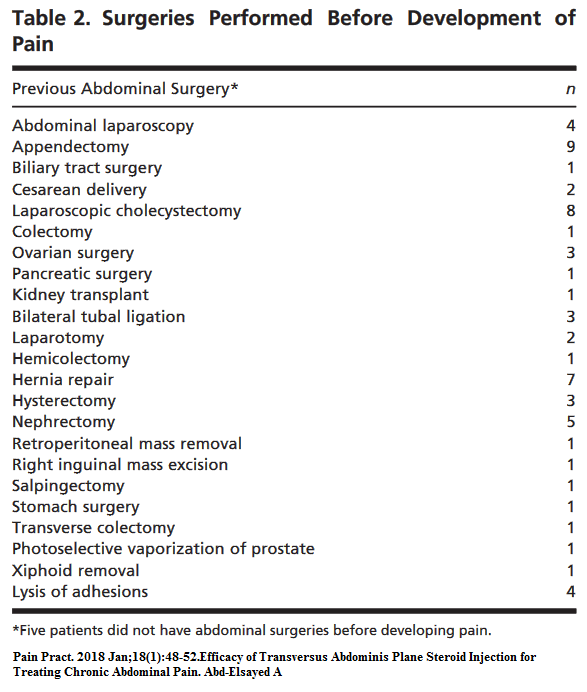
addendum – In same issue of Pain Practice a case series of chronic post surgical cases were given RAP blocks with benefit. Most were obvious abdominal wall nerve damage cases.
Transversus Abdominis Plane Block for the Diagnosis and Treatment of Chronic Abdominal Wall Pain Following Surgery: A Case Series
Marco Baciarello et al
Pain Practice 18(1), 2018 109–117
http://onlinelibrary.wiley.com/doi/10.1111/papr.12570/full
- Again demonstrating relief but highlighting how abdominal procedures can damage nerve – one pain was at the site of previous colostomy; another at the site of a drain, and so forth.
- Their cases had obvious neuropathic pain features (burning, paresthesias, high pain level).
- They used triamcinolone diacetate 40- 80 mgin 0.375% ropivacaine, 30 mL.
- Occasionally, they also infused it over a period of time so could get good relief -I think that is a smarter way to do things but not readily available in our country..
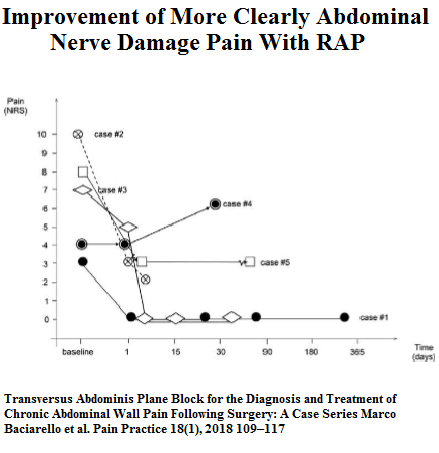 They gave up on one case with mesh neuroma lilke history because injection only lasted 1 week; I feel subject should have had a longer lasting alcohol injection into site. I’m going to include case into my new One-Shot-Wonder blog where I feel people fail to give adequate number shots
They gave up on one case with mesh neuroma lilke history because injection only lasted 1 week; I feel subject should have had a longer lasting alcohol injection into site. I’m going to include case into my new One-Shot-Wonder blog where I feel people fail to give adequate number shots
They’re from Italy so no quick referral for me…
Addendum:
Ali ME, Ali IM.
Defining an Opioid Sparing Treatment Pathway for Chronic Abdominal Pain of Somatic and Visceral Origin: A Case Series.
J Pain Palliat Care Pharmacother. 2021 Mar;35(1):43-47
https://pubmed.ncbi.nlm.nih.gov/33095081/
5 cases reduced chronic nonmalignant pain by 2/3rds